Ann Surg Treat Res.
2024 Apr;106(4):203-210. 10.4174/astr.2024.106.4.203.
Outcomes of bilateral axillo-breast approach robotic parathyroidectomy versus open parathyroidectomy for primary hyperparathyroidism: a single-institution retrospective study
- Affiliations
-
- 1Department of Surgery, Seoul National University Bundang Hospital, Seongnam, Korea
- 2Deprtment of Surgery, Icahn School of Medicine at Mount Sinai, The Mount Sinai Hospital, New York, NY, USA
- 3Department of Surgery, Seoul National University Hospital, Seoul, Korea
- 4Department of Surgery, Seoul National University College of Medicine, Seoul, Korea
- 5Cancer Research Institute, Seoul National University College of Medicine, Seoul, Korea
- 6Department of Surgery, Seoul National University Boramae Medical Center, Seoul, Korea
- KMID: 2554479
- DOI: http://doi.org/10.4174/astr.2024.106.4.203
Abstract
- Purpose
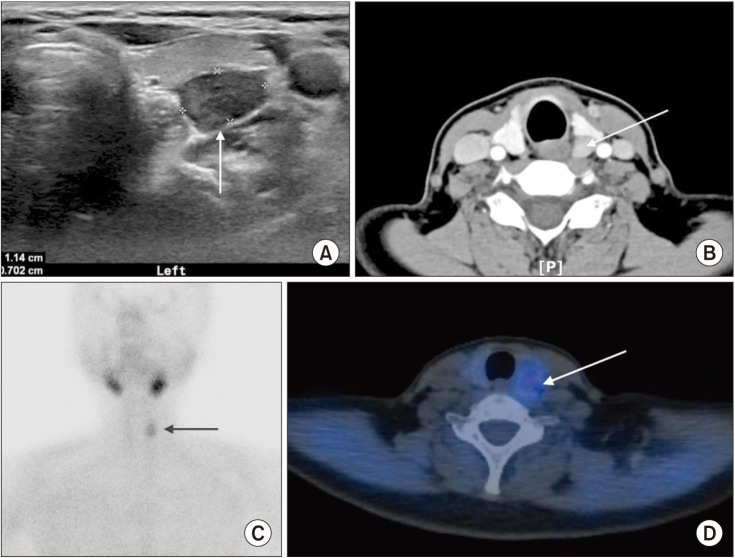
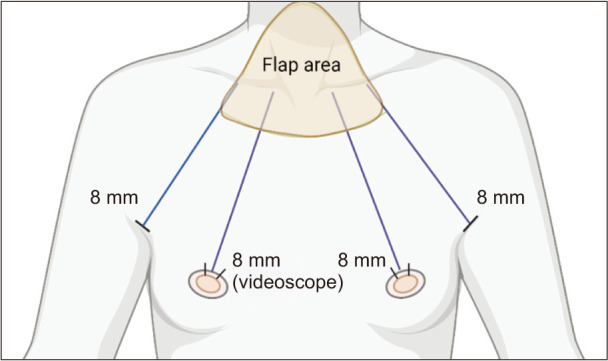
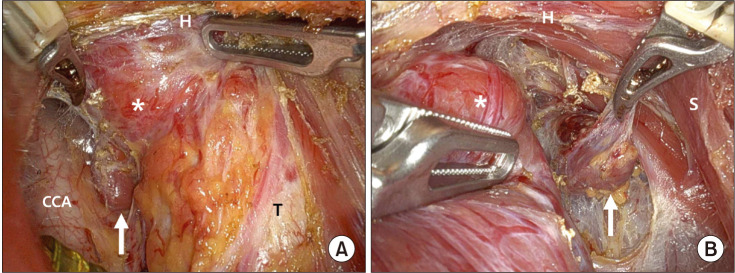
Bilateral axillo-breast approach robotic parathyroidectomy (BABA-RP) aims to remove overactive or enlarged parathyroid glands with no visible neck collar incision. In this study, we compared the safety and surgical outcomes of BABA-RP vs. those of an open surgery group to ascertain whether BABA-RP is a safe and feasible surgical approach for patients with primary hyperparathyroidism (pHPT).
Methods
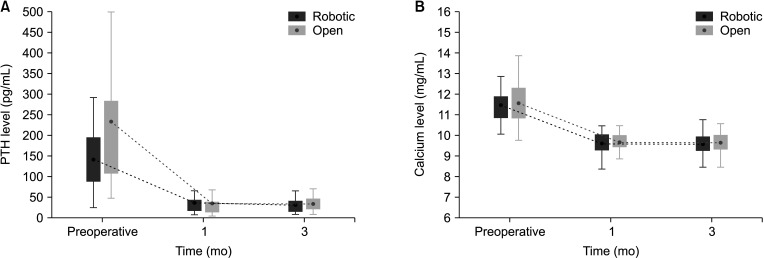
This single-institution retrospective cohort study included 74 patients with primary HPT who underwent open parathyroidectomy (n = 37) or BABA-RP (n = 37) at our institution between November 2014 and March 2023. Patient demographics, biochemical cure rates, operative time, blood loss rates, and complication rates were examined and compared.
Results
The patients in the BABA-RP group were younger and had a longer mean operative time. Regarding complication events, 2 patients in the open surgery group and 1 patient in the BABA-RP group had transient hypoparathyroidism. All 74 patients achieved biochemical cure at <6 months, regardless of the approach used. Two patients in the BABA-RP group and 1 patient in the open surgery group had carcinoma on surgical pathology. All 3 patients with parathyroid carcinoma remained recurrence-free at 1-year follow-up.
Conclusion
Compared with the open procedure, BABA-RP is a safe and feasible procedure that provides an excellent biochemical cure rate for patients with pHPT and has superior cosmetic benefits with equivalent surgical outcomes.
Figure
Reference
-
1. Yeh MW, Ituarte PH, Zhou HC, Nishimoto S, Liu IL, Harari A, et al. Incidence and prevalence of primary hyperparathyroidism in a racially mixed population. J Clin Endocrinol Metab. 2013; 98:1122–1129. PMID: 23418315.2. Wilhelm SM, Wang TS, Ruan DT, Lee JA, Asa SL, Duh QY, et al. The American Association of Endocrine Surgeons guidelines for definitive management of primary hyperparathyroidism. JAMA Surg. 2016; 151:959–968. PMID: 27532368.3. Zhu CY, Sturgeon C, Yeh MW. Diagnosis and management of primary hyperparathyroidism. JAMA. 2020; 323:1186–1187. PMID: 32031566.4. Delbridge LW, Palazzo FF. First parathyroid surgeon: Sir John Bland-Sutton and the parathyroids. ANZ J Surg. 2007; 77:1058–1061. PMID: 17973666.5. Udelsman R, Donovan PI. Open minimally invasive parathyroid surgery. World J Surg. 2004; 28:1224–1226. PMID: 15517494.6. Russell C. Unilateral neck exploration for primary hyperparathyroidism. Surg Clin North Am. 2004; 84:705–716. PMID: 15145229.7. Agarwal G, Barraclough BH, Reeve TS, Delbridge LW. Minimally invasive parathyroidectomy using the 'focused' lateral approach. II. Surgical technique. ANZ J Surg. 2002; 72:147–151. PMID: 12074068.8. Kandil E, Attia AS, Hadedeya D, Shihabi A, Elnahla A. Robotic thyroidectomy: past, future, and current perspectives. Otolaryngol Clin North Am. 2020; 53:1031–1039. PMID: 33127039.9. Kandil E, Hadedeya D, Shalaby M, Toraih E, Aparício D, Garstka M, et al. Robotic-assisted parathyroidectomy via transaxillary approach: feasibility and learning curves. Gland Surg. 2021; 10:953–960. PMID: 33842239.10. Mohamed HE, Bhatia P, Aslam R, Moulthrop T, Kandil E. Robotic transaxillary and retroauricular parathyroid surgery. Gland Surg. 2015; 4:420–428. PMID: 26425455.11. Tolley N, Arora A, Palazzo F, Garas G, Dhawan R, Cox J, et al. Robotic-assisted parathyroidectomy: a feasibility study. Otolaryngol Head Neck Surg. 2011; 144:859–866. PMID: 21546590.12. He Q, Zhu J, Zhuang D, Fan Z. Robotic total parathyroidectomy by the axillo-bilateral-breast approach for secondary hyperparathyroidism: a feasibility study. J Laparoendosc Adv Surg Tech A. 2015; 25:311–313. PMID: 25760735.13. Lee KE, Choi JY, Youn YK. Bilateral axillo-breast approach robotic thyroidectomy. Surg Laparosc Endosc Percutan Tech. 2011; 21:230–236. PMID: 21857470.14. Kwak J, Yu HW, Ahn JH, Kim SJ, Chai YJ, Choi JY, et al. A time trend analysis of 5,000 robotic thyroidectomies via bilateral axillo-breast approach. World J Surg. 2023; 47:403–411. PMID: 36525062.15. Lee KE, Rao J, Youn YK. Endoscopic thyroidectomy with the da Vinci robot system using the bilateral axillary breast approach (BABA) technique: our initial experience. Surg Laparosc Endosc Percutan Tech. 2009; 19:e71–e75. PMID: 19542833.16. Choi JY, Yu HW, Bae IE, Kim JK, Seong CY, Yi JW, et al. Novel method to save the parathyroid gland during thyroidectomy: Subcapsular saline injection. Head Neck. 2018; 40:801–807. PMID: 29356201.17. Soomro NA, Hashimoto DA, Porteous AJ, Ridley CJ, Marsh WJ, Ditto R, et al. Systematic review of learning curves in robot-assisted surgery. BJS Open. 2020; 4:27–44. PMID: 32011823.18. Catchpole K, Perkins C, Bresee C, Solnik MJ, Sherman B, Fritch J, et al. Safety, efficiency and learning curves in robotic surgery: a human factors analysis. Surg Endosc. 2016; 30:3749–3761. PMID: 26675938.19. Higgins KM, Mandell DL, Govindaraj S, Genden EM, Mechanick JI, Bergman DA, et al. The role of intraoperative rapid parathyroid hormone monitoring for predicting thyroidectomy-related hypocalcemia. Arch Otolaryngol Head Neck Surg. 2004; 130:63–67. PMID: 14732770.20. Orloff LA, Wiseman SM, Bernet VJ, Fahey TJ, Shaha AR, Shindo ML, et al. American Thyroid Association statement on postoperative hypoparathyroidism: diagnosis, prevention, and management in adults. Thyroid. 2018; 28:830–841. PMID: 29848235.21. Busaidy NL, Jimenez C, Habra MA, Schultz PN, El-Naggar AK, Clayman GL, et al. Parathyroid carcinoma: a 22-year experience. Head Neck. 2004; 26:716–726. PMID: 15287039.22. Harari A, Waring A, Fernandez-Ranvier G, Hwang J, Suh I, Mitmaker E, et al. Parathyroid carcinoma: a 43-year outcome and survival analysis. J Clin Endocrinol Metab. 2011; 96:3679–3686. PMID: 21937626.23. Choe JH, Kim SW, Chung KW, Park KS, Han W, Noh DY, et al. Endoscopic thyroidectomy using a new bilateral axillo-breast approach. World J Surg. 2007; 31:601–606. PMID: 17308853.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nonfunctioning Parathyromatosis after Endoscopic Thyroid Lobectomy via an Axillo-Breast Approach: A Case Report
- Minimally Invasive Parathyroidectomy without an Intraoperative i-PTH Test for Patients with Primary Hyperparathyroidism
- Subtotal Parathyroidectomy for Tertiary Hyperparathyroidism: a Case Report and Literature Review
- Bilateral axillo-breast approach robotic total thyroidectomy without isthmectomy: a case report
- Surgical Experience of Primary Hyperparathyroidism: Analysis of Postoperative Outcomes