Acute Crit Care.
2024 Feb;39(1):117-126. 10.4266/acc.2023.00913.
Diagnostic accuracy of left ventricular outflow tract velocity time integral versus inferior vena cava collapsibility index in predicting post-induction hypotension during general anesthesia: an observational study
- Affiliations
-
- 1Department of Anaesthesia, Indira Gandhi Medical College Shimla, India
- KMID: 2555230
- DOI: http://doi.org/10.4266/acc.2023.00913
Abstract
- Background
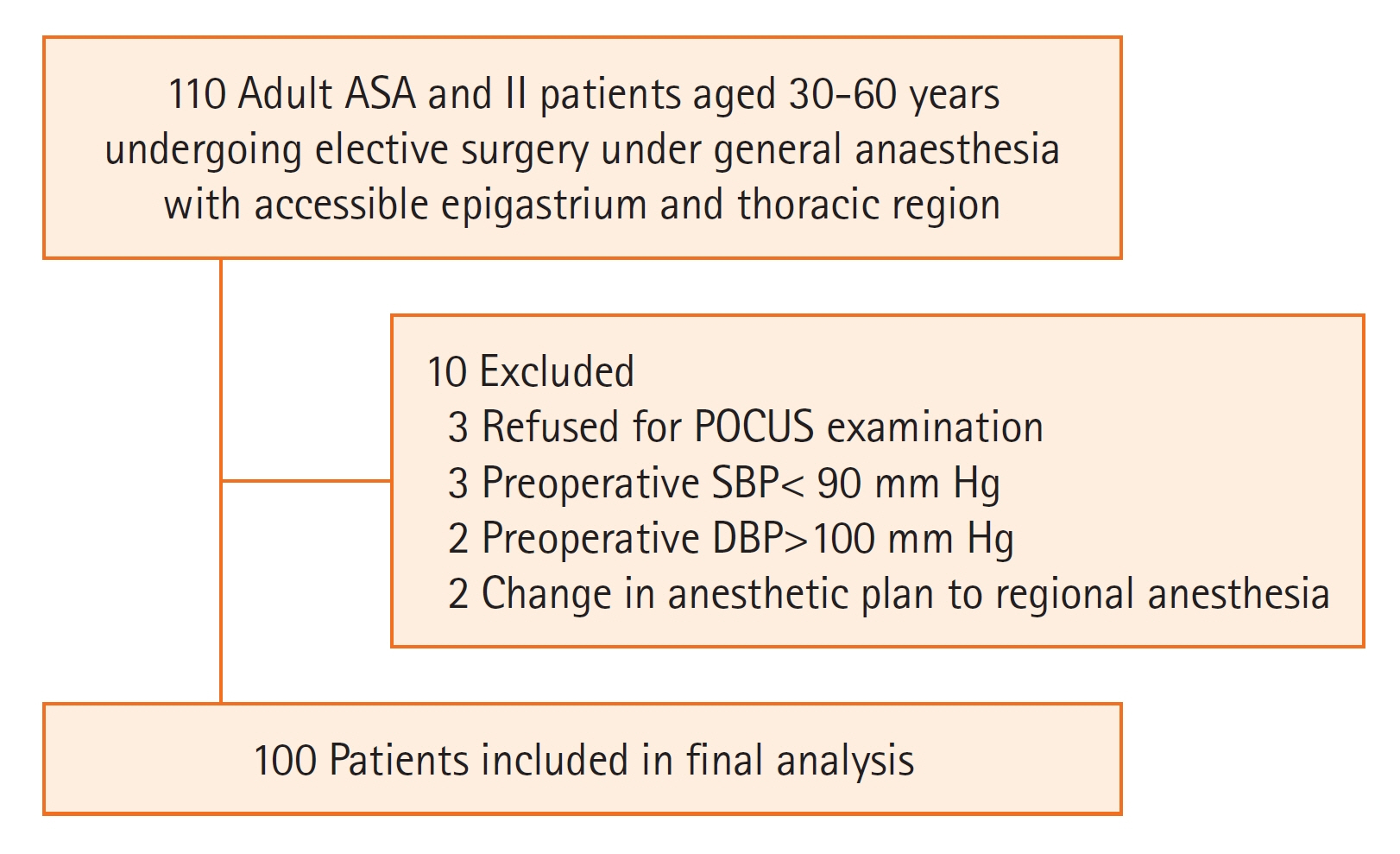
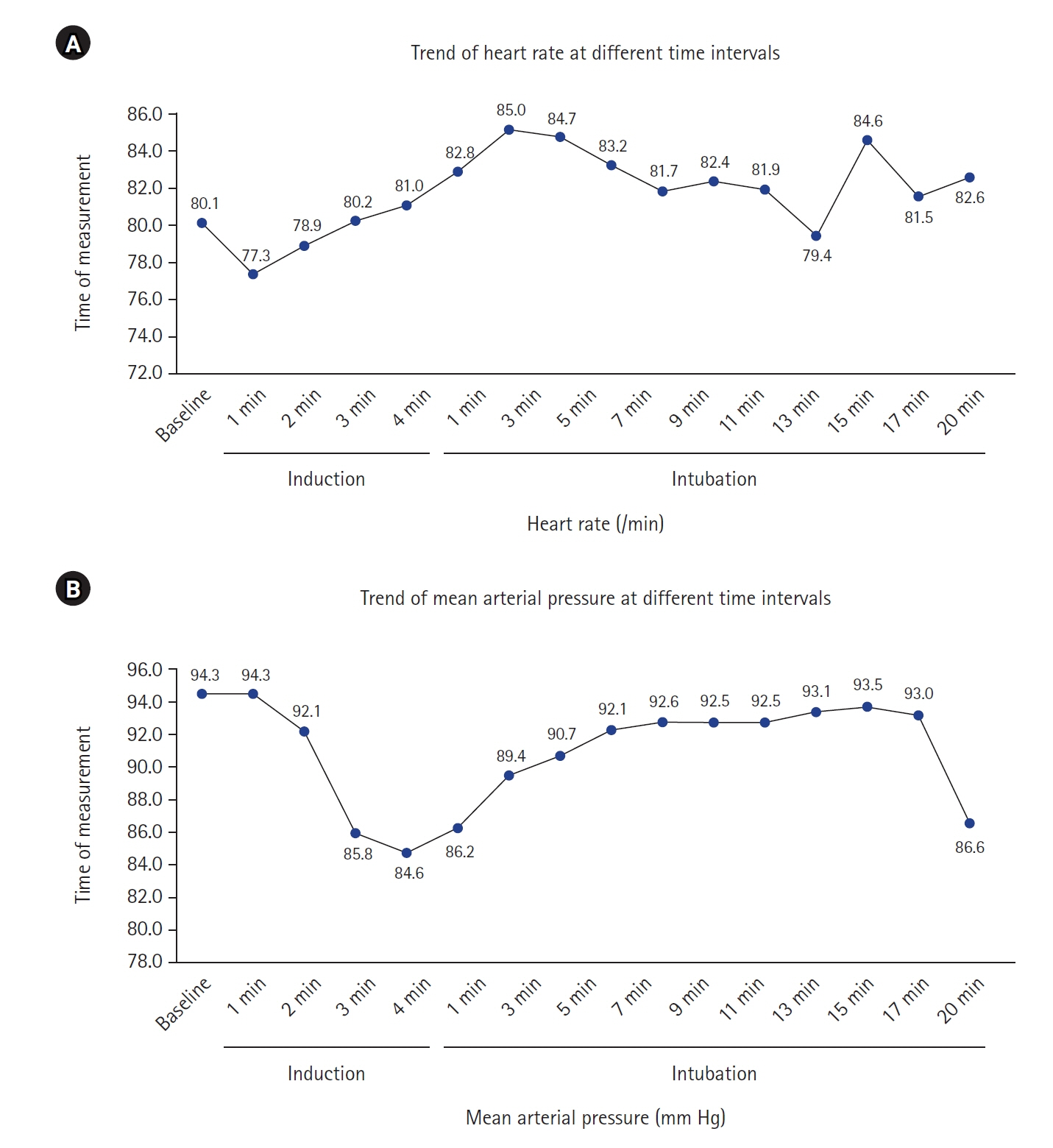
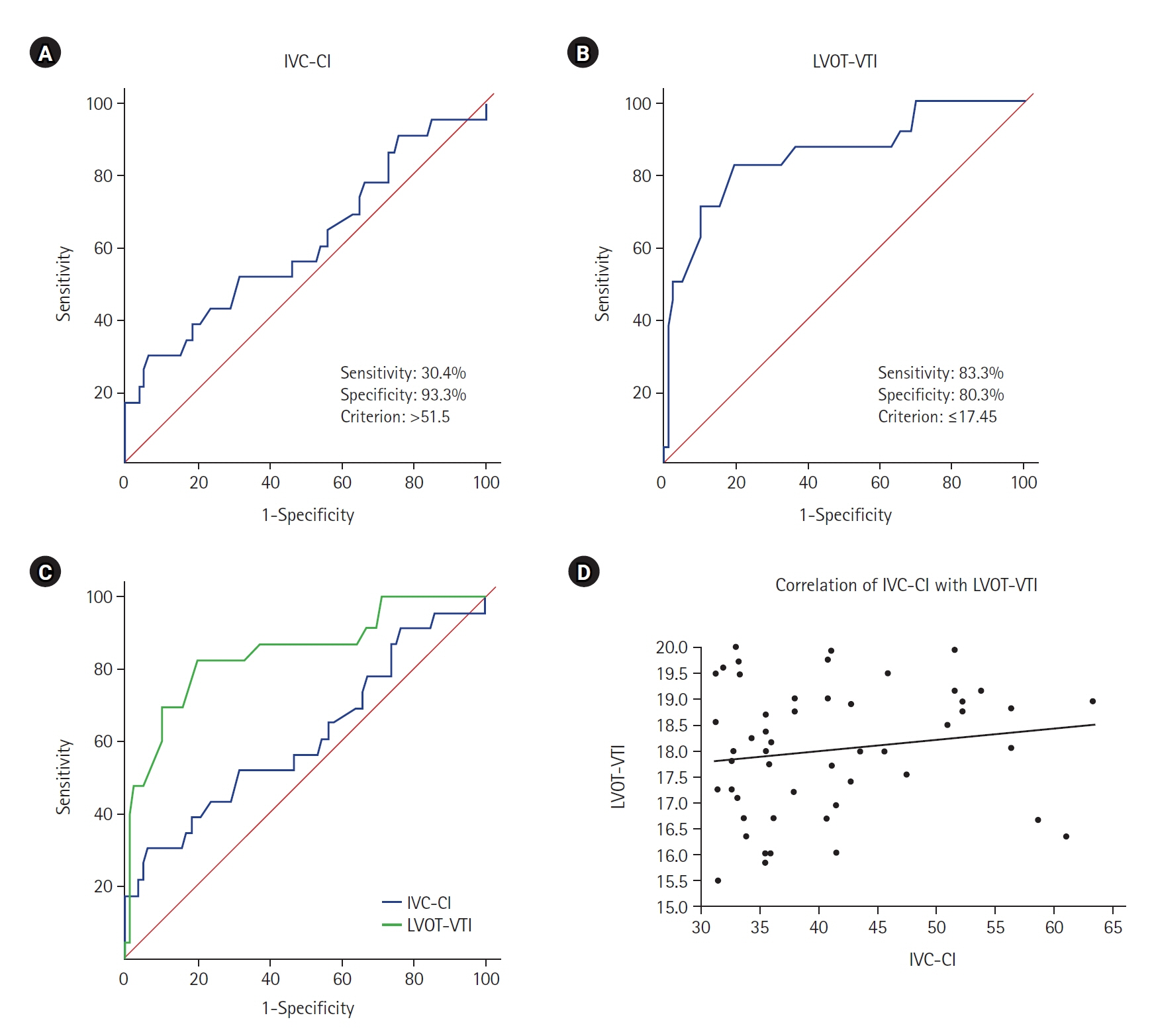
Point of care ultrasound (POCUS) is being explored for dynamic measurements like inferior vena cava collapsibility index (IVC-CI) and left ventricular outflow tract velocity time integral (LVOT-VTI) to guide anesthesiologists in predicting fluid responsiveness in the preoperative period and in treating post-induction hypotension (PIH) with varying accuracy. Methods: In this prospective, observational study on included 100 adult patients undergoing elective surgery under general anesthesia, the LVOT-VTI and IVC-CI measurements were performed in the preoperative room 15 minutes prior to surgery, and PIH was measured for 20 minutes in the post-induction period. Results: The incidence of PIH was 24%. The area under the curve, sensitivity, specificity, positive predictive value, negative predictive value, and diagnostic accuracy of the two techniques at 95% confidence interval was 0.613, 30.4%, 93.3%, 58.3%, 81.4%, 73.6% for IVC-CI and 0.853, 83.3%, 80.3%, 57.1%, 93.8%, 77.4% for LVOT-VTI, respectively. In multivariate analysis, the cutoff value for IVC-CI was >51.5 and for LVOT-VTI it was ≤17.45 for predicting PIH with odd ratio [OR] of 8.491 (P=0.025) for IVCCI and OR of 17.427 (P<0.001) for LVOT. LVOT-VTI assessment was possible in all the patients, while 10% of patients were having poor window for IVC measurements. Conclusions: We recommend the use of POCUS using LVOT-VTI or IVC-CI to predict PIH, to decrease the morbidity of patients undergoing surgery. Out of these, we recommend LVOT-VTI measurements as it has showed a better diagnostic accuracy (77.4%) with no failure rate.
Keyword
Figure
Reference
-
1. Kalagara H, Coker B, Gerstein NS, Kukreja P, Deriy L, Pierce A, et al. Point-of-care ultrasound (POCUS) for the cardiothoracic anesthesiologist. J Cardiothorac Vasc Anesth. 2022; 36:1132–47.
Article2. Spencer KT, Kimura BJ, Korcarz CE, Pellikka PA, Rahko PS, Siegel RJ. Focused cardiac ultrasound: recommendations from the American Society of Echocardiography. J Am Soc Echocardiogr. 2013; 26:567–81.
Article3. Südfeld S, Brechnitz S, Wagner JY, Reese PC, Pinnschmidt HO, Reuter DA, et al. Post-induction hypotension and early intraoperative hypotension associated with general anaesthesia. Br J Anaesth. 2017; 119:57–64.
Article4. Jor O, Maca J, Koutna J, Gemrotova M, Vymazal T, Litschmannova M, et al. Hypotension after induction of general anesthesia: occurrence, risk factors, and therapy: a prospective multicentre observational study. J Anesth. 2018; 32:673–80.
Article5. Blanco P. Rationale for using the velocity-time integral and the minute distance for assessing the stroke volume and cardiac output in point-of-care settings. Ultrasound J. 2020; 12:21.
Article6. Desai N, Garry D. Assessing dynamic fluid-responsiveness using transthoracic echocardiography in intensive care. BJA Educ. 2018; 18:218–26.
Article7. Benes J, Kirov M, Kuzkov V, Lainscak M, Molnar Z, Voga G, et al. Fluid therapy: double-edged sword during critical care? Biomed Res Int. 2015; 2015:729075.
Article8. Reich DL, Hossain S, Krol M, Baez B, Patel P, Bernstein A, et al. Predictors of hypotension after induction of general anesthesia. Anesth Analg. 2005; 101:622–8.
Article9. Aissaoui Y, Jozwiak M, Bahi M, Belhadj A, Alaoui H, Qamous Y, et al. Prediction of post-induction hypotension by point-of-care echocardiography: a prospective observational study. Anaesth Crit Care Pain Med. 2022; 41:101090.
Article10. Wang J, Zhou D, Gao Y, Wu Z, Wang X, Lv C. Effect of VTILVOT variation rate on the assessment of fluid responsiveness in septic shock patients. Medicine (Baltimore). 2020; 99:e22702.
Article11. Szabó M, Bozó A, Darvas K, Horváth A, Iványi ZD. Role of inferior vena cava collapsibility index in the prediction of hypotension associated with general anesthesia: an observational study. BMC Anesthesiol. 2019; 19:139.
Article12. Zhang J, Critchley LA. Inferior vena cava ultrasonography before general anesthesia can predict hypotension after induction. Anesthesiology. 2016; 124:580–9.
Article13. Airapetian N, Maizel J, Alyamani O, Mahjoub Y, Lorne E, Levrard M, et al. Does inferior vena cava respiratory variability predict fluid responsiveness in spontaneously breathing patients? Crit Care. 2015; 19:400.
Article14. Singh Y, Anand RK, Gupta S, Chowdhury SR, Maitra S, Baidya DK, et al. Role of IVC collapsibility index to predict post spinal hypotension in pregnant women undergoing caesarean section: an observational trial. Saudi J Anaesth. 2019; 13:312–7.
Article15. Salama ER, Elkashlan M. Pre-operative ultrasonographic evaluation of inferior vena cava collapsibility index and caval aorta index as new predictors for hypotension after induction of spinal anaesthesia: a prospective observational study. Eur J Anaesthesiol. 2019; 36:297–302.
Article16. Dinh VA, Ko HS, Rao R, Bansal RC, Smith DD, Kim TE, et al. Measuring cardiac index with a focused cardiac ultrasound examination in the ED. Am J Emerg Med. 2012; 30:1845–51.
Article17. Hutchings SD, Rees PS. Trauma resuscitation using echocardiography in a deployed military intensive care unit. J Intensive Care Soc. 2013; 14:120–5.
Article18. Bergenzaun L, Gudmundsson P, Öhlin H, Düring J, Ersson A, Ihrman L, et al. Assessing left ventricular systolic function in shock: evaluation of echocardiographic parameters in intensive care. Crit Care. 2011; 15:R200.
Article19. Nega MH, Ahmed SA, Tawuye HY, Mustofa SY. Incidence and factors associated with post-induction hypotension among adult surgical patients: prospective follow-up study. Int J Surg Open. 2022; 49:100565.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of hemiazygos continuation of a left inferior vena cava
- Effect of Changes of Inferior Vena Cava Diameter on Left Ventricular Hypertrophy in Hemodialysis Patients
- Pseudoaneurysm of Surgically Reconstructed Right Ventricular Outflow Tract Complicated by Superior Vena Cava Syndrome
- Left Ventricular Metastasis From Renal Cell Carcinoma Causing Left Ventricular Outflow Tract Obstruction
- A Case of Persistent Left Superior Vena Cava with Interruption of Inferior Vena Cava