Acute Crit Care.
2024 Feb;39(1):78-90. 10.4266/acc.2023.00416.
Effectiveness of massage and range of motion exercises on muscle strength and intensive care unit-acquired weakness in Iranian patients with COVID-19: a randomized parallel-controlled trial
- Affiliations
-
- 1Pistachio Safety Research Center, Rafsanjan University of Medical Sciences, Rafsanjan, Iran
- 2Clinical Research Development Unit, Ali-Ibn Abi-Talib Hospital, Rafsanjan University of Medical Sciences, Rafsanjan, Iran
- 3College of Nursing, Al-Kitab University, Kirkuk, Iraq
- 4Student Research Committee, Razi Faculty of Nursing and Midwifery, Kerman University of Medical Sciences, Kerman, Iran
- 5Nursing Research Center, Kerman University of Medical Sciences, Kerman, Iran
- 6Department of Critical Care, Faculty of Nursing and Midwifery, Kerman University of Medical Sciences, Kerman, Iran
- KMID: 2555226
- DOI: http://doi.org/10.4266/acc.2023.00416
Abstract
- Background
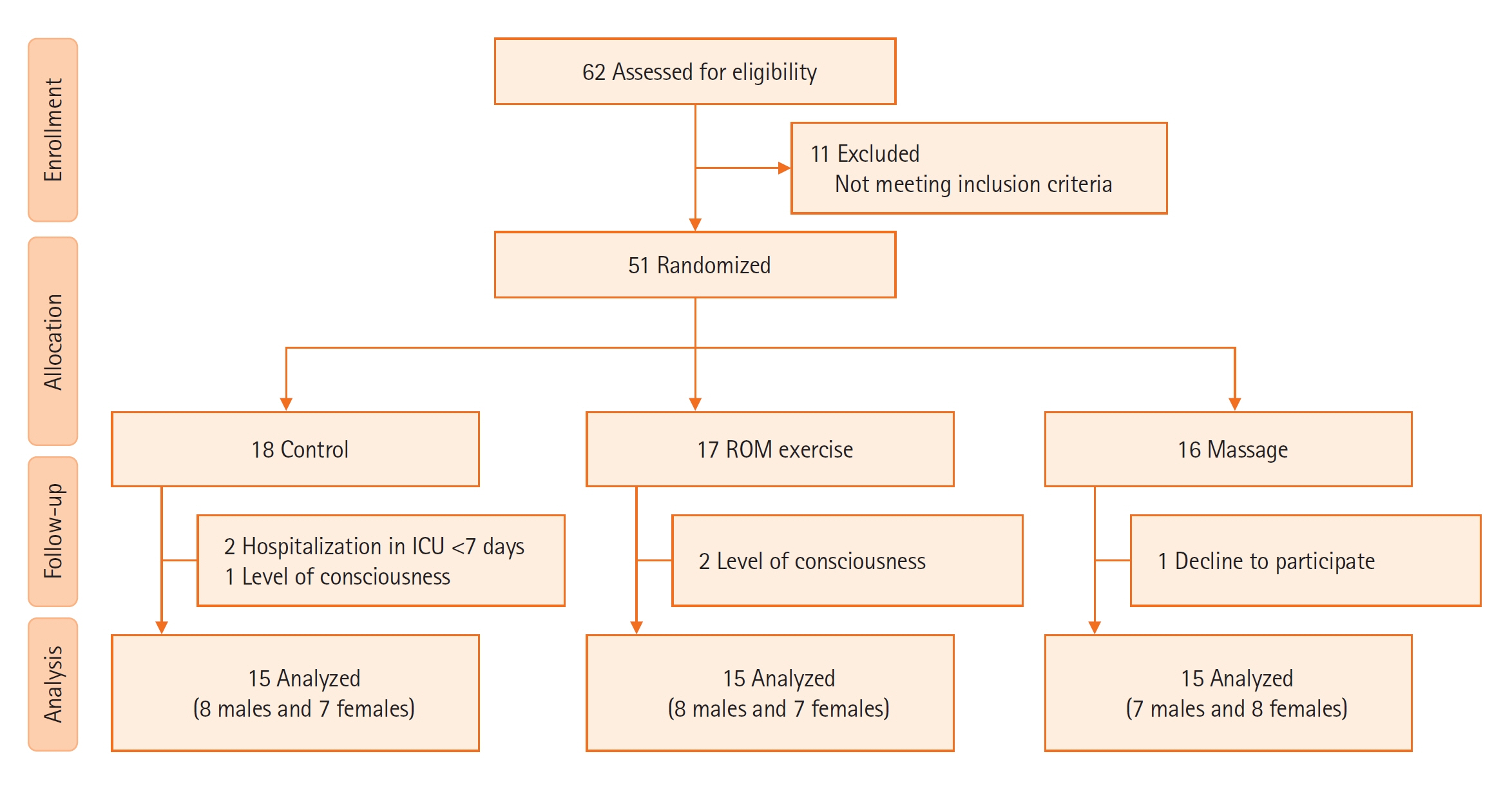
Muscle weakness is prevalent in intensive care patients. This study focused on comparing the effects of massage and range of motion (ROM) exercises on muscle strength and intensive care unit-acquired weakness (ICU-AW) among patients with coronavirus disease 2019 (COVID-19). Methods: This study was a randomized clinical trial that recruited patients (n=45) with COVID-19 admitted to the ICU and divided them into three groups (ROM exercises, massage, and control). We evaluated muscle strength and ICU-AW in the arms and legs using a hand dynamometer. The Medical Research Council sum score was determined before and after the intervention. Results: The study findings were that 0%, 20%, and 100% of the participants in the ROM exercises, massage, and control groups had ICU-AW on the 7th day of ICU admission. The ROM exercise group had greater muscle strength in the hands and legs than the massage and control groups, and the massage group had greater muscle strength than the control group. Conclusions: Massage and ROM exercises could improve muscle strength and reduce ICU-AW in COVID-19 patients admitted to the ICU.
Keyword
Figure
Reference
-
1. Zakeri MA, Hossini Rafsanjanipoor SM, Sedri N, Kahnooji M, Sanji Rafsanjani M, Zakeri M, et al. Psychosocial status during the prevalence of COVID-19 disease: the comparison between healthcare workers and general population. Curr Psychol. 2021; 40:6324–32.
Article2. Abbas J, Mubeen R, Iorember PT, Raza S, Mamirkulova G. Exploring the impact of COVID-19 on tourism: transformational potential and implications for a sustainable recovery of the travel and leisure industry. Curr Res Behav Sci. 2021; 2:100033.
Article3. Shoib S, Gaitán Buitrago JE, Shuja KH, Aqeel M, de Filippis R, Abbas J, et al. Suicidal behavior sociocultural factors in developing countries during COVID-19. Encephale. 2022; 48:78–82.
Article4. Zhou Y, Draghici A, Abbas J, Mubeen R, Boatca ME, Salam MA. Social media efficacy in crisis management: effectiveness of non-pharmaceutical interventions to manage COVID-19 challenges. Front Psychiatry. 2022; 12:626134.
Article5. Li Z, Wang D, Abbas J, Hassan S, Mubeen R. Tourists’ health risk threats amid COVID-19 era: role of technology innovation, transformation, and recovery implications for sustainable tourism. Front Psychol. 2022; 12:769175.
Article6. Hossini Rafsanjanipoor SM, Zakeri MA, Dehghan M, Kahnooji M, Sanji Rafsanjani M, Ahmadinia H, et al. Iranian psychosocial status and its determinant factors during the prevalence of COVID-19 disease. Psychol Health Med. 2022; 27:30–41.
Article7. Zakeri MA, Hossini Rafsanjanipoor SM, Kahnooji M, Ghaedi Heidari F, Dehghan M. Generalized anxiety disorder during the COVID-19 outbreak in iran: the role of social dysfunction. J Nerv Ment Dis. 2021; 209:491–6.
Article8. Yoosefi Lebni J, Abbas J, Moradi F, Salahshoor MR, Chaboksavar F, Irandoost SF, et al. How the COVID-19 pandemic effected economic, social, political, and cultural factors: a lesson from Iran. Int J Soc Psychiatry. 2021; 67:298–300.
Article9. Su Z, McDonnell D, Wen J, Kozak M, Abbas J, Šegalo S, et al. Mental health consequences of COVID-19 media coverage: the need for effective crisis communication practices. Global Health. 2021; 17:4.
Article10. Su Z, McDonnell D, Cheshmehzangi A, Abbas J, Li X, Cai Y. The promise and perils of Unit 731 data to advance COVID-19 research. BMJ Glob Health. 2021; 6:e004772.
Article11. Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA. 2020; 323:1574–81.
Article12. Hodgson CL, Tipping CJ. Physiotherapy management of intensive care unit-acquired weakness. J Physiother. 2017; 63:4–10.
Article13. Connolly B, Thompson A, Douiri A, Moxham J, Hart N. Exercise-based rehabilitation after hospital discharge for survivors of critical illness with intensive care unit-acquired weakness: a pilot feasibility trial. J Crit Care. 2015; 30:589–98.
Article14. Thomas S, Mehrholz J. Health-related quality of life, participation, and physical and cognitive function of patients with intensive care unit-acquired muscle weakness 1 year after rehabilitation in Germany: the GymNAST cohort study. BMJ Open. 2018; 8:e020163.
Article15. Fattahi E, Solhi M, Abbas J, Kasmaei P, Rastaghi S, Pouresmaeil M, et al. Prioritization of needs among students of University of Medical Sciences: a needs assessment. J Educ Health Promot. 2020; 9:57.16. Aqeel M, Abbas J, Shuja KH, Rehna T, Ziapour A, Yousaf I, et al. The influence of illness perception, anxiety and depression disorders on students mental health during COVID-19 outbreak in Pakistan: a Web-based cross-sectional survey. Int J Hum Rights Healthc. 2021; 14:1–14.
Article17. David OB, Idowu O, Adeloye OO, Tosin O. COVID-19: intensive care acquired weakness, a possible challenge in patient recovery? Middle East J Appl Sci Technol. 2020; 3:1–6.18. Bolton CF. The discovery of critical illness polyneuropathy: a memoir. Can J Neurol Sci. 2010; 37:431–8.
Article19. Piva S, Fagoni N, Latronico N. Intensive care unit-acquired weakness: unanswered questions and targets for future research. F1000Res. 2019; 8:508.
Article20. Argov Z, Latronico N. Neuromuscular complications in intensive care patients. Handb Clin Neurol. 2014; 121:1673–85.
Article21. Fan E, Cheek F, Chlan L, Gosselink R, Hart N, Herridge MS, et al. An official American Thoracic Society Clinical Practice guideline: the diagnosis of intensive care unit-acquired weakness in adults. Am J Respir Crit Care Med. 2014; 190:1437–46.
Article22. Wieske L, Dettling-Ihnenfeldt DS, Verhamme C, Nollet F, van Schaik IN, Schultz MJ, et al. Impact of ICU-acquired weakness on post-ICU physical functioning: a follow-up study. Crit Care. 2015; 19:196.
Article23. Appleton R, Kinsella J. Intensive care unit-acquired weakness. Contin Educ Anaesth Crit Care Pain. 2012; 12:62–6.
Article24. Parry SM, Berney S, Granger CL, Koopman R, El-Ansary D, Denehy L. Electrical muscle stimulation in the intensive care setting: a systematic review. Crit Care Med. 2013; 41:2406–18.25. Lindgren L, Rundgren S, Winsö O, Lehtipalo S, Wiklund U, Karlsson M, et al. Physiological responses to touch massage in healthy volunteers. Auton Neurosci. 2010; 158:105–10.
Article26. Yosef-Brauner O, Adi N, Ben Shahar T, Yehezkel E, Carmeli E. Effect of physical therapy on muscle strength, respiratory muscles and functional parameters in patients with intensive care unit-acquired weakness. Clin Respir J. 2015; 9:1–6.
Article27. Kisner C, Colby LA. Therapeutic exercise: foundations and techniques. F.A. Davis Company;2012.28. Sullivan KM, Silvey DB, Button DC, Behm DG. Roller-massager application to the hamstrings increases sit-and-reach range of motion within five to ten seconds without performance impairments. Int J Sports Phys Ther. 2013; 8:228–36.29. Wollersheim T, Haas K, Wolf S, Mai K, Spies C, Steinhagen-Thiessen E, et al. Whole-body vibration to prevent intensive care unit-acquired weakness: safety, feasibility, and metabolic response. Crit Care. 2017; 21:9.
Article30. Patsaki I, Gerovasili V, Sidiras G, Karatzanos E, Mitsiou G, Papadopoulos E, et al. Effect of neuromuscular stimulation and individualized rehabilitation on muscle strength in Intensive Care Unit survivors: a randomized trial. J Crit Care. 2017; 40:76–82.
Article31. Field T. Massage therapy research review. Complement Ther Clin Pract. 2016; 24:19–31.
Article32. Imtiyaz S, Veqar Z, Shareef MY. To compare the effect of vibration therapy and massage in prevention of delayed onset muscle soreness (DOMS). J Clin Diagn Res. 2014; 8:133–6.
Article33. Kong PW, Chua YH, Kawabata M, Burns SF, Cai C. Effect of post-exercise massage on passive muscle stiffness measured using myotonometry: a double-blind study. J Sports Sci Med. 2018; 17:599–606.34. Alves da Silva T, Stripari Schujmann D, Yamada da Silveira LT, Caromano FA, Fu C. Effect of therapeutic Swedish massage on anxiety level and vital signs of intensive care unit patients. J Bodyw Mov Ther. 2017; 21:565–8.
Article35. MacSween A, Lorrimer S, van Schaik P, Holmes M, van Wersch A. A randomised crossover trial comparing Thai and Swedish massage for fatigue and depleted energy. J Bodyw Mov Ther. 2018; 22:817–28.
Article36. Candan SA, Elibol N, Abdullahi A. Consideration of prevention and management of long-term consequences of post-acute respiratory distress syndrome in patients with COVID-19. Physiother Theory Pract. 2020; 36:663–8.
Article37. Poussardin C, Oulehri W, Isner ME, Mertes PM, Collange O. In-ICU COVID-19 patients’ characteristics for an estimation in post-ICU rehabilitation care requirement. Anaesth Crit Care Pain Med. 2020; 39:479–80.
Article38. Rahiminezhad E, Zakeri MA, Dehghan M. Muscle strength/intensive care unit acquired weakness in COVID-19 and non-COVID-19 patients. Nurs Crit Care. 2022; Jul. 27. [Epub]. https://doi.org/10.1111/nicc.12830.
Article39. Rahiminezhad E, Sadeghi M, Ahmadinejad M, Mirzadi Gohari SI, Dehghan M. A randomized controlled clinical trial of the effects of range of motion exercises and massage on muscle strength in critically ill patients. BMC Sports Sci Med Rehabil. 2022; 14:96.
Article40. Dehghan M, Malakoutikhah A, Ghaedi Heidari F, Zakeri MA. The effect of abdominal massage on gastrointestinal functions: a systematic review. Complement Ther Med. 2020; 54:102553.
Article41. Bernheim A, Mei X, Huang M, Yang Y, Fayad ZA, Zhang N, et al. Chest CT findings in coronavirus disease-19 (COVID-19): relationship to duration of infection. Radiology. 2020; 295:200463.
Article42. Mardani R, Ahmadi Vasmehjani A, Zali F, Gholami A, Mousavi Nasab SD, Kaghazian H, et al. Laboratory parameters in detection of COVID-19 patients with positive RT-PCR; a diagnostic accuracy study. Arch Acad Emerg Med. 2020; 8:e43.43. Lebni JY, Toghroli R, Abbas J, Kianipour N, NeJhaddadgar N, Salahshoor MR, et al. Nurses’ work-related quality of life and its influencing demographic factors at a public hospital in Western Iran: a cross-sectional study. Int Q Community Health Educ. 2021; 42:37–45.
Article44. Azadi NA, Ziapour A, Lebni JY, Irandoost SF, Abbas J, Chaboksavar F. The effect of education based on health belief model on promoting preventive behaviors of hypertensive disease in staff of the Iran University of Medical Sciences. Arch Public Health. 2021; 79:69.
Article45. Abbas J, Aman J, Nurunnabi M, Bano S. The impact of social media on learning behavior for sustainable education: evidence of students from selected universities in Pakistan. Sustainability. 2019; 11:1683.
Article46. Watanabe S, Iida Y, Ito T, Mizutani M, Morita Y, Suzuki S, et al. Effect of early rehabilitation activity time on critically ill patients with intensive care unit-acquired weakness: a Japanese retrospective multicenter study. Prog Rehabil Med. 2018; 3:20180003.
Article47. Kisner C, Colby LA, Borstad J. Therapeutic exercise: foundations and techniques. 2017. F.A. Davis Company.48. Fritz S, Fritz LA. Mosby's fundamentals of therapeutic massage: e-book. Elsevier Health Sciences;2020.49. Su Z, McDonnell D, Li X, Bennett B, Šegalo S, Abbas J, et al. COVID-19 vaccine donations-vaccine empathy or vaccine diplomacy?: a narrative literature review. Vaccines (Basel). 2021; 9:1024.
Article50. Su Z, Wen J, Abbas J, McDonnell D, Cheshmehzangi A, Li X, et al. A race for a better understanding of COVID-19 vaccine non-adopters. Brain Behav Immun Health. 2020; 9:100159.
Article51. Aman J, Abbas J, Lela U, Shi G. Religious affiliation, daily spirituals, and private religious factors promote marital commitment among married couples: does religiosity help people amid the COVID-19 crisis? Front Psychol. 2021; 12:657400.
Article52. Su Z, McDonnell D, Abbas J, Shi L, Cai Y, Yang L. Secondhand smoke exposure of expectant mothers in China: factoring in the role of culture in data collection. JMIR Cancer. 2021; 7:e24984.
Article53. Hu Y, Hu X, Xiao J, Li D. Effect of early mobilization on the physical function of patients in intensive care unit: a meta-analysis. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2019; 31:458–63.54. Disser NP, De Micheli AJ, Schonk MM, Konnaris MA, Piacentini AN, Edon DL, et al. Musculoskeletal consequences of COVID-19. J Bone Joint Surg Am. 2020; 102:1197–204.
Article55. Thomas P, Baldwin C, Bissett B, Boden I, Gosselink R, Granger CL, et al. Physiotherapy management for COVID-19 in the acute hospital setting: clinical practice recommendations. J Physiother. 2020; 66:73–82.
Article56. Lau HM, Ng GY, Jones AY, Lee EW, Siu EH, Hui DS. A randomised controlled trial of the effectiveness of an exercise training program in patients recovering from severe acute respiratory syndrome. Aust J Physiother. 2005; 51:213–9.
Article57. Verceles AC, Wells CL, Sorkin JD, Terrin ML, Beans J, Jenkins T, et al. A multimodal rehabilitation program for patients with ICU acquired weakness improves ventilator weaning and discharge home. J Crit Care. 2018; 47:204–10.
Article58. Lindberg P, Schmitz C, Forssberg H, Engardt M, Borg J. Effects of passive-active movement training on upper limb motor function and cortical activation in chronic patients with stroke: a pilot study. J Rehabil Med. 2004; 36:117–23.
Article59. Baroni BM, Pompermayer MG, Cini A, Peruzzolo AS, Radaelli R, Brusco CM, et al. Full range of motion induces greater muscle damage than partial range of motion in elbow flexion exercise with free weights. J Strength Cond Res. 2017; 31:2223–30.
Article60. Weerapong P, Hume PA, Kolt GS. The mechanisms of massage and effects on performance, muscle recovery and injury prevention. Sports Med. 2005; 35:235–56.
Article61. Best TM, Hunter R, Wilcox A, Haq F. Effectiveness of sports massage for recovery of skeletal muscle from strenuous exercise. Clin J Sport Med. 2008; 18:446–60.
Article62. Behm DG, Blazevich AJ, Kay AD, McHugh M. Acute effects of muscle stretching on physical performance, range of motion, and injury incidence in healthy active individuals: a systematic review. Appl Physiol Nutr Metab. 2016; 41:1–11.
Article63. Hindle KB, Whitcomb TJ, Briggs WO, Hong J. Proprioceptive neuromuscular facilitation (PNF): its mechanisms and effects on range of motion and muscular function. J Hum Kinet. 2012; 31:105–13.
Article64. McNair PJ, Dombroski EW, Hewson DJ, Stanley SN. Stretching at the ankle joint: viscoelastic responses to holds and continuous passive motion. Med Sci Sports Exerc. 2001; 33:354–8.
Article65. Hermans G, Van den Berghe G. Clinical review: intensive care unit acquired weakness. Crit Care. 2015; 19:274.
Article66. Latronico N, Bolton CF. Critical illness polyneuropathy and myopathy: a major cause of muscle weakness and paralysis. Lancet Neurol. 2011; 10:931–41.
Article67. Chan KH, Farouji I, Abu Hanoud A, Slim J. Weakness and elevated creatinine kinase as the initial presentation of coronavirus disease 2019 (COVID-19). Am J Emerg Med. 2020; 38:1548.
Article68. Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020; 77:683–90.
Article69. Zhang H, Charmchi Z, Seidman RJ, Anziska Y, Velayudhan V, Perk J. COVID-19-associated myositis with severe proximal and bulbar weakness. Muscle Nerve. 2020; 62:E57–60.70. Bagnato S, Boccagni C, Marino G, Prestandrea C, D’Agostino T, Rubino F. Critical illness myopathy after COVID-19. Int J Infect Dis. 2020; 99:276–78.
Article71. Bakhru RN, Davidson JF, Bookstaver RE, Kenes MT, Welborn KG, Morris PE, et al. Physical function impairment in survivors of critical illness in an ICU recovery clinic. J Crit Care. 2018; 45:163–9.
Article72. Harvey NR, Stanton MP. Intensive care unit-acquired weakness: implications for case management. Prof Case Manag. 2017; 22:72–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Muscle Growth and Anabolism in Intensive Care Survivors (GAINS) trial: a pilot randomised controlled trial
- Early Mobilization and Rehabilitation of Critically-Ill Patients
- Effects of Plantar Flexor Muscle Static Stretching Alone and Combined With Massage on Postural Balance
- The Effect of Subacromial Massage for Hemiplegic Shoulder: Ramdomized Controlled Study
- Effectiveness of the Eye Care Protocol in the Intensive Care Unit Patients: A Randomized Controlled Trial