J Korean Med Sci.
2024 Apr;39(15):e143. 10.3346/jkms.2024.39.e143.
Outcomes of Concomitant Maze Procedure in Tricuspid Repair for Severe Tricuspid Regurgitation
- Affiliations
-
- 1Department of Thoracic and Cardiovascular Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Department of Thoracic and Cardiovascular Surgery, Dongsan Medical Center, Keimyung University School of Medicine, Daegu, Korea
- 3Biostatistics and Clinical Epidemiology Center, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 4Department of Thoracic and Cardiovascular Surgery, Incheon Sejong Hospital, Incheon, Korea
- KMID: 2555473
- DOI: http://doi.org/10.3346/jkms.2024.39.e143
Abstract
- Background
We aimed to analyze the impact of concomitant Maze procedure on the clinical and rhythm outcomes, and echocardiographic parameters in tricuspid repair for patients with severe tricuspid regurgitation (TR) and persistent atrial fibrillation (AF).
Methods
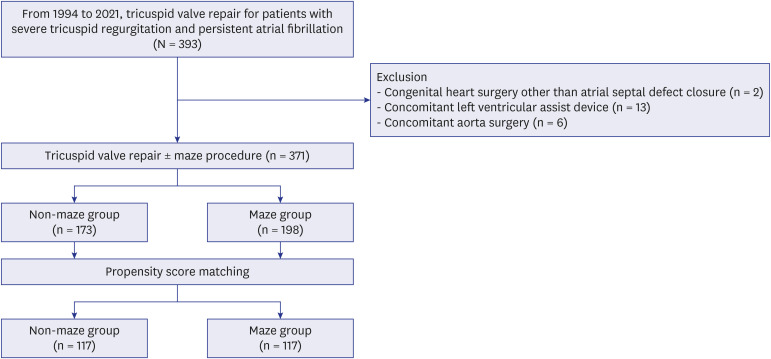
Patients who had severe TR and persistent AF and underwent tricuspid valve (TV) repair were included in the study. Both primary TR and secondary TR were included in the current study. The study population was stratified according to Maze procedure. The primary outcome was major adverse cardiovascular and cerebrovascular event (MACCE) at 15 years postsurgery. Propensity-score matching analyses was performed to adjust baseline differences.
Results
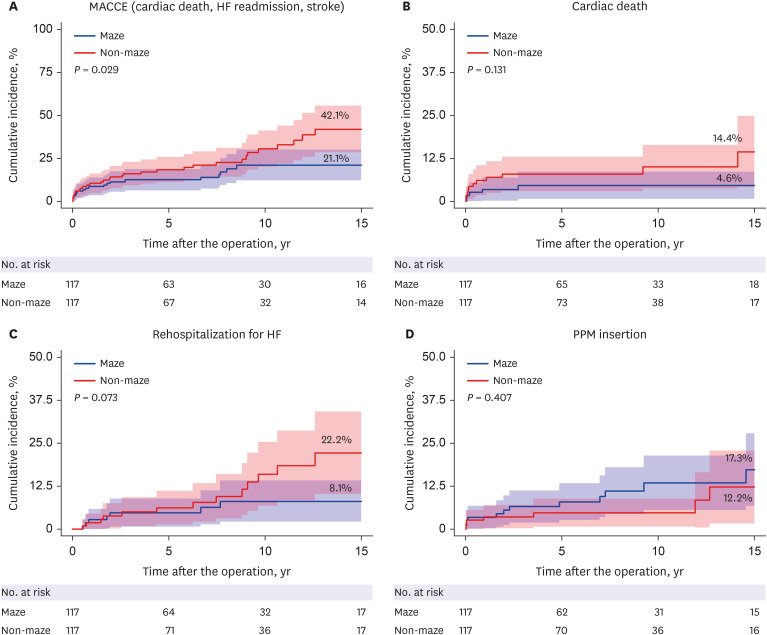
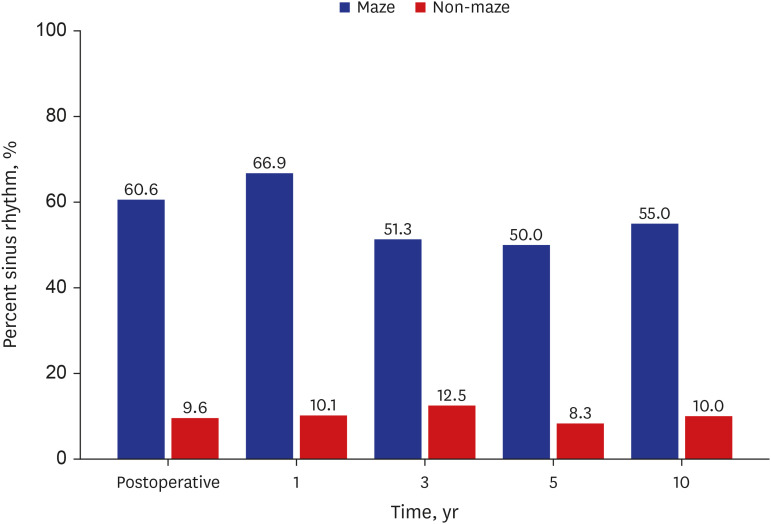
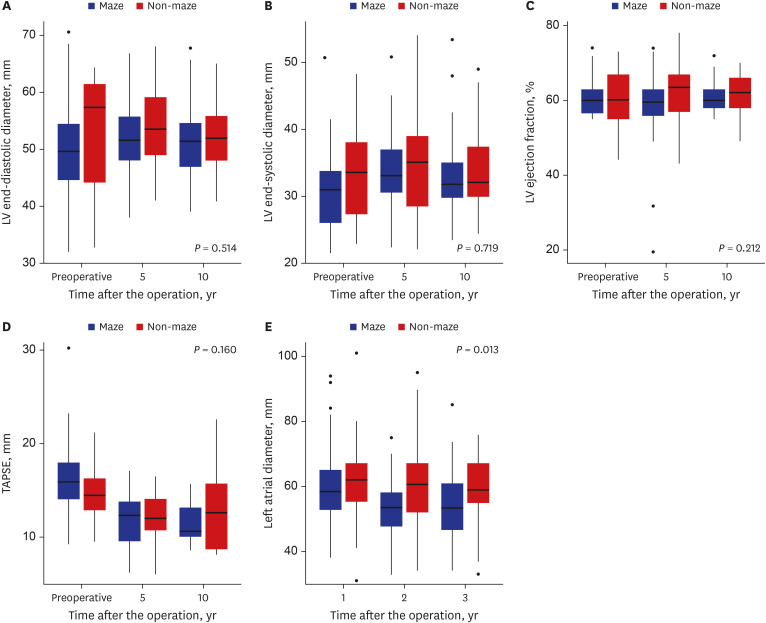
Three hundred seventy-one patients who underwent tricuspid repair for severe TR and persistent AF from 1994 to 2021 were included, and 198 patients (53.4%) underwent concomitant Maze procedure. The maze group showed 10-year sinus rhythm (SR) restoration rate of 55%. In the matched cohort, the maze group showed a lower cumulative incidence of cardiac death (4.6% vs. 14.4%, P = 0.131), readmission for heart failure (8.1% vs. 22.2%, P = 0.073), and MACCE (21.1% vs. 42.1%, P = 0.029) at 15 years compared to the non-maze group. Left atrial (LA) diameter significantly decreased in the maze group at 5 years (53.3 vs. 59.6 mm, P < 0.001) after surgery compared to preoperative level, and there was a significant difference in the change of LA diameter over time between the two groups (P = 0.013).
Conclusion
The Maze procedure during TV repair in patients with severe TR and persistent AF showed acceptable SR rates and lower MACCE rates compared to those without the procedure, while also promoting LA reverse remodeling.
Keyword
Figure
Reference
-
1. Suwalski P, Kowalewski M, Jasiński M, Staromłyński J, Zembala M, Widenka K, et al. Surgical ablation for atrial fibrillation during isolated coronary artery bypass surgery. Eur J Cardiothorac Surg. 2020; 57(4):691–700. PMID: 31665277.2. Henn MC, Lancaster TS, Miller JR, Sinn LA, Schuessler RB, Moon MR, et al. Late outcomes after the Cox maze IV procedure for atrial fibrillation. J Thorac Cardiovasc Surg. 2015; 150(5):1168–1176. 1178.e1–1178.e2. PMID: 26432719.3. Alfieri O, De Bonis M. Tricuspid valve surgery for severe tricuspid regurgitation. Heart. 2013; 99(3):149–150. PMID: 23236026.4. Bar N, Schwartz LA, Biner S, Aviram G, Ingbir M, Nachmany I, et al. Clinical outcome of isolated tricuspid regurgitation in patients with preserved left ventricular ejection fraction and pulmonary hypertension. J Am Soc Echocardiogr. 2018; 31(1):34–41. PMID: 29191730.5. Park I, Jeong DS, Park SJ, Ahn JH, Kim J, Kim EK, et al. Impact of maze procedure in patients with severe tricuspid regurgitation and persistent atrial fibrillation. J Thorac Cardiovasc Surg. 2023; 166(2):478–488.e5. PMID: 34872766.6. Marquis-Gravel G, Bouchard D, Perrault LP, Pagé P, Jeanmart H, Demers P, et al. Retrospective cohort analysis of 926 tricuspid valve surgeries: clinical and hemodynamic outcomes with propensity score analysis. Am Heart J. 2012; 163(5):851–858.e1. PMID: 22607864.7. Saran N, Dearani JA, Said SM, Greason KL, Pochettino A, Stulak JM, et al. Long-term outcomes of patients undergoing tricuspid valve surgery. Eur J Cardiothorac Surg. 2019; 56(5):950–958. PMID: 30919898.8. Bevan PJ, Haydock DA, Kang N. Long-term survival after isolated tricuspid valve replacement. Heart Lung Circ. 2014; 23(8):697–702. PMID: 24680484.9. Taramasso M, Gavazzoni M, Pozzoli A, Dreyfus GD, Bolling SF, George I, et al. Tricuspid regurgitation: predicting the need for intervention, procedural success, and recurrence of disease. JACC Cardiovasc Imaging. 2019; 12(4):605–621. PMID: 30947904.10. Hahn RT. Current transcatheter devices to treat functional tricuspid regurgitation with discussion of issues relevant to clinical trial design. Ann Cardiothorac Surg. 2017; 6(3):240–247. PMID: 28706866.11. Chang HW, Jeong DS, Cho YH, Sung K, Kim WS, Lee YT, et al. Tricuspid valve replacement vs. repair in severe tricuspid regurgitation. Circ J. 2017; 81(3):330–338. PMID: 28025464.12. Calkins H, Hindricks G, Cappato R, Kim YH, Saad EB, Aguinaga L, et al. 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation. Heart Rhythm. 2017; 14(10):e275–e444. PMID: 28506916.13. Cox JL, Churyla A, Malaisrie SC, Kruse J, Pham DT, Kislitsina ON, et al. When is a Maze procedure a Maze procedure? Can J Cardiol. 2018; 34(11):1482–1491. PMID: 30121148.14. Cox JL, Malaisrie SC, Kislitsina ON, McCarthy PM. The electrophysiologic basis for lesions of the contemporary Maze operation. J Thorac Cardiovasc Surg. 2019; 157(2):584–590. PMID: 30669224.15. Musharbash FN, Schill MR, Sinn LA, Schuessler RB, Maniar HS, Moon MR, et al. Performance of the Cox-maze IV procedure is associated with improved long-term survival in patients with atrial fibrillation undergoing cardiac surgery. J Thorac Cardiovasc Surg. 2018; 155(1):159–170. PMID: 29056264.16. Raikhelkar J, Lin HM, Neckman D, Afonso A, Scurlock C. Isolated tricuspid valve surgery: predictors of adverse outcome and survival. Heart Lung Circ. 2013; 22(3):211–220. PMID: 23103071.17. Wang TK, Mentias A, Akyuz K, Kirincich J, Crane AD, Popovic ZB, et al. Effect of tricuspid valve repair or replacement on survival in patients with isolated severe tricuspid regurgitation. Am J Cardiol. 2022; 162:163–169. PMID: 34903339.18. Kim HK, Kim YJ, Kim KI, Jo SH, Kim KB, Ahn H, et al. Impact of the maze operation combined with left-sided valve surgery on the change in tricuspid regurgitation over time. Circulation. 2005; 112(9):Suppl. I14–I19. PMID: 16159806.19. Yoo JS, Kim JB, Jung SH, Choo SJ, Chung CH, Lee JW. Impact of the maze procedure and postoperative atrial fibrillation on progression of functional tricuspid regurgitation in patients undergoing degenerative mitral repair. Eur J Cardiothorac Surg. 2013; 43(3):520–525. PMID: 22677351.20. Thomas L, Abhayaratna WP. Left atrial reverse remodeling: mechanisms, evaluation, and clinical significance. JACC Cardiovasc Imaging. 2017; 10(1):65–77. PMID: 28057220.21. Yu CM, Fang F, Zhang Q, Yip GW, Li CM, Chan JY, et al. Improvement of atrial function and atrial reverse remodeling after cardiac resynchronization therapy for heart failure. J Am Coll Cardiol. 2007; 50(8):778–785. PMID: 17707183.22. Kagawa Y, Fujii E, Fujita S, Ito M. Association between left atrial reverse remodeling and maintenance of sinus rhythm after catheter ablation of persistent atrial fibrillation. Heart Vessels. 2020; 35(2):239–245. PMID: 31346694.23. La Meir M, Gelsomino S, Lucà F, Pison L, Rao CM, Wellens F, et al. Improvement of left atrial function and left atrial reverse remodeling after minimally invasive radiofrequency ablation evaluated by 2-dimensional speckle tracking echocardiography. J Thorac Cardiovasc Surg. 2013; 146(1):72–77. PMID: 22713302.24. Thomas L, Muraru D, Popescu BA, Sitges M, Rosca M, Pedrizzetti G, et al. Evaluation of left atrial size and function: relevance for clinical practice. J Am Soc Echocardiogr. 2020; 33(8):934–952. PMID: 32762920.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Permanent Pacemaker Lead Induced Severe Tricuspid Regurgitation in Patient Undergoing Multiple Valve Surgery
- Repair of Posttraumatic Tricuspid Regurgitation Using Artificial Chordae and an Annuloplasty Ring
- Tricuspid Valve Repair for Tricuspid Valve Insufficiency Following a Cardiac Stab Injury
- Tricuspid Valve Re-Repair in Ebstein Anomaly Using the Cone Technique
- Successful Repair of Critical Tricuspid Regurgitation Secondary to a Ruptured Papillary Muscle in a Neonate