J Korean Med Sci.
2024 Apr;39(15):e139. 10.3346/jkms.2024.39.e139.
Current Status and Associated Factors of Post-Hemorrhagic Hydrocephalus in Infants of 22 to 28 Weeks Gestation With Severe Intraventricular Hemorrhage in Korea: A Nationwide Cohort Study
- Affiliations
-
- 1Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Cell and Gene Therapy Institute, Samsung Medical Center, Seoul, Korea
- 3Department of Clinical Research Design and Evaluation, Samsung Advanced Institute for Health Sciences & Technology (SAIHST), Sungkyunkwan University, Seoul, Korea
- 4Department of Health Sciences and Technology, Samsung Advanced Institute for Health Sciences & Technology (SAIHST), Sungkyunkwan University, Seoul, Korea
- 5Department of Pediatrics, Gangnam CHA Hospital, Seoul, Korea
- KMID: 2555471
- DOI: http://doi.org/10.3346/jkms.2024.39.e139
Abstract
- Background
Post-hemorrhagic hydrocephalus (PHH), a common complication of severe intraventricular hemorrhage (IVH) in very low birth weight (BW) infants, is associated with significant morbidity and poor neurological outcomes. The objective of this study was to assess the current status of PHH and analyze the risk factors associated with the necessity of treatment for PHH in infants born between 22 and 28 weeks of gestation, specifically those with severe IVH (grade 3 or 4).
Methods
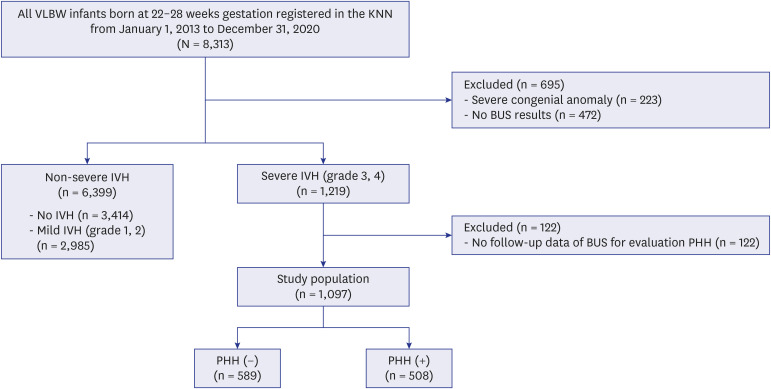
The analysis was conducted on 1,097 infants who were born between 22–28 gestational weeks and diagnosed with severe IVH, using data from the Korean Neonatal Network. We observed that the prevalence of PHH requiring treatment was 46.3% in infants with severe IVH.
Results
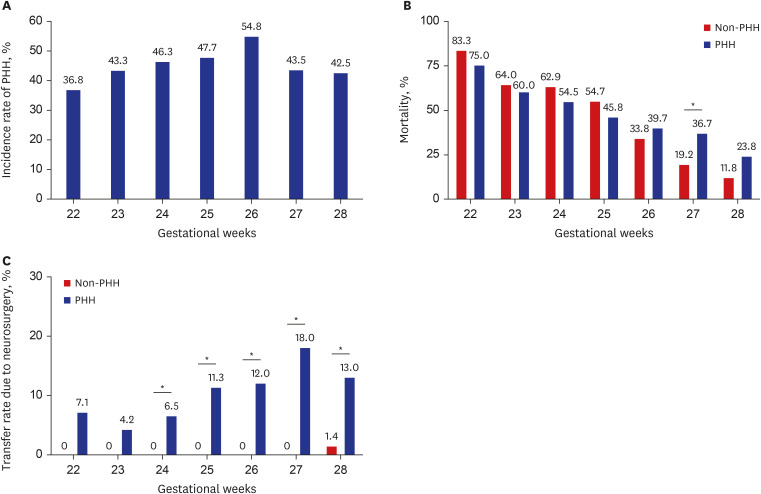
Higher rates of mortality, transfer during admission, cerebral palsy, and ventriculoperitoneal shunt after discharge were higher in infants with PHH than in those without PHH. PHH in severe IVH was associated with a higher rate of pulmonary hemorrhage, seizures, and IVH grade 4 in the entire cohort. In addition, it was associated with a lower rate of small for gestational age and chorioamnionitis. In the subgroup analysis, high BW, outborn status, pulmonary hemorrhage, seizure, sepsis, and IVH grade 4 were associated with a higher incidence of PHH between 22 and 25 gestational weeks (GW). In infants born between 26 and 28 GW, a higher incidence of PHH was associated with seizures and IVH grade 4.
Conclusion
It is necessary to maintain meticulous monitoring and neurological intervention for infants with PHH not only during admission but also after discharge. In addition, identifying the clinical factors that increase the likelihood of developing PHH from severe IVH is crucial.
Figure
Reference
-
1. Kazan S, Güra A, Uçar T, Korkmaz E, Ongun H, Akyuz M. Hydrocephalus after intraventricular hemorrhage in preterm and low-birth weight infants: analysis of associated risk factors for ventriculoperitoneal shunting. Surg Neurol. 2005; 64(Suppl 2):S77–S81. PMID: 16256848.2. Adams-Chapman I, Hansen NI, Stoll BJ, Higgins R. NICHD Research Network. Neurodevelopmental outcome of extremely low birth weight infants with posthemorrhagic hydrocephalus requiring shunt insertion. Pediatrics. 2008; 121(5):e1167–e1177. PMID: 18390958.3. Wilson-Costello D, Friedman H, Minich N, Fanaroff AA, Hack M. Improved survival rates with increased neurodevelopmental disability for extremely low birth weight infants in the 1990s. Pediatrics. 2005; 115(4):997–1003. PMID: 15805376.4. Shah PS, Lui K, Sjörs G, Mirea L, Reichman B, Adams M, et al. Neonatal outcomes of very low birth weight and very preterm neonates: an international comparison. J Pediatr. 2016; 177:144–152.e6. PMID: 27233521.5. Ahn SY, Shim SY, Sung IK. Intraventricular hemorrhage and post hemorrhagic hydrocephalus among very-low-birth-weight infants in Korea. J Korean Med Sci. 2015; 30 :Suppl 1. (Suppl 1):S52–S58. PMID: 26566358.6. Murphy BP, Inder TE, Rooks V, Taylor GA, Anderson NJ, Mogridge N, et al. Posthaemorrhagic ventricular dilatation in the premature infant: natural history and predictors of outcome. Arch Dis Child Fetal Neonatal Ed. 2002; 87(1):F37–F41. PMID: 12091289.7. Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978; 92(4):529–534. PMID: 305471.8. Afifi J, Shah PS, Ye XY, Shah V, Piedboeuf B, Barrington K, et al. Epidemiology of post-hemorrhagic ventricular dilatation in very preterm infants. J Perinatol. 2022; 42(10):1392–1399. PMID: 35945347.9. Klinger G, Osovsky M, Boyko V, Sokolover N, Sirota L, Lerner-Geva L, et al. Risk factors associated with post-hemorrhagic hydrocephalus among very low birth weight infants of 24-28 weeks gestation. J Perinatol. 2016; 36(7):557–563. PMID: 26938917.10. Lee SM, Chang YS, Park WS. Korean Neonatal Network. International Perspectives: Implementation of the Korean Neonatal Network. Neoreviews. 2019; 20(4):e177–e188. PMID: 31261059.11. Fenton TR, Kim JH. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 2013; 13(1):59. PMID: 23601190.12. Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L, et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg. 1978; 187(1):1–7. PMID: 413500.13. Behjati S, Emami-Naeini P, Nejat F, El Khashab M. Incidence of hydrocephalus and the need to ventriculoperitoneal shunting in premature infants with intraventricular hemorrhage: risk factors and outcome. Childs Nerv Syst. 2011; 27(6):985–989. PMID: 21234576.14. Gilard V, Chadie A, Ferracci FX, Brasseur-Daudruy M, Proust F, Marret S, et al. Post hemorrhagic hydrocephalus and neurodevelopmental outcomes in a context of neonatal intraventricular hemorrhage: an institutional experience in 122 preterm children. BMC Pediatr. 2018; 18(1):288. PMID: 30170570.15. Alan N, Manjila S, Minich N, Bass N, Cohen AR, Walsh M, et al. Reduced ventricular shunt rate in very preterm infants with severe intraventricular hemorrhage: an institutional experience. J Neurosurg Pediatr. 2012; 10(5):357–364. PMID: 22938077.16. Jin MC, Parker JJ, Rodrigues AJ, Ruiz Colón GD, Garcia CA, Mahaney KB, et al. Development of an integrated risk scale for prediction of shunt placement after neonatal intraventricular hemorrhage. J Neurosurg Pediatr. 2022; 29(4):444–453. PMID: 35090135.17. Kohelet D, Shochat R, Lusky A, Reichman B. Israel Neonatal Network. Risk factors for neonatal seizures in very low birthweight infants: population-based survey. J Child Neurol. 2004; 19(2):123–128. PMID: 15072105.18. Holste KG, Xia F, Ye F, Keep RF, Xi G. Mechanisms of neuroinflammation in hydrocephalus after intraventricular hemorrhage: a review. Fluids Barriers CNS. 2022; 19(1):28. PMID: 35365172.19. Hill A, Volpe JJ. Seizures, hypoxic-ischemic brain injury, and intraventricular hemorrhage in the newborn. Ann Neurol. 1981; 10(2):109–121. PMID: 7283398.20. Ogiwara H, Dipatri AJ Jr, Alden TD, Bowman RM, Tomita T. Endoscopic third ventriculostomy for obstructive hydrocephalus in children younger than 6 months of age. Childs Nerv Syst. 2010; 26(3):343–347. PMID: 19915853.21. Castejón OJ. Blood-brain barrier ultrastructural alterations in human congenital hydrocephalus and Arnold-Chiari malformation. Folia Neuropathol. 2009; 47(1):11–19. PMID: 19353430.22. Seyfert S, Becher A, Ohring R, Faulstich A. The permeability of the blood-CSF barrier in hydrocephalus, polyradiculitis, and meningitis. J Neurol. 2004; 251(3):355–356. PMID: 15015021.23. Lin CY, Chang HY, Chang JH, Hsu CH, Jim WT, Peng CC, et al. The impact of small-for-gestational-age status on the outcomes in very-low-birth-weight (VLBW) premature infants: a prospective cohort study in Taiwan. Front Pediatr. 2023; 11:1209765. PMID: 37520047.24. Bartels DB, Kreienbrock L, Dammann O, Wenzlaff P, Poets CF. Population based study on the outcome of small for gestational age newborns. Arch Dis Child Fetal Neonatal Ed. 2005; 90(1):F53–F59. PMID: 15613577.25. Wu T, Wang Y, Xiong T, Huang S, Tian T, Tang J, et al. Risk factors for the deterioration of periventricular-intraventricular hemorrhage in preterm infants. Sci Rep. 2020; 10(1):13609. PMID: 32788671.26. Parodi A, Giordano I, De Angelis L, Malova M, Calevo MG, Preiti D, et al. Post-haemorrhagic hydrocephalus management: delayed neonatal transport negatively affects outcome. Acta Paediatr. 2021; 110(1):168–170. PMID: 33007123.27. Ichi S. Clinical feature and general management of post-hemorrhagic hydrocephalus in premature infants. J Korean Neurosurg Soc. 2023; 66(3):247–257. PMID: 37032482.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Fibrinolytic (Thrombolytic) Therapy for Post Intraventricular Hemorrhagic Hydrocephalus in Preterm Infants
- A Case of congenital hydrocephalus associated with fetal intraventricular hemorrhage
- Intraventricular Hemorrhage and Post Hemorrhagic Hydrocephalus among Very-Low-Birth-Weight Infants in Korea
- Clinical Feature and General Management of Post-Hemorrhagic Hydrocephalus in Premature Infants
- Temporary Surgical Management of Intraventricular Hemorrhage in Premature Infants