Acute Crit Care.
2024 Feb;39(1):61-69. 10.4266/acc.2022.01543.
Comparison of preoxygenation with a high-flow nasal cannula and a simple face mask before intubation in Korean patients with head and neck cancer
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2555224
- DOI: http://doi.org/10.4266/acc.2022.01543
Abstract
- Background
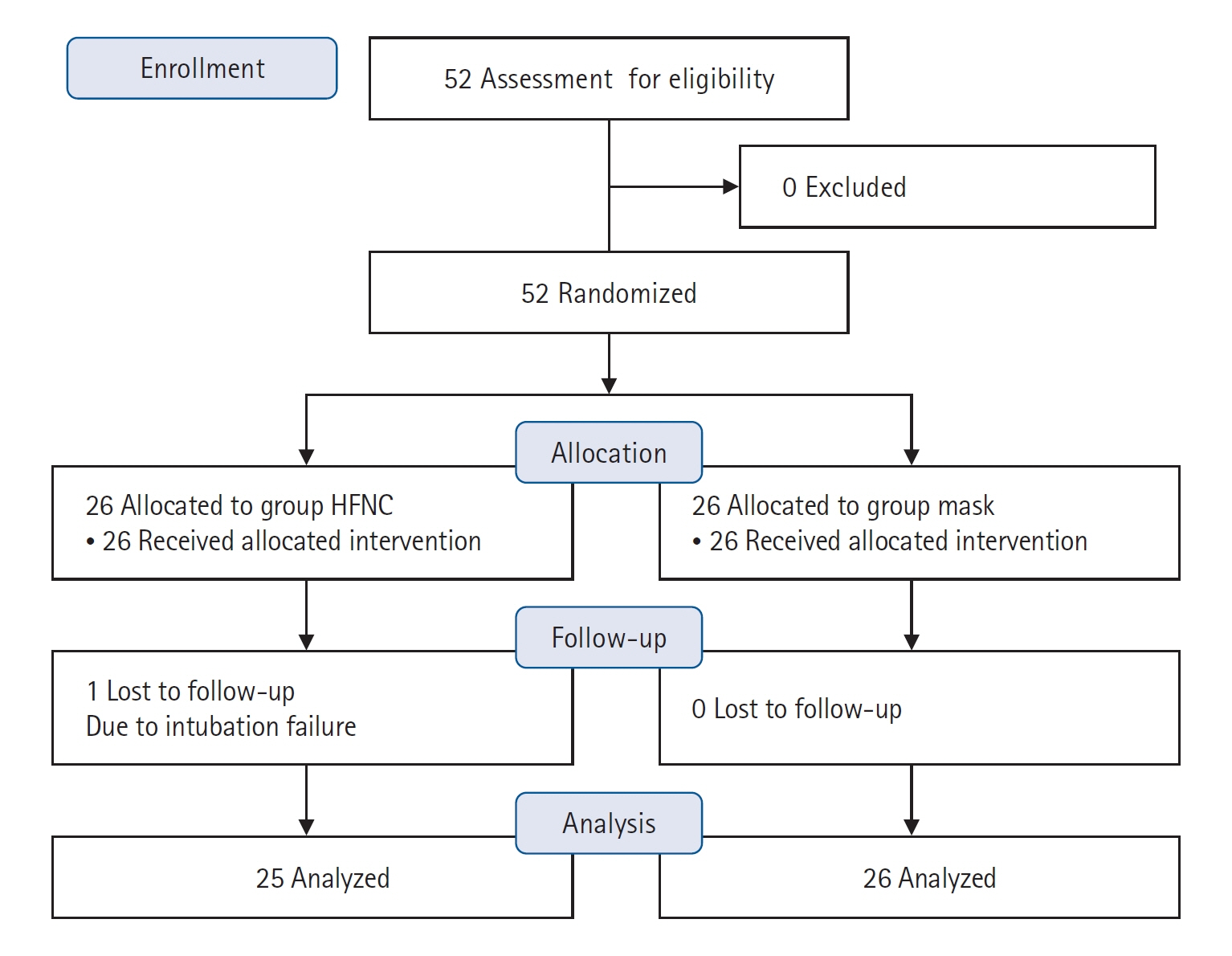
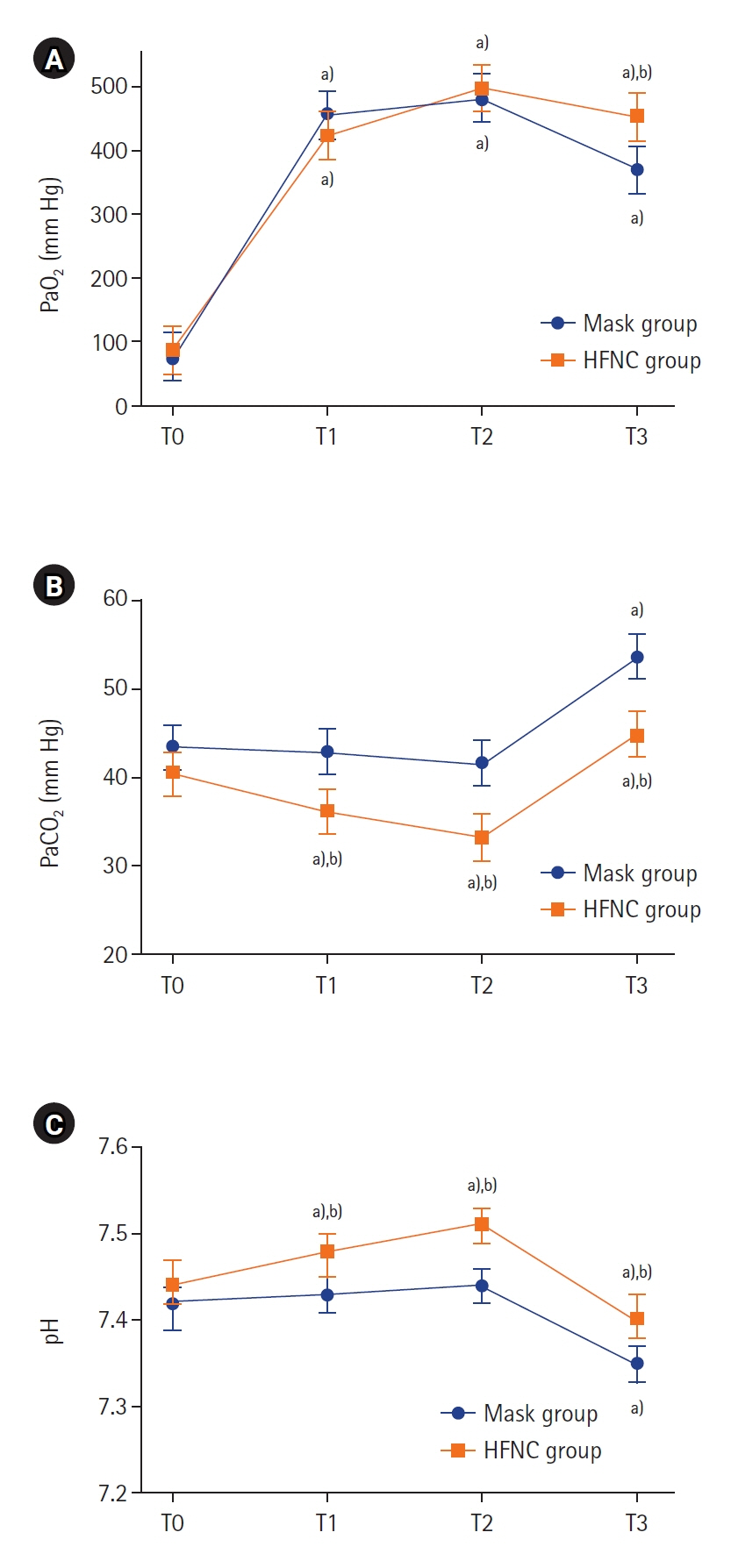
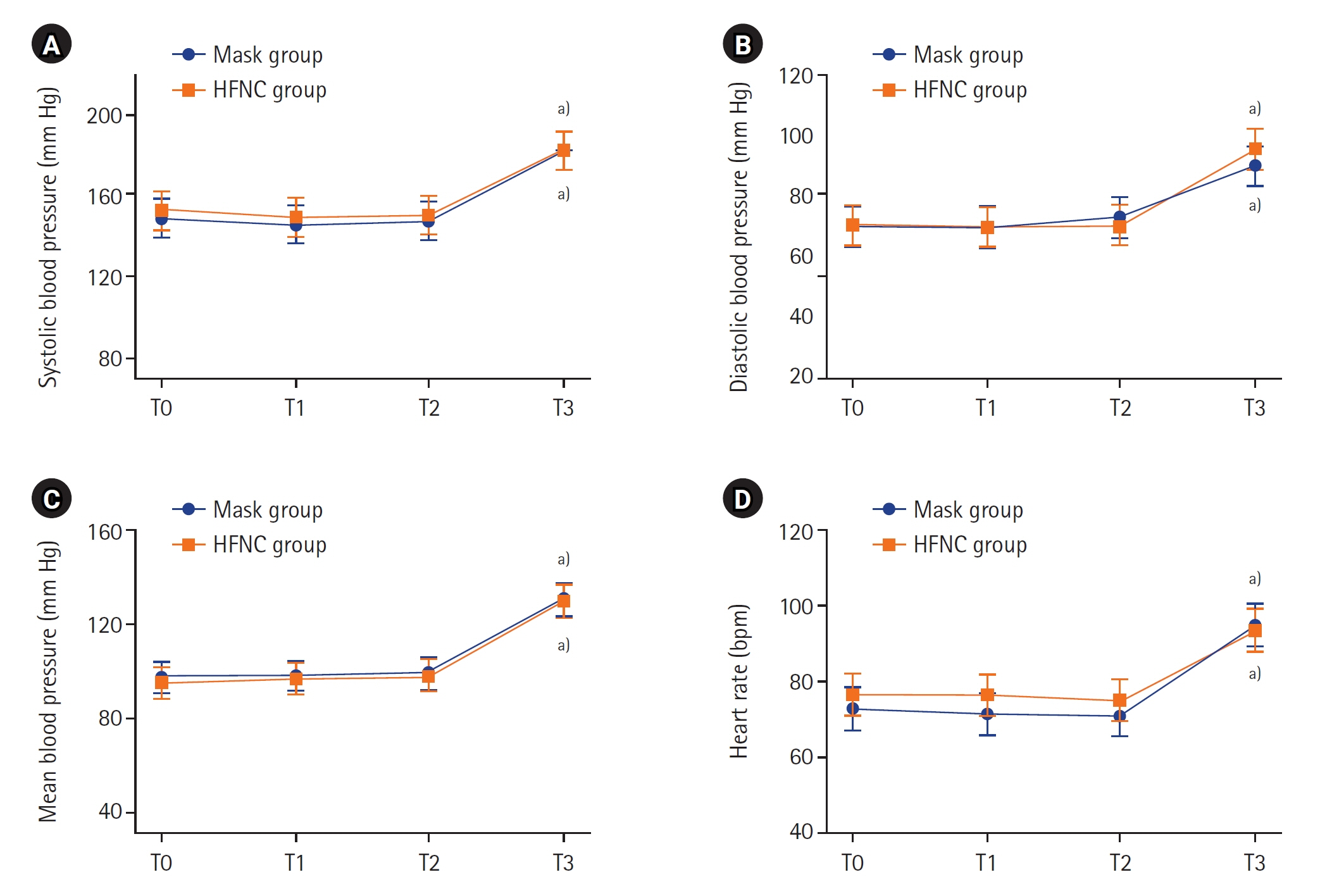
Although preoxygenation is an essential procedure for safe endotracheal intubation, in some cases securing sufficient time for tracheal intubation may not be possible. Patients with head and neck cancer might have a difficult airway and need a longer time for endotracheal intubation. We hypothesized that the extended apneic period with preoxygenation via a high-flow nasal cannula (HFNC) is beneficial to patients who undergo head and neck surgery compared with preoxygenation with a simple mask. Methods: The study was conducted as a single-center, single-blinded, prospective, randomized controlled trial. Patients were divided into groups based on one of the two preoxygenation methods: HFNC group or simple facemask (mask group). Preoxygenation was performed for 5 minutes with each method, and endotracheal intubation for all patients was performed using a video laryngoscope. Oxygen partial pressures of the arterial blood were compared at the predefined time points. Results: For the primary outcome, the mean arterial oxygen partial pressure (PaO2 ) immediately after intubation was 454.2 mm Hg (95% confidence interval [CI], 416.9–491.5 mm Hg) in the HFNC group and 370.7 mm Hg (95% CI, 333.7–407.4 mm Hg) in the mask group (P=0.002). The peak PaO2 at 5 minutes after preoxygenation was not statistically different between the groups (P=0.355). Conclusions: Preoxygenation with a HFNC extending to the apneic period before endotracheal intubation may be beneficial in patients with head and neck cancer.
Keyword
Figure
Reference
-
1. Bignami E, Saglietti F, Girombelli A, Briolini A, Bove T, Vetrugno L. Preoxygenation during induction of anesthesia in non-critically ill patients: a systematic review. J Clin Anesth. 2019; 52:85–90.
Article2. Shippam W, Preston R, Douglas J, Taylor J, Albert A, Chau A. High-flow nasal oxygen vs. standard flow-rate facemask pre-oxygenation in pregnant patients: a randomised physiological study. Anaesthesia. 2019; 74:450–6.
Article3. Frat JP, Ricard JD, Quenot JP, Pichon N, Demoule A, Forel JM, et al. Non-invasive ventilation versus high-flow nasal cannula oxygen therapy with apnoeic oxygenation for preoxygenation before intubation of patients with acute hypoxaemic respiratory failure: a randomised, multicentre, open-label trial. Lancet Respir Med. 2019; 7:303–12.4. Bouroche G, Bourgain JL. Preoxygenation and general anesthesia: a review. Minerva Anestesiol. 2015; 81:910–20.5. Heinrich S, Horbach T, Stubner B, Prottengeier J, Irouschek A, Schmidt J. Benefits of heated and humidified high flow nasal oxygen for preoxygenation in morbidly obese patients undergoing bariatric surgery: a randomized controlled study. J Obes Bariatrics. 2014; 1:7.6. Azam Danish M. Preoxygenation and anesthesia: a detailed review. Cureus. 2021; 13:e13240.
Article7. Mariyaselvam M, Stolady D, Wijewardena G, Blunt M, Young P. Transnasal humidified rapid insufflation ventilatory exchange for pre-oxygenation and apnoeic oxygenation during rapid sequence induction. Crit Care. 2015; 19(Suppl 1):P208.
Article8. Stolady D, Mariyaselvam M, Young H, Fawzy E, Blunt M, Young P, et al. Pharyngeal oxygenation during apnoea following conventional pre-oxygenation and high-flow nasal oxygenation. Crit Care. 2015; 19(Suppl 1):P200.
Article9. Grude O, Solli HJ, Andersen C, Oveland NP. Effect of nasal or nasopharyngeal apneic oxygenation on desaturation during induction of anesthesia and endotracheal intubation in the operating room: a narrative review of randomized controlled trials. J Clin Anesth. 2018; 51:1–7.
Article10. Ramachandran SK, Cosnowski A, Shanks A, Turner CR. Apneic oxygenation during prolonged laryngoscopy in obese patients: a randomized, controlled trial of nasal oxygen administration. J Clin Anesth. 2010; 22:164–8.
Article11. Jo JY, Kim WJ, Ku S, Choi SS. Comparison of preoxygenation with a high-flow nasal cannula and a simple mask before intubation during induction of general anesthesia in patients undergoing head and neck surgery: Study protocol clinical trial (SPIRIT Compliant). Medicine (Baltimore). 2020; 99:e19525.12. Luo D, Wan X, Liu J, Tong T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res. 2018; 27:1785–805.
Article13. Pillai A, Daga V, Lewis J, Mahmoud M, Mushambi M, Bogod D. High-flow humidified nasal oxygenation vs. standard face mask oxygenation. Anaesthesia. 2016; 71:1280–3.
Article14. Mir F, Patel A, Iqbal R, Cecconi M, Nouraei SA. A randomised controlled trial comparing transnasal humidified rapid insufflation ventilatory exchange (THRIVE) pre-oxygenation with facemask pre-oxygenation in patients undergoing rapid sequence induction of anaesthesia. Anaesthesia. 2017; 72:439–43.
Article15. Tanoubi I, Drolet P, Donati F. Optimizing preoxygenation in adults. Can J Anaesth. 2009; 56:449–66.
Article16. Nimmagadda U, Salem MR, Crystal GJ. Preoxygenation: physiologic basis, benefits, and potential risks. Anesth Analg. 2017; 124:507–17.
Article17. Lee HW, Choi SM, Lee J, Park YS, Lee CH, Yoo CG, et al. Reduction of PaCO2 by high-flow nasal cannula in acute hypercapnic respiratory failure patients receiving conventional oxygen therapy. Acute Crit Care. 2019; 34:202–11.
Article18. Kim HJ, Asai T. High-flow nasal oxygenation for anesthetic management. Korean J Anesthesiol. 2019; 72:527–47.
Article19. Kim ES, Lee H, Kim SJ, Park J, Lee YJ, Park JS, et al. Effectiveness of high-flow nasal cannula oxygen therapy for acute respiratory failure with hypercapnia. J Thorac Dis. 2018; 10:882–8.
Article20. Huang Y, Lei W, Zhang W, Huang JA. High-flow nasal cannula in hypercapnic respiratory failure: a systematic review and meta-analysis. Can Respir J. 2020; 2020:7406457.
Article21. Lyons C, Callaghan M. Uses and mechanisms of apnoeic oxygenation: a narrative review. Anaesthesia. 2019; 74:497–507.
Article22. Tournadre JP, Allaouchiche B, Malbert CH, Chassard D. Metabolic acidosis and respiratory acidosis impair gastro-pyloric motility in anesthetized pigs. Anesth Analg. 2000; 90:74–9.
Article23. Epstein SK, Singh N. Respiratory acidosis. Respir Care. 2001; 46:366–83.24. Walley KR, Lewis TH, Wood LD. Acute respiratory acidosis decreases left ventricular contractility but increases cardiac output in dogs. Circ Res. 1990; 67:628–35.
Article25. Andersen MN, Mouritzen C. Effect of acute respiratory and metabolic acidosis on cardiac output and peripheral resistance. Ann Surg. 1966; 163:161–8.
Article26. Fike CD, Hansen TN. The effect of alkalosis on hypoxia-induced pulmonary vasoconstriction in lungs of newborn rabbits. Pediatr Res. 1989; 25:383–8.
Article27. Morel J, Gergele L, Domine A, Molliex S, Perrot JL, Labeille B, et al. The venous-arterial difference in CO2 should be interpreted with caution in case of respiratory alkalosis in healthy volunteers. J Clin Monit Comput. 2017; 31:701–7.
Article28. Samuelsson RG, Nagy G. Effects of respiratory alkalosis and acidosis on myocardial excitation. Acta Physiol Scand. 1976; 97:158–65.
Article29. Crawley SM, Dalton AJ. Predicting the difficult airway. BJA Educ. 2015; 15:253–7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Successful anesthetic management of a giant lower lip hemangioma patient using high flow nasal cannula -a case report-
- High Flow Nasal Cannula Assisted Tracheostomy for Securing Airways in Patients with Acute Respiratory Distress Induced by Glottic Cancer
- High-flow nasal oxygenation for anesthetic management
- Factors about Failure after High Flow Oxygen through Nasal Cannula Therapy in Hypoxic Respiratory Failure Patients at Emergency Department Presentation
- Use of a human patient simulator for apnea studies: a preliminary in vitro trial