Ann Surg Treat Res.
2024 Apr;106(4):189-194. 10.4174/astr.2024.106.4.189.
Safe and successful pregnancy following breast cancer treatment in young patients 35 years old or under without invasive fertility preservation: a retrospective study
- Affiliations
-
- 1Department of Breast and Endocrine Surgery, Korea University Guro Hospital, Korea University College of Medicine, Seoul, Korea
- KMID: 2554477
- DOI: http://doi.org/10.4174/astr.2024.106.4.189
Abstract
- Purpose
Recent advances in the treatment of breast cancer have led to the improvement of breast cancer patient’s survival. With the prolonged survival of these patients, pregnancy became an important issue, especially in young cancer patient aged 35 years or under. Increased hormone levels during pregnancy, however, raise concerns about elevating the risk of cancer recurrence. The aim of this study was to validate the notion of increased risk associated with pregnancy after breast cancer treatment in young patients.
Methods
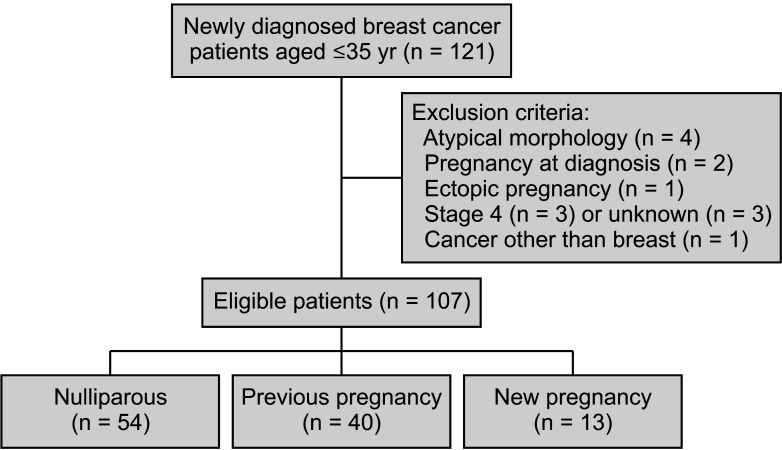
From January 2009 to December 2020, newly diagnosed breast cancer patients 35 years old or under who underwent optimal surgery in Korea University Guro Hospital were enrolled in this study. Patients were categorized into 3 groups: nulliparous, pregnancy prior to treatment of breast cancer, and patients with pregnancy after breast cancer treatment. Their overall survival and disease-free survival were evaluated.
Results
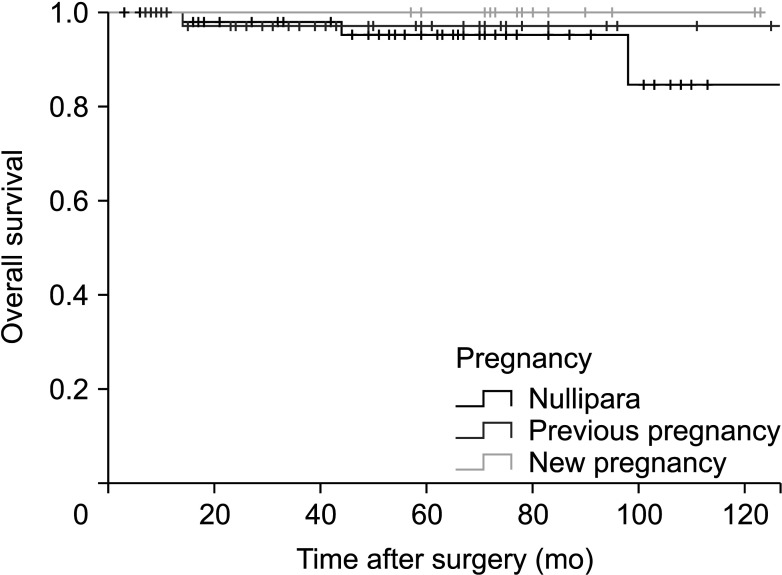
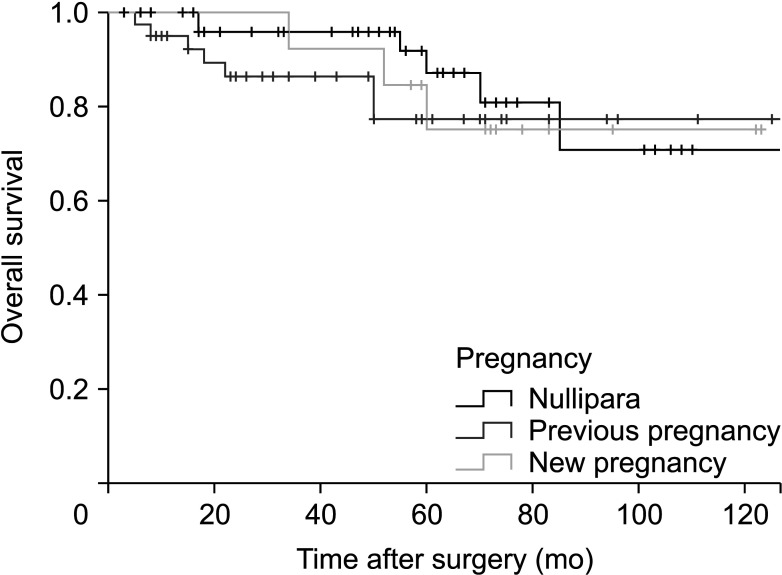
A total of 107 patients were enrolled in this study. Thirteen patients (12.1%) conceived and successfully delivered. The mean follow-up period after surgery was 58.9 (± 33.5) months. There was no significant difference in overall survival (P = 0.608) and disease-free survival (P = 0.591) among different groups.
Conclusion
In young patients, pregnancy after treatment for breast cancer did not affect their overall survival or diseasefree survival as compared to nullipara or previously delivered groups. Therefore, pregnancy counseling should not be prevented in young breast cancer patients 35 years old or under.
Keyword
Figure
Reference
-
1. Lee MH, Kim YA, Hong JH, Jung SY, Lee S, Kong SY, et al. Outcomes of pregnancy after breast cancer in Korean women: a large cohort study. Cancer Res Treat. 2020; 52:426–437. PMID: 31476846.2. de la Rochefordiere A, Asselain B, Campana F, Scholl SM, Fenton J, Vilcoq JR, et al. Age as prognostic factor in premenopausal breast carcinoma. Lancet. 1993; 341:1039–1043. PMID: 8096955.3. Han W, Kim SW, Park IA, Kang D, Kim SW, Youn YK, et al. Young age: an independent risk factor for disease-free survival in women with operable breast cancer. BMC Cancer. 2004; 4:82. PMID: 15546499.4. Wang SS, Loong H, Chung JP, Yeo W. Preservation of fertility in premenopausal patients with breast cancer. Hong Kong Med J. 2020; 26:216–226. PMID: 32482909.5. Llarena NC, Estevez SL, Tucker SL, Jeruss JS. Impact of fertility concerns on tamoxifen initiation and persistence. J Natl Cancer Inst. 2015; 107:djv202. PMID: 26307641.6. Anderson PR, Hanlon AL, Freedman GM, Nicolaou N. Parity confers better prognosis in older women with early-stage breast cancer treated with breast-conserving therapy. Clin Breast Cancer. 2004; 5:225–231. PMID: 15335456.7. Papatestas AE, Mulvihill M, Josi C, Ioannovich J, Lesnick G, Aufses AH. Parity and prognosis in breast cancer. Cancer. 1980; 45:191–194. PMID: 7351001.8. Phillips KA, Milne RL, Friedlander ML, Jenkins MA, McCredie MR, Giles GG, et al. Prognosis of premenopausal breast cancer and childbirth prior to diagnosis. J Clin Oncol. 2004; 22:699–705. PMID: 14966094.9. Rosenberg L, Thalib L, Adami HO, Hall P. Childbirth and breast cancer prognosis. Int J Cancer. 2004; 111:772–776. PMID: 15252849.10. Sun X, Nichols HB, Tse CK, Bell MB, Robinson WR, Sherman ME, et al. Association of parity and time since last birth with breast cancer prognosis by intrinsic subtype. Cancer Epidemiol Biomarkers Prev. 2016; 25:60–67. PMID: 26545404.11. Luo M, Zeng J, Li F, He L, Li T. Safety of pregnancy after surgical treatment for breast cancer: a meta-analysis. Int J Gynecol Cancer. 2014; 24:1366–1372. PMID: 25188887.12. Lambertini M, Kroman N, Ameye L, Cordoba O, Pinto A, Benedetti G, et al. Long-term safety of pregnancy following breast cancer according to estrogen receptor status. J Natl Cancer Inst. 2018; 110:426–429. PMID: 29087485.13. Carneiro MM, Cota AM, Amaral MC, Pedrosa ML, Martins BO, Furtado MH, et al. Motherhood after breast cancer: can we balance fertility preservation and cancer treatment? A narrative review of the literature. JBRA Assist Reprod. 2018; 22:244–252. PMID: 29932615.14. Petrek JA. Pregnancy safety after breast cancer. Cancer. 1994; 74:528–531. PMID: 8004628.15. Sankila R, Heinävaara S, Hakulinen T. Survival of breast cancer patients after subsequent term pregnancy: "healthy mother effect". Am J Obstet Gynecol. 1994; 170:818–823. PMID: 8141209.16. Ives A, Saunders C, Bulsara M, Semmens J. Pregnancy after breast cancer: population based study. BMJ. 2007; 334:194. PMID: 17158581.17. Partridge AH, Niman SM, Ruggeri M, Peccatori FA, Azim HA Jr, Colleoni M, et al. Interrupting endocrine therapy to attempt pregnancy after breast cancer. N Engl J Med. 2023; 388:1645–1656. PMID: 37133584.18. Bouferraa Y, Haibe Y, Chedid A, Jabra E, Charafeddine M, Temraz S, et al. The impact of young age (< 40 years) on the outcome of a cohort of patients with primary non-metastatic breast cancer: analysis of 10-year survival of a prospective study. BMC Cancer. 2022; 22:27. PMID: 34980002.19. Assi HA, Khoury KE, Dbouk H, Khalil LE, Mouhieddine TH, El Saghir NS. Epidemiology and prognosis of breast cancer in young women. J Thorac Dis. 2013; 5 Suppl 1:S2–S8. PMID: 23819024.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Controlled ovarian hyperstimulation for fertility preservation in women with breast cancer: Practical issues
- Fertility Preservation in Young Women With Breast Cancer: A Review
- Fertility preservation for patients with breast cancer: The Korean Society for Fertility Preservation clinical guidelines
- Current Practices toward Fertility Issues for Young Breast Cancer Patients: A Survey of the Korean Breast Cancer Society; The SMARTSHIP Study
- Cancer and Male Infertility