Acute Crit Care.
2024 Feb;39(1):47-60. 10.4266/acc.2023.01284.
Prolonged intensive care: muscular functional, and nutritional insights from the COVID-19 pandemic
- Affiliations
-
- 1Department of Critical Care Rehabilitation, Hospital General de México “Dr. Eduardo Liceaga”, Mexico City, Mexico
- 2Department of Clinical Nutrition, Hospital General de México “Dr. Eduardo Liceaga”, Mexico City, Mexico
- 3Division of Critical Care, Hospital General de México “Dr. Eduardo Liceaga”, Mexico City, Mexico
- KMID: 2555223
- DOI: http://doi.org/10.4266/acc.2023.01284
Abstract
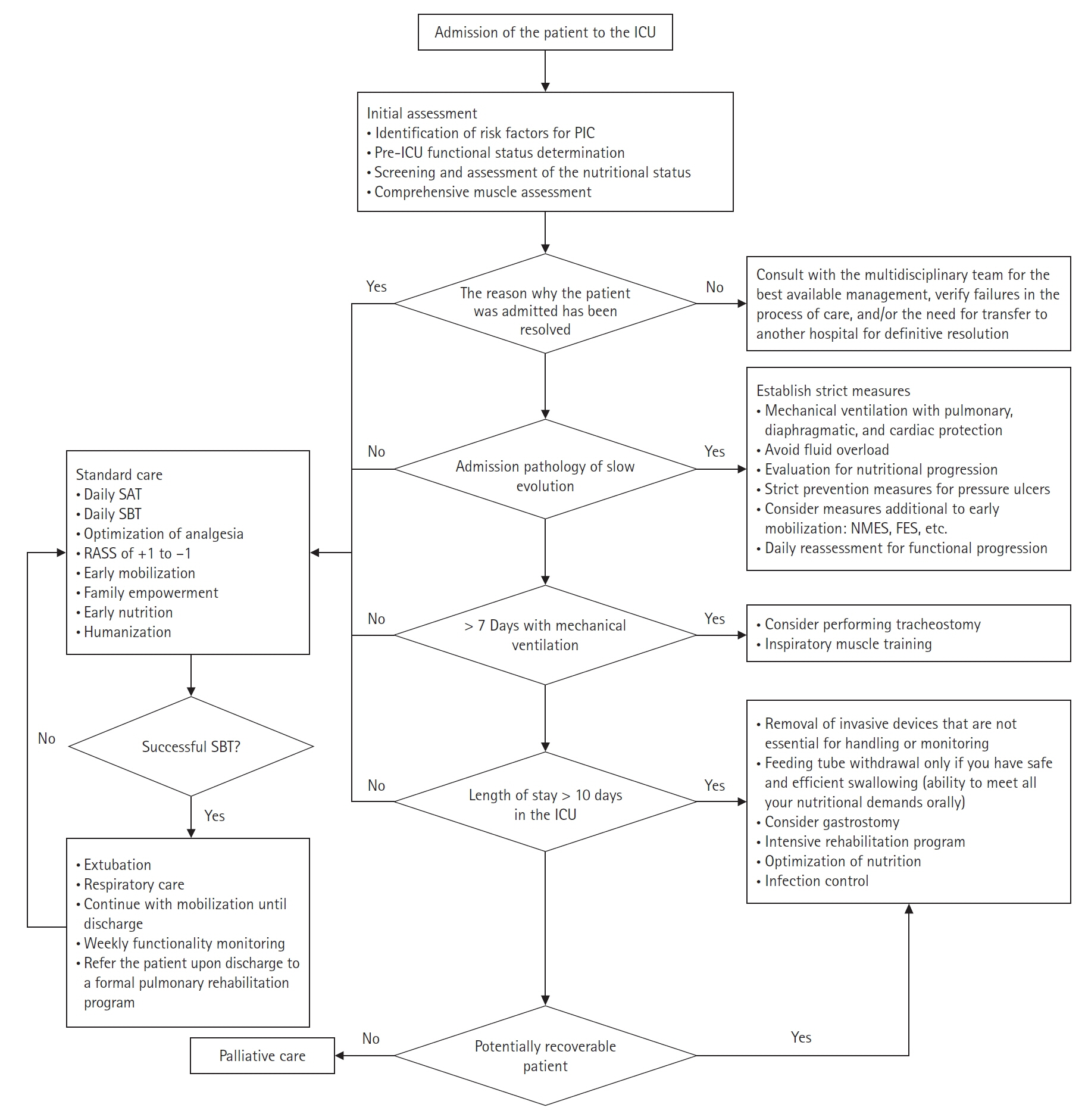
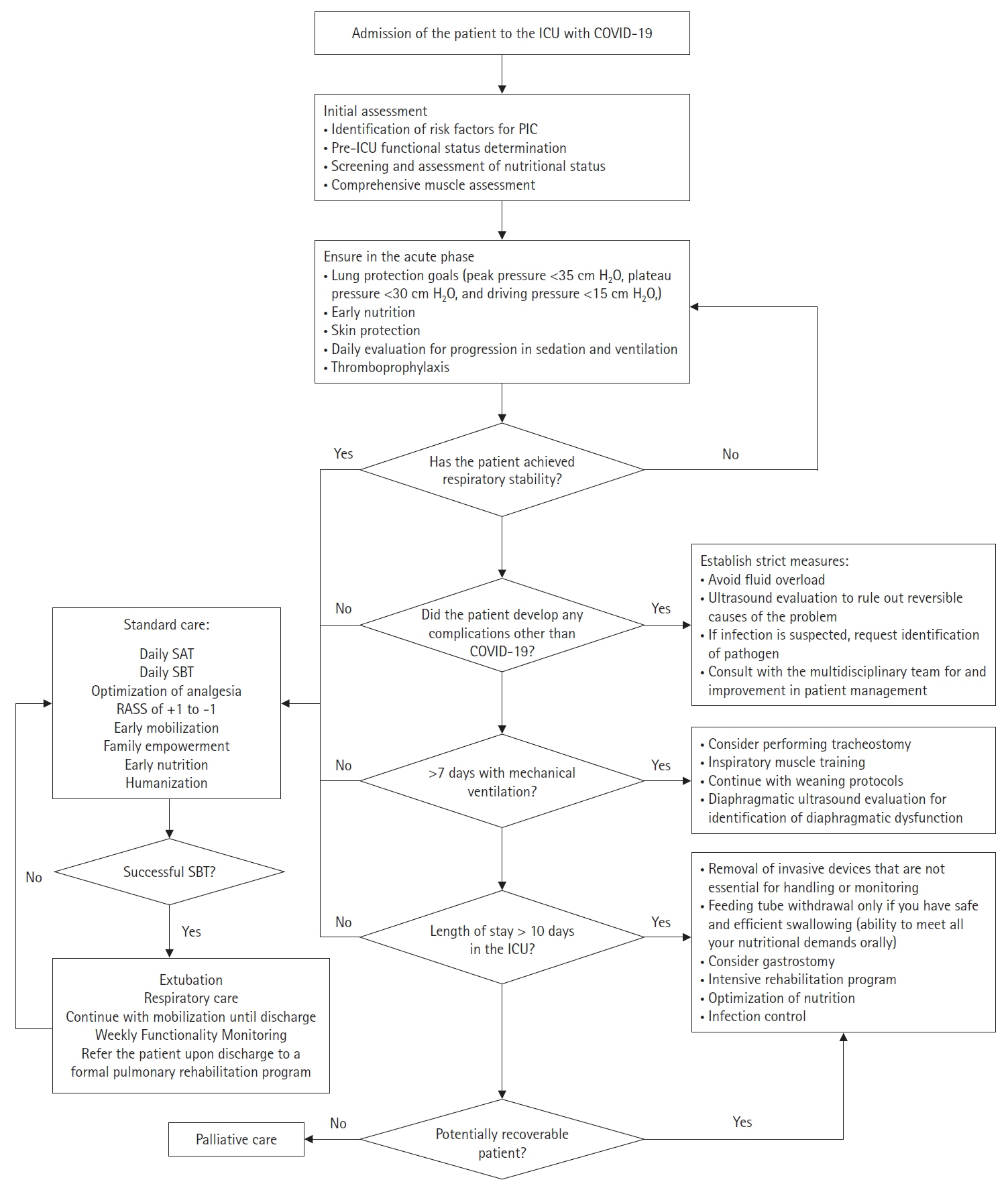
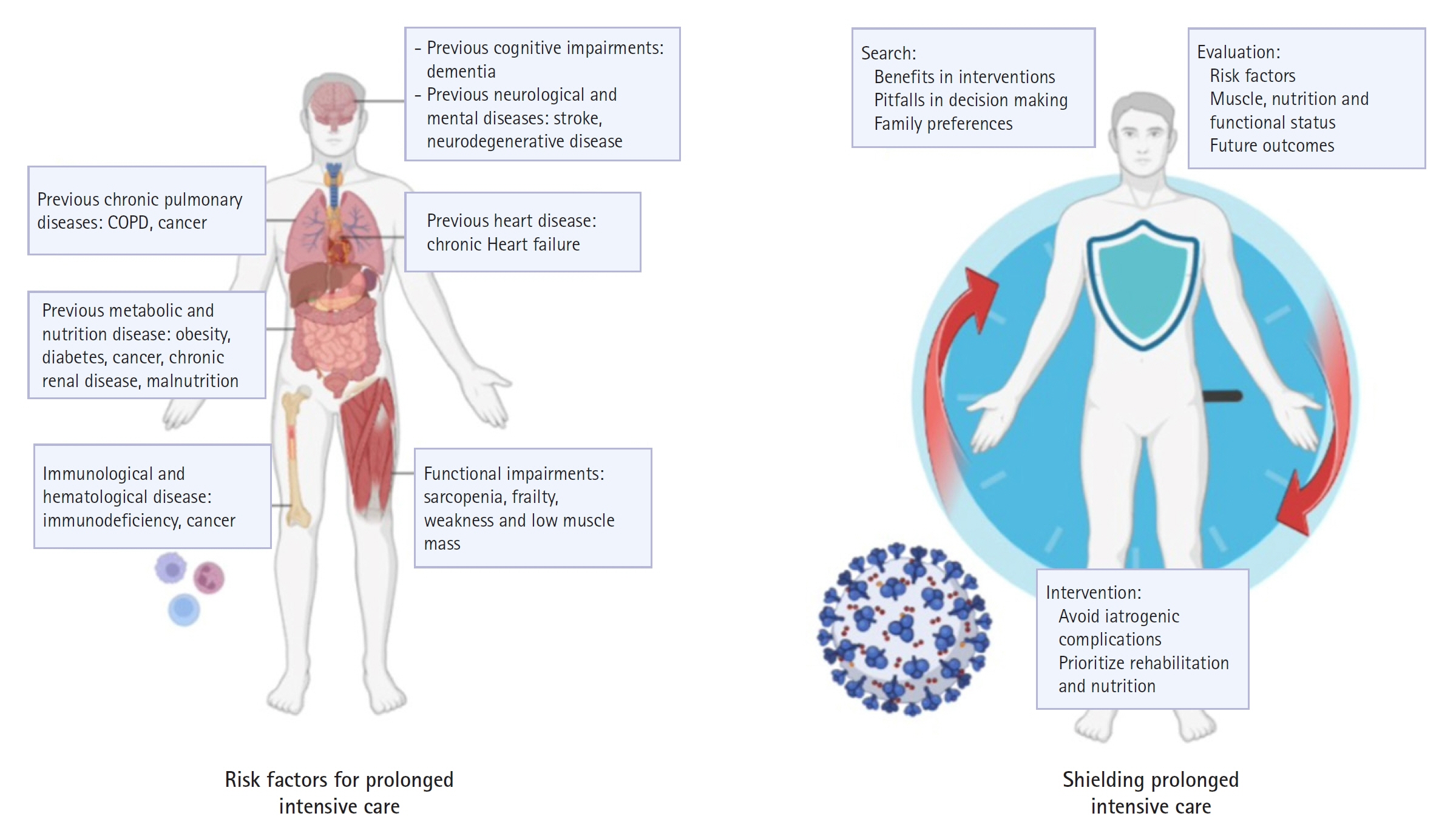
- During the coronavirus disease 2019 (COVID-19) pandemic, clinical staff learned how to manage patients enduring extended stays in an intensive care unit (ICU). COVID-19 patients requiring critical care in an ICU face a high risk of experiencing prolonged intensive care (PIC). The use of invasive mechanical ventilation in individuals with severe acute respiratory distress syndrome can cause numerous complications that influence both short-term and long-term morbidity and mortality. Those risks underscore the importance of proactively addressing functional complications. Mitigating secondary complications unrelated to the primary pathology of admission is imperative in minimizing the risk of PIC. Therefore, incorporating strategies to do that into daily ICU practice for both COVID-19 patients and those critically ill from other conditions is significantly important.
Keyword
Figure
Reference
-
1. Damuth E, Mitchell JA, Bartock JL, Roberts BW, Trzeciak S. Long-term survival of critically ill patients treated with prolonged mechanical ventilation: a systematic review and meta-analysis. Lancet Respir Med. 2015; 3:544–53.
Article2. Kamdar BB, Suri R, Suchyta MR, Digrande KF, Sherwood KD, Colantuoni E, et al. Return to work after critical illness: a systematic review and meta-analysis. Thorax. 2020; 75:17–27.
Article3. Iwashyna TJ, Hodgson CL, Pilcher D, Bailey M, van Lint A, Chavan S, et al. Timing of onset and burden of persistent critical illness in Australia and New Zealand: a retrospective, population-based, observational study. Lancet Respir Med. 2016; 4:566–73.
Article4. Iwashyna TJ, Viglianti EM. Patient and population-level approaches to persistent critical illness and prolonged intensive care unit stays. Crit Care Clin. 2018; 34:493–500.
Article5. Chatterjee SK, Saha S, Munoz MN. Molecular pathogenesis, immunopathogenesis and novel therapeutic strategy against COVID-19. Front Mol Biosci. 2020; 7:196.
Article6. Roedl K, Jarczak D, Boenisch O, de Heer G, Burdelski C, Frings D, et al. Chronic critical illness in patients with COVID-19: characteristics and outcome of prolonged intensive care therapy. J Clin Med. 2022; 11:1049.
Article7. Voiriot G, Oualha M, Pierre A, Salmon-Gandonnière C, Gaudet A, Jouan Y, et al. Chronic critical illness and post-intensive care syndrome: from pathophysiology to clinical challenges. Ann Intensive Care. 2022; 12:58.
Article8. Bonorino KC, Cani KC. Early mobilization in the time of COVID-19. Rev Bras Ter Intensiva. 2020; 32:484–6.
Article9. Melamed R, Paz F, Jepsen S, Smith C, Saavedra R, Mulder M, et al. Prognostic factors and outcomes in COVID-19 patients requiring prolonged mechanical ventilation: a retrospective cohort study. Ther Adv Respir Dis. 2022; 16:17534666221086415.
Article10. Nakanishi N, Liu K, Kawakami D, Kawai Y, Morisawa T, Nishida T, et al. Post-intensive care syndrome and its new challenges in coronavirus disease 2019 (COVID-19) pandemic: a review of recent advances and perspectives. J Clin Med. 2021; 10:3870.
Article11. WHO Rapid Evidence Appraisal for COVID-19 Therapies (REACT) Working Group, Sterne JA, Murthy S, Diaz JV, Slutsky AS, Villar J, et al. Association between administration of systemic corticosteroids and mortality among critically ill patients with COVID-19: a meta-analysis. JAMA. 2020; 324:1330–41.12. Papazian L, Aubron C, Brochard L, Chiche JD, Combes A, Dreyfuss D, et al. Formal guidelines: management of acute respiratory distress syndrome. Ann Intensive Care. 2019; 9:69.
Article13. Yang T, Li Z, Jiang L, Wang Y, Xi X. Risk factors for intensive care unit-acquired weakness: a systematic review and meta-analysis. Acta Neurol Scand. 2018; 138:104–14.
Article14. Stripari Schujmann D, Claudia Lunardi A, Neri Peso C, Pompeu JE, Annoni R, Miura MC, et al. Functional recovery groups in critically ill COVID-19 patients and their associated factors: from ICU to hospital discharge. Crit Care Med. 2022; 50:1799–808.
Article15. Soto GL. The chronic critical patient. Rev Med Clin Condes. 2019; 30:160–70.16. Loss SH, Nunes DS, Franzosi OS, Salazar GS, Teixeira C, Vieira SR. Chronic critical illness: are we saving patients or creating victims? Rev Bras Ter Intensiva. 2017; 29:87–95.
Article17. Baggerman MR, van Dijk DP, Winkens B, van Gassel RJ, Bol ME, Schnabel RM, et al. Muscle wasting associated co-morbidities, rather than sarcopenia are risk factors for hospital mortality in critical illness. J Crit Care. 2020; 56:31–6.
Article18. Kahn JM, Le T, Angus DC, Cox CE, Hough CL, White DB, et al. The epidemiology of chronic critical illness in the United States. Crit Care Med. 2015; 43:282–7.
Article19. Kou HW, Yeh CH, Tsai HI, Hsu CC, Hsieh YC, Chen WT, et al. Sarcopenia is an effective predictor of difficult-to-wean and mortality among critically ill surgical patients. PLoS One. 2019; 14:e0220699.
Article20. Muscedere J, Waters B, Varambally A, Bagshaw SM, Boyd JG, Maslove D, et al. The impact of frailty on intensive care unit outcomes: a systematic review and meta-analysis. Intensive Care Med. 2017; 43:1105–22.
Article21. Instituto Nacional de Estadística y Geografía. Encuesta Nacional de Salud y Nutrición 2018: diseño conceptual. Instituto Nacional de Salud Pública;2018.22. Zhou D, Wang C, Lin Q, Li T. The obesity paradox for survivors of critically ill patients. Crit Care. 2022; 26:198.
Article23. Azevedo LC, Caruso P, Silva UV, Torelly AP, Silva E, Rezende E, et al. Outcomes for patients with cancer admitted to the ICU requiring ventilatory support: results from a prospective multicenter study. Chest. 2014; 146:257–66.
Article24. Salahuddin N, Sammani M, Hamdan A, Joseph M, Al-Nemary Y, Alquaiz R, et al. Fluid overload is an independent risk factor for acute kidney injury in critically ill patients: results of a cohort study. BMC Nephrol. 2017; 18:45.
Article25. Osuna-Padilla IA, Rodríguez-Moguel NC, Rodríguez-Llamazares S, Orsso CE, Prado CM, Ríos-Ayala MA, et al. Low muscle mass in COVID-19 critically-ill patients: prognostic significance and surrogate markers for assessment. Clin Nutr. 2022; 41:2910–7.
Article26. Meduri GU, Chrousos GP. General adaptation in critical illness: glucocorticoid receptor-alpha master regulator of homeostatic corrections. Front Endocrinol (Lausanne). 2020; 11:161.
Article27. Wang W, Xu C, Ma X, Zhang X, Xie P. Intensive care unit-acquired weakness: a review of recent progress with a look toward the future. Front Med (Lausanne). 2020; 7:559789.
Article28. Kho ME, Rewa OG, Boyd JG, Choong K, Stewart GC, Herridge MS. Outcomes of critically ill COVID-19 survivors and caregivers: a case study-centred narrative review. Can J Anaesth. 2022; 69:630–43.
Article29. Umbrello M, Guglielmetti L, Formenti P, Antonucci E, Cereghini S, Filardo C, et al. Qualitative and quantitative muscle ultrasound changes in patients with COVID-19-related ARDS. Nutrition. 2021; 91-92:111449.
Article30. Nakanishi N, Oto J, Tsutsumi R, Akimoto Y, Nakano Y, Nishimura M. Upper limb muscle atrophy associated with in-hospital mortality and physical function impairments in mechanically ventilated critically ill adults: a two-center prospective observational study. J Intensive Care. 2020; 8:87.
Article31. Vanhorebeek I, Latronico N, Van den Berghe G. ICU-acquired weakness. Intensive Care Med. 2020; 46:637–53.
Article32. Formenti P, Umbrello M, Coppola S, Froio S, Chiumello D. Clinical review: peripheral muscular ultrasound in the ICU. Ann Intensive Care. 2019; 9:57.
Article33. Toledo DO, Freitas BJ, Dib R, Pfeilsticker FJ, Santos DM, Gomes BC, et al. Peripheral muscular ultrasound as outcome assessment tool in critically ill patients on mechanical ventilation: an observational cohort study. Clin Nutr ESPEN. 2021; 43:408–14.
Article34. Haaksma ME, Smit JM, Boussuges A, Demoule A, Dres M, Ferrari G, et al. EXpert consensus On Diaphragm UltraSonography in the critically ill (EXODUS): a Delphi consensus statement on the measurement of diaphragm ultrasound-derived parameters in a critical care setting. Crit Care. 2022; 26:99.
Article35. Schreiber A, Bertoni M, Goligher EC. Avoiding respiratory and peripheral muscle injury during mechanical ventilation: diaphragm-protective ventilation and early mobilization. Crit Care Clin. 2018; 34:357–81.36. Looijaard WG, Molinger J, Weijs PJ. Measuring and monitoring lean body mass in critical illness. Curr Opin Crit Care. 2018; 24:241–7.
Article37. Jung C, Guidet B, Flaatten H; VIP study group. Frailty in intensive care medicine must be measured, interpreted and taken into account! Intensive Care Med. 2023; 49:87–90.
Article38. Bruno RR, Wernly B, Flaatten H, Fjølner J, Artigas A, Baldia PH, et al. The association of the activities of daily living and the outcome of old intensive care patients suffering from COVID-19. Ann Intensive Care. 2022; 12:26.39. Subramaniam A, Ueno R, Tiruvoipati R, Srikanth V, Bailey M, Pilcher D. Comparison of the predictive ability of clinical frailty scale and hospital frailty risk score to determine long-term survival in critically ill patients: a multicentre retrospective cohort study. Crit Care. 2022; 26:121.
Article40. Parry SM, Huang M, Needham DM. Evaluating physical functioning in critical care: considerations for clinical practice and research. Crit Care. 2017; 21:249.
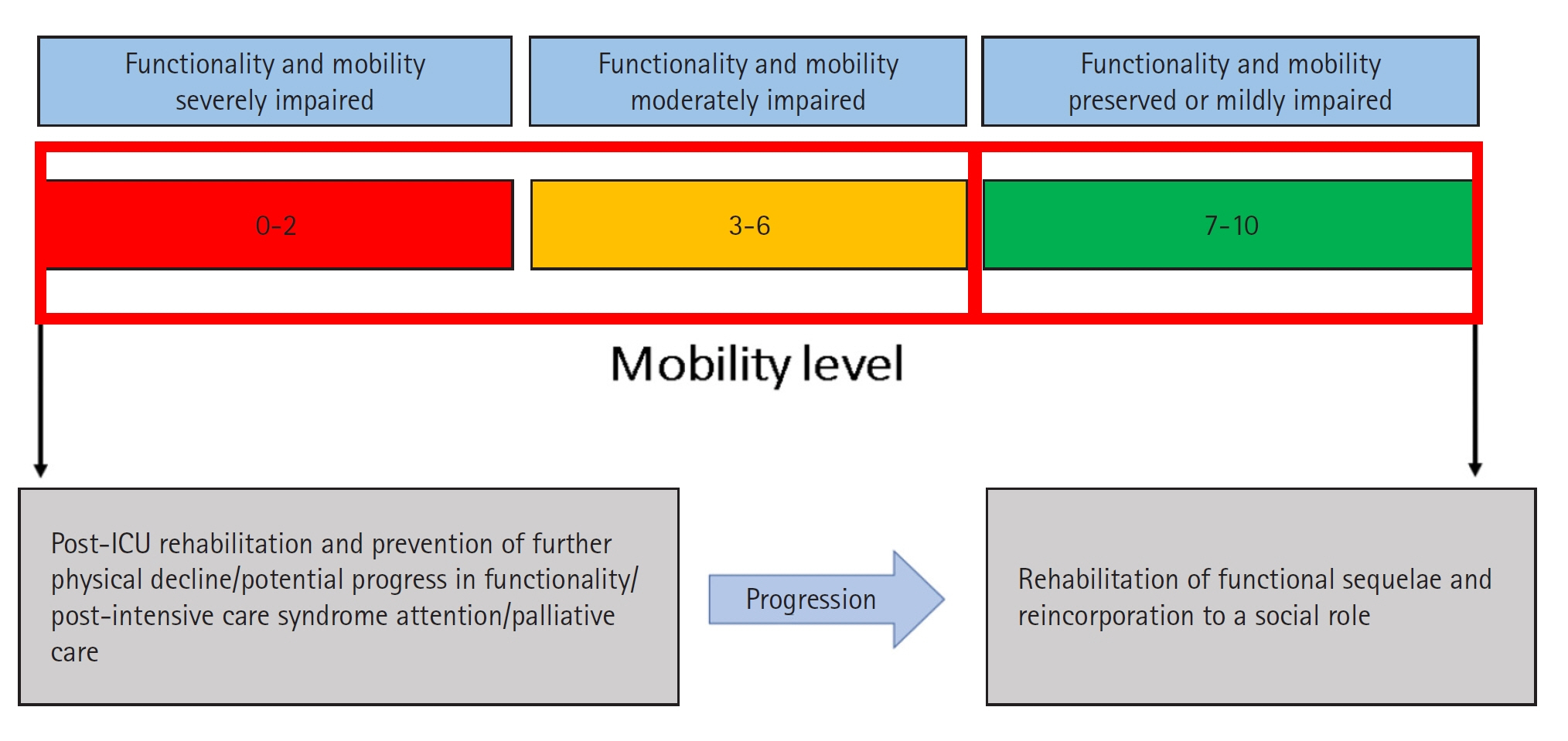
Article41. Tipping CJ, Bailey MJ, Bellomo R, Berney S, Buhr H, Denehy L, et al. The ICU mobility scale has construct and predictive validity and is responsive. a multicenter observational study. Ann Am Thorac Soc. 2016; 13:887–93.
Article42. Tipping CJ, Holland AE, Harrold M, Crawford T, Halliburton N, Hodgson CL. The minimal important difference of the ICU mobility scale. Heart Lung. 2018; 47:497–501.
Article43. Liu K, Nakamura K, Kudchadkar SR, Katsukawa H, Nydahl P, Ely EW, et al. Mobilization and rehabilitation practice in ICUs during the COVID-19 pandemic. J Intensive Care Med. 2022; 37:1256–64.
Article44. Arabi YM, Casaer MP, Chapman M, Heyland DK, Ichai C, Marik PE, et al. The intensive care medicine research agenda in nutrition and metabolism. Intensive Care Med. 2017; 43:1239–56.
Article45. Hill A, Elke G, Weimann A. Nutrition in the intensive care unit-A narrative review. Nutrients. 2021; 13:2851.
Article46. Bolayir B, Arik G, Yeşil Y, Kuyumcu ME, Varan HD, Kara Ö, et al. Validation of Nutritional Risk Screening-2002 in a hospitalized adult population. Nutr Clin Pract. 2019; 34:297–303.
Article47. de Vries MC, Koekkoek WK, Opdam MH, van Blokland D, van Zanten AR. Nutritional assessment of critically ill patients: validation of the modified NUTRIC score. Eur J Clin Nutr. 2018; 72:428–35.
Article48. Cederholm T, Jensen GL, Correia MI, Gonzalez MC, Fukushima R, Higashiguchi T, et al. GLIM criteria for the diagnosis of malnutrition: a consensus report from the global clinical nutrition community. Clin Nutr. 2019; 38:1–9.49. Singer P, Blaser AR, Berger MM, Alhazzani W, Calder PC, Casaer MP, et al. ESPEN guideline on clinical nutrition in the intensive care unit. Clin Nutr. 2019; 38:48–79.
Article50. Thibault R, Seguin P, Tamion F, Pichard C, Singer P. Nutrition of the COVID-19 patient in the intensive care unit (ICU): a practical guidance. Crit Care. 2020; 24:447.
Article51. Nakanishi N, Tsutsumi R, Okayama Y, Takashima T, Ueno Y, Itagaki T, et al. Monitoring of muscle mass in critically ill patients: comparison of ultrasound and two bioelectrical impedance analysis devices. J Intensive Care. 2019; 7:61.
Article52. Preiser JC, van Zanten AR, Berger MM, Biolo G, Casaer MP, Doig GS, et al. Metabolic and nutritional support of critically ill patients: consensus and controversies. Crit Care. 2015; 19:35.
Article53. Hawkins RB, Raymond SL, Stortz JA, Horiguchi H, Brakenridge SC, Gardner A, et al. Chronic critical illness and the persistent inflammation, immunosuppression, and catabolism syndrome. Front Immunol. 2018; 9:1511.
Article54. da Silva JS, Seres DS, Sabino K, Adams SC, Berdahl GJ, Citty SW, et al. ASPEN consensus recommendations for refeeding syndrome. Nutr Clin Pract. 2020; 35:178–95.
Article55. Cereda E, Clavé P, Collins PF, Holdoway A, Wischmeyer PE. Recovery focused nutritional therapy across the continuum of care: learning from COVID-19. Nutrients. 2021; 13:3293.
Article56. Barazzoni R, Bischoff SC, Breda J, Wickramasinghe K, Krznaric Z, Nitzan D, et al. ESPEN expert statements and practical guidance for nutritional management of individuals with SARS-CoV-2 infection. Clin Nutr. 2020; 39:1631–8.
Article57. Cavalleri J, Treguier D, Deliège T, Gurdebeke C, Ernst M, Lambermont B, et al. One-year functional decline in COVID-19 and non-COVID-19 critically ill survivors: a prospective study incorporating a pre-ICU status assessment. Healthcare (Basel). 2022; 10:2023.
Article58. Hodgson CL, Higgins AM, Bailey MJ, Mather AM, Beach L, Bellomo R, et al. The impact of COVID-19 critical illness on new disability, functional outcomes and return to work at 6 months: a prospective cohort study. Crit Care. 2021; 25:382.
Article59. Cameron S, Ball I, Cepinskas G, Choong K, Doherty TJ, Ellis CG, et al. Early mobilization in the critical care unit: a review of adult and pediatric literature. J Crit Care. 2015; 30:664–72.
Article60. Lipshutz AK, Engel H, Thornton K, Gropper MA. Early mobilization in the intensive care unit: evidence and implementation. ICU Dir. 2012; 3:10–6.61. Zang K, Chen B, Wang M, Chen D, Hui L, Guo S, et al. The effect of early mobilization in critically ill patients: a meta-analysis. Nurs Crit Care. 2020; 25:360–7.
Article62. Olkowski BF, Shah SO. Early mobilization in the neuro-ICU: how far can we go? Neurocrit Care. 2017; 27:141–50.
Article63. Clarissa C, Salisbury L, Rodgers S, Kean S. Early mobilisation in mechanically ventilated patients: a systematic integrative review of definitions and activities. J Intensive Care. 2019; 7:3.
Article64. Paton M, Chan S, Tipping CJ, Stratton A, Serpa Neto A, Lane R, et al. The effect of mobilization at 6 months after critical illness: meta-analysis. NEJM Evid. 2023; 2:EVIDoa2200234.65. Devlin JW, Skrobik Y, Gélinas C, Needham DM, Slooter AJ, Pandharipande PP, et al. Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit Care Med. 2018; 46:e825–73.66. Pan H, Shi W, Zhou Q, Chen G, Pan P. Palliative care in the intensive care unit: not just end-of-life care. Intensive Care Res. 2023; 3:77–82.
Article67. Ito K, George N, Wilson J, Bowman J, Aaronson E, Ouchi K. Primary palliative care recommendations for critical care clinicians. J Intensive Care. 2022; 10:20.
Article68. Vincent JL. The continuum of critical care. Crit Care. 2019; 23(Suppl 1):122.
Article69. Zhang L, Hu W, Cai Z, Liu J, Wu J, Deng Y, et al. Early mobilization of critically ill patients in the intensive care unit: a systematic review and meta-analysis. PLoS One. 2019; 14:e0223185.
Article70. Ding N, Zhang Z, Zhang C, Yao L, Yang L, Jiang B, et al. What is the optimum time for initiation of early mobilization in mechanically ventilated patients?: a network meta-analysis. PLoS One. 2019; 14:e0223151.
Article71. Menges D, Seiler B, Tomonaga Y, Schwenkglenks M, Puhan MA, Yebyo HG. Systematic early versus late mobilization or standard early mobilization in mechanically ventilated adult ICU patients: systematic review and meta-analysis. Crit Care. 2021; 25:16.
Article72. Pun BT, Balas MC, Barnes-Daly MA, Thompson JL, Aldrich JM, Barr J, et al. Caring for critically ill patients with the ABCDEF bundle: results of the ICU liberation collaborative in over 15,000 adults. Crit Care Med. 2019; 47:3–14.
Article73. Arias-Fernández P, Romero-Martin M, Gómez-Salgado J, Fernández-García D. Rehabilitation and early mobilization in the critical patient: systematic review. J Phys Ther Sci. 2018; 30:1193–201.
Article74. Tanaka A, Uchiyama A, Kitamura T, Sakaguchi R, Komukai S, Matsuyama T, et al. Association between early tracheostomy and patient outcomes in critically ill patients on mechanical ventilation: a multicenter cohort study. J Intensive Care. 2022; 10:19.
Article75. Evans L, Rhodes A, Alhazzani W, Antonelli M, Coopersmith CM, French C, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 2021; 47:1181–247.