Ann Rehabil Med.
2024 Apr;48(2):146-154. 10.5535/arm.230028.
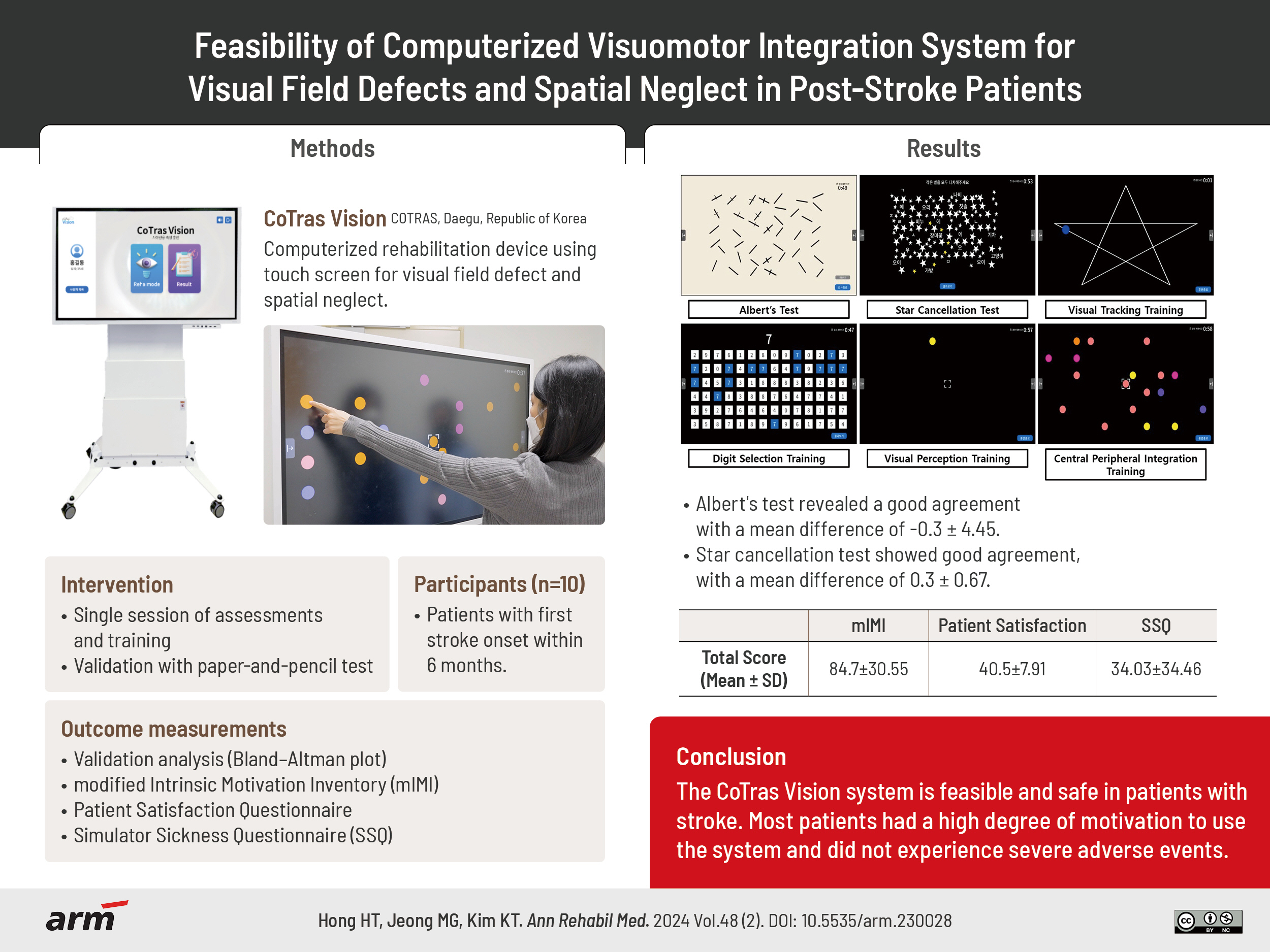
Feasibility of Computerized Visuomotor Integration System for Visual Field Defects and Spatial Neglect in Poststroke Patients
- Affiliations
-
- 1Department of Rehabilitation Medicine, Keimyung University Dongsan Hospital, Keimyung University School of Medicine, Daegu, Korea
- 2Department of Rehabilitation Science, Graduate School, Daegu University, Gyeongsan, Korea
- KMID: 2554790
- DOI: http://doi.org/10.5535/arm.230028
Abstract
Objective
To develop a computerized visuomotor integration system for assessment and training of visual perception impairments and evaluate its safety and feasibility in patients with a stroke. Visual field defects and spatial neglect lead to substantial poststroke impairment. Most diagnostic assessments are anchored in traditional methods, and clinical effects of rehabilitation treatments are limited.
Methods
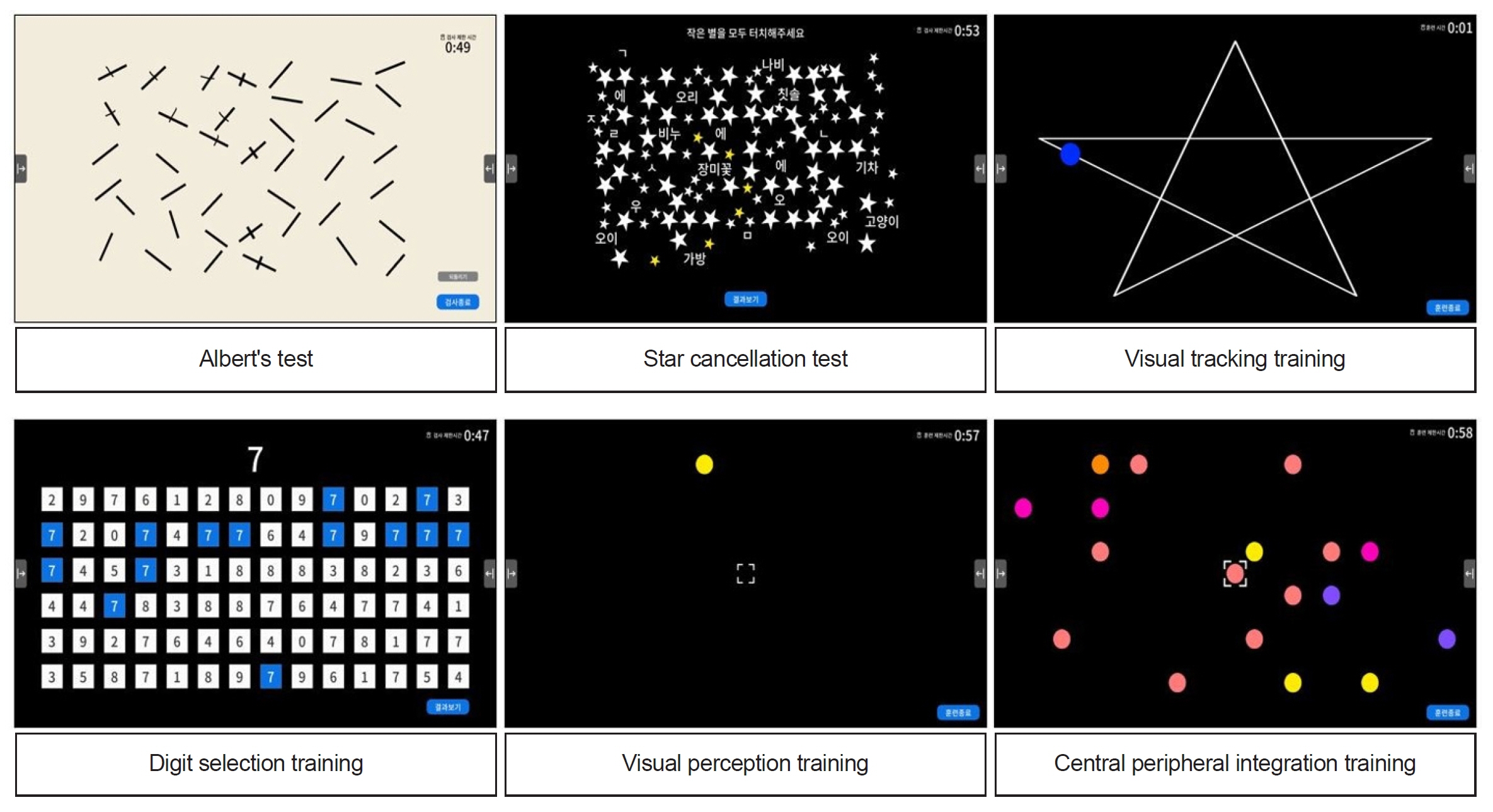
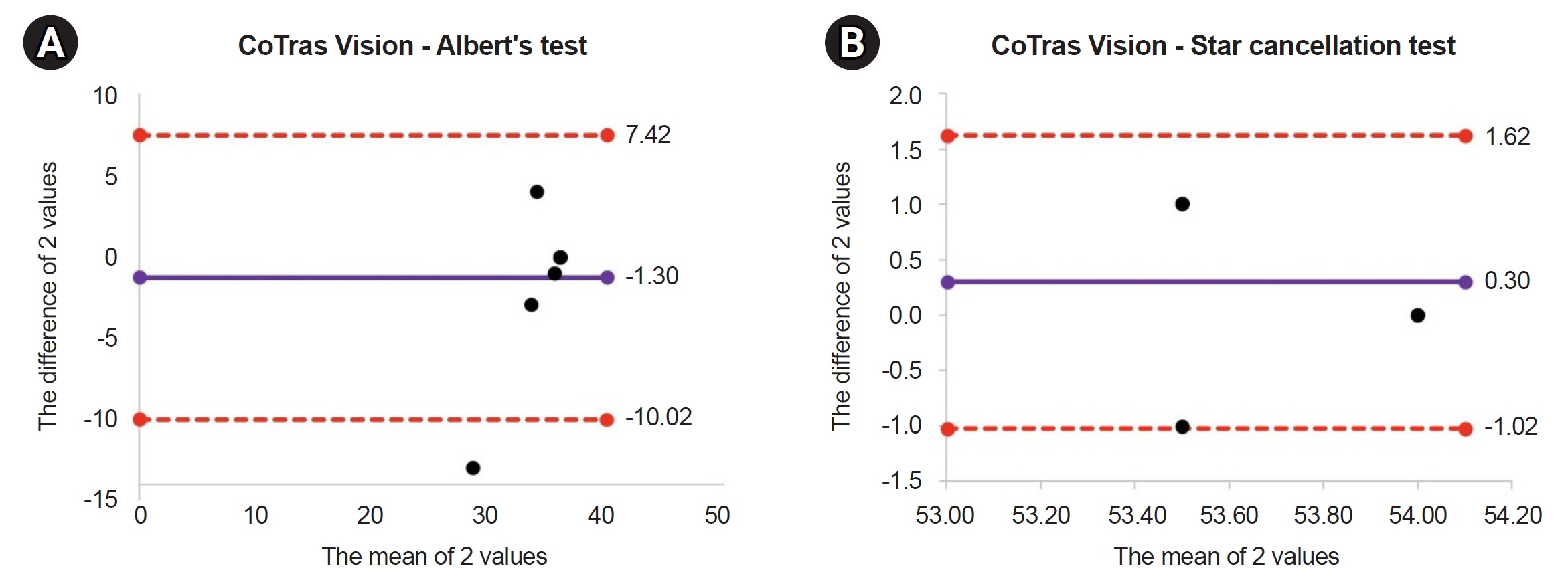
The CoTras Vision system included two evaluations and four training modules. The evaluation modules were based on the Albert’s test and Star cancellation test, and training modules were based on visual tracking, central-peripheral integration, and visuomotor perception techniques. Bland–Altman plots for agreement with the traditional paper-and-pencil test were performed, and the modified Intrinsic Motivation Inventory, Patient Satisfaction Questionnaire, and Simulator Sickness Questionnaire were conducted.
Results
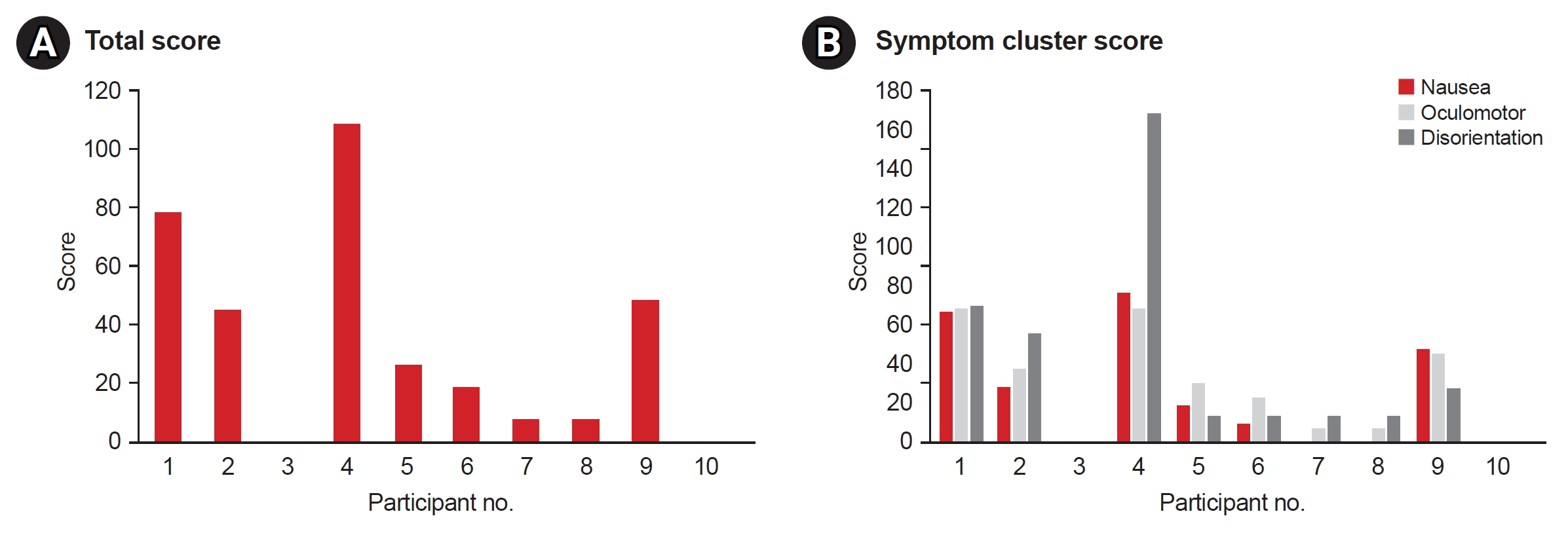
Ten patients with acute stroke completed the study. Bland–Altman plots revealed good agreements for Albert’s test (mean difference, -0.3±4.5) and Star cancellation test (mean difference, 0.3±0.7). The mean±standard deviation scores of the modified Intrinsic Motivation Inventory, Patient Satisfaction Survey, and Simulator Sickness Questionnaire were 84.7±30.6, 40.5±7.9, and 34.0±34.5 respectively.
Conclusion
The CoTras Vision system is feasible and safe in patients with stroke. Most patients had a high degree of motivation to use the system and did not experience severe adverse events. Further studies are needed to confirm its usefulness in stroke patients with visual field defects and hemineglect symptoms. Furthermore, a large, well-designed, randomized controlled trial will be needed to confirm the treatment effect of the CoTras Vision system.
Figure
Reference
-
1. Katan M, Luft A. Global burden of stroke. Semin Neurol. 2018; 38:208–11.
Article2. Rowe FJ, Hepworth LR, Howard C, Hanna KL, Currie J. Impact of visual impairment following stroke (IVIS study): a prospective clinical profile of central and peripheral visual deficits, eye movement abnormalities and visual perceptual deficits. Disabil Rehabil. 2022; 44:3139–53.
Article3. Bouwmeester L, Heutink J, Lucas C. The effect of visual training for patients with visual field defects due to brain damage: a systematic review. J Neurol Neurosurg Psychiatry. 2007; 78:555–64.
Article4. Matteo BM, Viganò B, Cerri CG, Perin C. Visual field restorative rehabilitation after brain injury. J Vis. 2016; 16:11.
Article5. Urbanski M, Thiebaut de Schotten M, Rodrigo S, Oppenheim C, Touzé E, Méder JF, et al. DTI-MR tractography of white matter damage in stroke patients with neglect. Exp Brain Res. 2011; 208:491–505.
Article6. Rowe F; VIS Group UK. Symptoms of stroke-related visual impairment. Strabismus. 2013; 21:150–4.
Article7. Hepworth L, Rowe F. Visual Impairment following stroke - the impact on quality of life: a systematic review. Ophthalmol Res Int J. 2016; 5:1–15.
Article8. Berger S, Kaldenberg J, Selmane R, Carlo S. Effectiveness of interventions to address visual and visual-perceptual impairments to improve occupational performance in adults with traumatic brain injury: a systematic review. Am J Occup Ther. 2016; 70:7003180010p1-7.
Article9. Zeltzer L, Menon A. Albert’s test [Internet]. STROKE ENGINE team;2010 [cited 2023 Apr 16]. Available from: https://strokengine.ca/en/assessments/alberts-test/.10. Zeltzer L, Menon A. Line bisection test [Internet]. STROKE ENGINE team;2008 [cited 2023 Apr 16]. Available from: https://strokengine.ca/en/assessments/line-bisection-test/.11. Anderson L, Cross A, Wynthein D, Schmidt L, Grutz K. Effects of Dynavision training as a preparatory intervention status postcerebrovascular accident: a case report. Occup Ther Health Care. 2011; 25:270–82.
Article12. Jutai JW, Bhogal SK, Foley NC, Bayley M, Teasell RW, Speechley MR. Treatment of visual perceptual disorders post stroke. Top Stroke Rehabil. 2003; 10:77–106.
Article13. El Nahas N, Elbokl AM, Abd Eldayem EH, Roushdy TM, Amin RM, Helmy SM, et al. Navigated perilesional transcranial magnetic stimulation can improve post-stroke visual field defect: a double-blind sham-controlled study. Restor Neurol Neurosci. 2021; 39:199–207.
Article14. Gartz R, Dickerson A, Radloff JC. Comparing component-based and occupation-based interventions of a person with visual deficits’ performance. Occup Ther Health Care. 2021; 35:40–56.
Article15. Pratviel Y, Deschodt-Arsac V, Larrue F, Arsac LM. Reliability of the Dynavision task in virtual reality to explore visuomotor phenotypes. Sci Rep. 2021; 11:587.
Article16. Jang HJ, Choi YD, Kim NH. Effects and satisfaction of medical device safety information reporting system using electronic medical record. Healthc Inform Res. 2017; 23:94–100.
Article17. Sahraie A, Smania N, Zihl J. Use of NeuroEyeCoach™ to improve eye movement efficacy in patients with homonymous visual field loss. Biomed Res Int. 2016; 2016:5186461.
Article18. Varela-Aldás J, Buele J, Ramos Lorente P, García-Magariño I, Palacios-Navarro G. A virtual reality-based cognitive telerehabilitation system for use in the COVID-19 pandemic. Sustainability. 2021; 13:2183.
Article19. King M, Hijmans JM, Sampson M, Satherley J, Hale L. Home-based stroke rehabilitation using computer gaming. NZ J Physiother. 2012; 40:128–34.20. Beattie PF, Pinto MB, Nelson MK, Nelson R. Patient satisfaction with outpatient physical therapy: instrument validation. Phys Ther 2002;82:557-65. Erratum in: Phys Ther. 2002; 82:827.21. Kennedy RS, Lane NE, Berbaum KS, Lilienthal MG. Simulator Sickness Questionnaire: an enhanced method for quantifying simulator sickness. Int J Aviat Psychol. 1993; 3:203–20.
Article22. Zeltzer L, Menon A. Star cancellation test [Internet]. STROKE ENGINE team;2008 [cited 2023 Apr 16]. Available from: https://strokengine.ca/en/assessments/star-cancellation-test/.23. Mannan MMN, Kamran MA, Kang S, Choi HS, Jeong MY. A hybrid speller design using eye tracking and SSVEP brain-computer interface. Sensors (Basel). 2020; 20:891.
Article24. Stanney KM, Kennedy RS, Drexler JM. Cybersickness is not simulator sickness. Proc Hum Factors Ergon Soc Annu Meet. 1997; 41:1138–42.
Article25. Bimberg P, Weissker T, Kulik A. On the usage of the Simulator Sickness Questionnaire for virtual reality research. Paper presented at: 2020 IEEE Conference on Virtual Reality and 3D User Interfaces Abstracts and Workshops (VRW); 2020 Mar 22-26; Atlanta, USA.26. Circle Peripheral Awareness. Eye Cam Learn. Tracking: central-peripheral integration [Internet]. Circle Peripheral Awareness;2014 [cited 2023 Apr 16]. Available from: https://eyecanlearn.com/tracking/peripheral/.27. Rusconi ML, Meinecke C, Sbrissa P, Bernardini B. Different cognitive trainings in the rehabilitation of visuo-spatial neglect. Eur J Phys Rehabil Med. 2002; 38:159–66.28. Moon SJ, Park CH, Jung SI, Yu JW, Son EC, Lee HN, et al. Effects of an eye-tracking linkage attention training system on cognitive function compared to conventional computerized cognitive training system in patients with stroke. Healthcare (Basel). 2022; 10:456.
Article29. Choi SY, Han SW, Lee JS. The effect of Dynavision training on visual attention during task after stroke: single subject research design. Korean J Occup Ther. 2015; 23:1–13.30. Pouget MC, Lévy-Bencheton D, Prost M, Tilikete C, Husain M, Jacquin-Courtois S. Acquired visual field defects rehabilitation: critical review and perspectives. Ann Phys Rehabil Med. 2012; 55:53–74.
Article31. Mueller I, Mast H, Sabel BA. Recovery of visual field defects: a large clinical observational study using vision restoration therapy. Restor Neurol Neurosci. 2007; 25:563–72.32. Aimola L, Lane AR, Smith DT, Kerkhoff G, Ford GA, Schenk T. Efficacy and feasibility of home-based training for individuals with homonymous visual field defects. Neurorehabil Neural Repair. 2014; 28:207–18.
Article33. van Kessel ME, Geurts AC, Brouwer WH, Fasotti L. Visual scanning training for neglect after stroke with and without a computerized lane tracking dual task. Front Hum Neurosci. 2013; 7:358.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relationship between Comorbid Cognitive Impairment and Functional Outcomes in Stroke Patients with Spatial Neglect
- Subtypes of Spatial Neglect and Assessment
- Neuroanatomy of Unilateral Neglect Syndrome
- Effect of Computer-based Cognitive Rehabilitation on Unilateral Spatial Neglect in Stroke Patients
- Visual Field Defects and Disc Findings in Glaucoma