J Korean Med Sci.
2024 Apr;39(12):e118. 10.3346/jkms.2024.39.e118.
Incidence of Clostridioides difficile Infections in Republic of Korea: A Prospective Study With Active Surveillance vs. National Data From Health Insurance Review & Assessment Service
- Affiliations
-
- 1Department of Internal Medicine, Hanyang University College of Medicine, Seoul, Korea
- 2Department of Non-benefits Management, National Health Insurance Service, Wonju, Korea
- 3Hanyang University Guri Hospital, Guri, Korea
- 4Divison of Infectious Diseases, Department of Internal Medicine, Soonchunhyang University Bucheon Hospital, Bucheon, Korea
- 5Department of Internal Medicine, Kyung Hee University College of Medicine, Seoul, Korea
- 6Department of Infectious Diseases, Chonnam National University Medical School, Gwangju, Korea
- 7Division of Infectious Diseases, Department of Internal Medicine, Korea University Ansan Hospital, Ansan, Korea
- 8Division of Infectious Diseases, Chungnam National University School of Medicine, Daejeon, Korea
- 9Department of Internal Medicine and Research Institute of Clinical Medicine, Jeonbuk National University Medical School and Hospital, Jeonju, Korea
- 10Department of Internal Medicine, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea
- 11Department of Internal Medicine, Pusan National University School of Medicine, Busan, Korea
- 12Division of Infectious Diseases, Department of Internal Medicine, School of Medicine, Kyungpook National University, Daegu, Korea
- 13Division of Infectious Diseases, Department of Internal Medicine, Hallym University, Chuncheon Sacred Heart Hospital, Hallym University College of Medicine, Chuncheon, Korea
- 14Department of Internal Medicine, Ewha Womans University College of Medicine, Seoul, Korea
- 15Department of Infectious Diseases, Daegu Fatima Hospital, Daegu, Korea
- 16Department of Infectious Diseases, Bucheon Sejong Hospital, Bucheon, Korea
- 17Division of Infectious Diseases, Samsung Changwon Hospital, Sungkyunkwan University, Changwon, Korea
- 18Division of Infectious Diseases, Dongguk University Ilsan Hospital, Goyang, Korea
- 19Department of Infectious Diseases, International St. Mary’s Hospital, Catholic Kwandong University College of Medicine, Incheon, Korea
- KMID: 2554211
- DOI: http://doi.org/10.3346/jkms.2024.39.e118
Abstract
- Background
Since the emergence of hypervirulent strains of Clostridioides difficile, the incidence of C. difficile infections (CDI) has increased significantly.
Methods
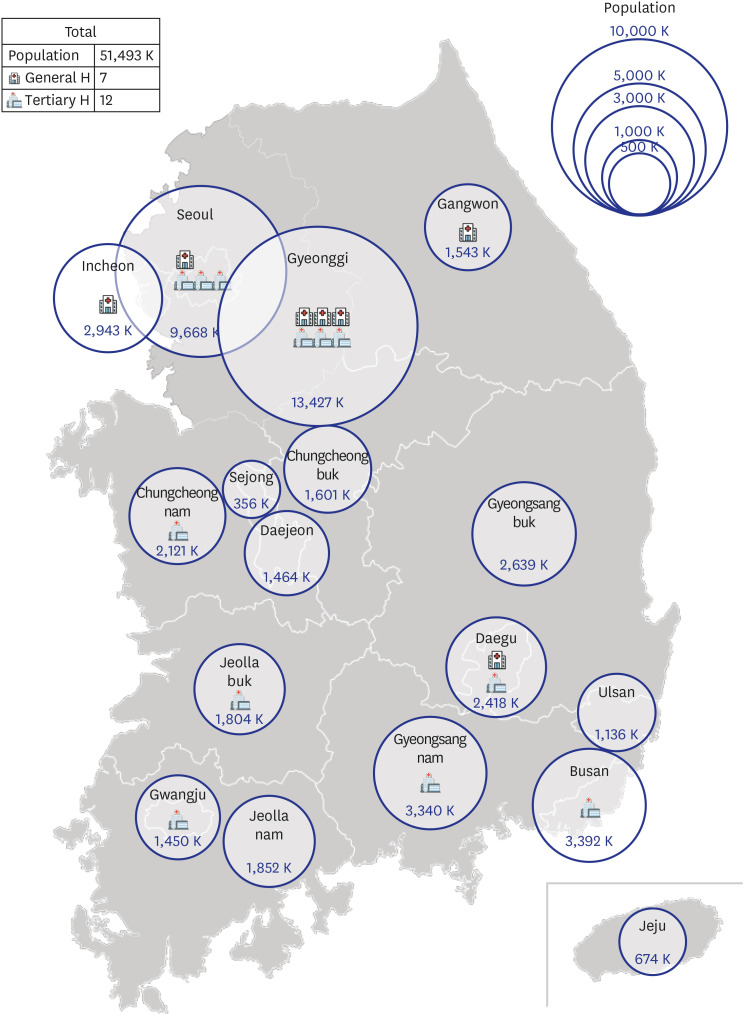
To assess the incidence of CDI in Korea, we conducted a prospective multicentre observational study from October 2020 to October 2021. Additionally, we calculated the incidence of CDI from mass data obtained from the Health Insurance Review and Assessment Service (HIRA) from 2008 to 2020.
Results
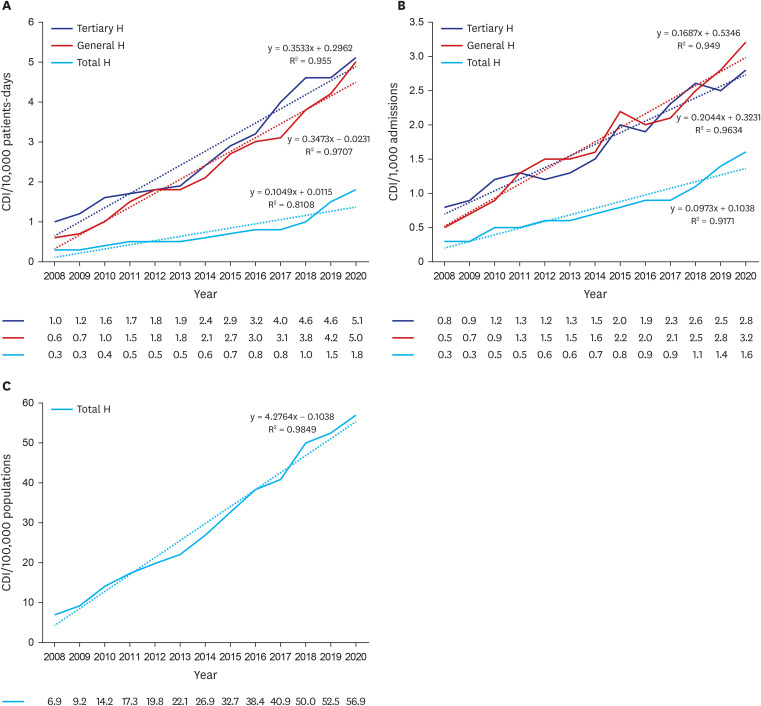
In the prospective study with active surveillance, 30,212 patients had diarrhoea and 907 patients were diagnosed with CDI over 1,288,571 patient-days and 193,264 admissions in 18 participating hospitals during 3 months of study period; the CDI per 10,000 patientdays was 7.04 and the CDI per 1,000 admission was 4.69. The incidence of CDI was higher in general hospitals than in tertiary hospitals: 6.38 per 10,000 patient-days (range: 3.25–12.05) and 4.18 per 1,000 admissions (range: 1.92–8.59) in 11 tertiary hospitals, vs. 9.45 per 10,000 patient-days (range: 5.68–13.90) and 6.73 per 1,000 admissions (range: 3.18–15.85) in seven general hospitals. With regard to HIRA data, the incidence of CDI in all hospitals has been increasing over the 13-year-period: from 0.3 to 1.8 per 10,000 patient-days, 0.3 to 1.6 per 1,000 admissions, and 6.9 to 56.9 per 100,000 population, respectively.
Conclusion
The incidence of CDI in Korea has been gradually increasing, and its recent value is as high as that in the United State and Europe. CDI is underestimated, particularly in general hospitals in Korea.
Figure
Reference
-
1. Martin JS, Monaghan TM, Wilcox MH. Clostridium difficile infection: epidemiology, diagnosis and understanding transmission. Nat Rev Gastroenterol Hepatol. 2016; 13(4):206–216. PMID: 26956066.2. Tschudin-Sutter S, Kuijper EJ, Durovic A, Vehreschild MJ, Barbut F, Eckert C, et al. Guidance document for prevention of Clostridium difficile infection in acute healthcare settings. Clin Microbiol Infect. 2018; 24(10):1051–1054. PMID: 29505879.3. Ho J, Wong SH, Doddangoudar VC, Boost MV, Tse G, Ip M. Regional differences in temporal incidence of Clostridium difficile infection: a systematic review and meta-analysis. Am J Infect Control. 2020; 48(1):89–94. PMID: 31387772.4. Marra AR, Perencevich EN, Nelson RE, Samore M, Khader K, Chiang HY, et al. Incidence and outcomes associated with Clostridium difficile infections: a systematic review and meta-analysis. JAMA Netw Open. 2020; 3(1):e1917597. PMID: 31913488.5. Borren NZ, Ghadermarzi S, Hutfless S, Ananthakrishnan AN. The emergence of Clostridium difficile infection in Asia: a systematic review and meta-analysis of incidence and impact. PLoS One. 2017; 12(5):e0176797. PMID: 28463987.6. Collins DA, Sohn KM, Wu Y, Ouchi K, Ishii Y, Elliott B, et al. Clostridioides difficile infection in the Asia-Pacific region. Emerg Microbes Infect. 2019; 9(1):42–52. PMID: 31873046.7. Kim YS, Han DS, Kim YH, Kim WH, Kim JS, Kim HS, et al. Incidence and clinical features of Clostridium difficile infection in Korea: a nationwide study. Epidemiol Infect. 2013; 141(1):189–194. PMID: 22717061.8. Han SH, Kim H, Lee K, Jeong SJ, Park KH, Song JY, et al. Epidemiology and clinical features of toxigenic culture-confirmed hospital-onset Clostridium difficile infection: a multicentre prospective study in tertiary hospitals of South Korea. J Med Microbiol. 2014; 63(Pt 11):1542–1551. PMID: 25187603.9. Kim J, Pai H, Seo MR, Kang JO. Epidemiology and clinical characteristics of Clostridium difficile infection in a Korean tertiary hospital. J Korean Med Sci. 2011; 26(10):1258–1264. PMID: 22022175.10. Czepiel J, Dróżdż M, Pituch H, Kuijper EJ, Perucki W, Mielimonka A, et al. Clostridium difficile infection. [review]. Eur J Clin Microbiol Infect Dis. 2019; 38(7):1211–1221. PMID: 30945014.11. Kim Y, Chae J, Shin S, Jo G, Shin J, Kim B, et al. Trends in national pharmaceutical expenditure in Korea during 2011–2020. Infect Chemother. 2023; 55(2):237–246. PMID: 37407241.12. Baek JY, Lee E, Jung HW, Jang IY. Geriatrics fact sheet in Korea 2021. Ann Geriatr Med Res. 2021; 25(2):65–71. PMID: 34187140.13. McDonald LC, Gerding DN, Johnson S, Bakken JS, Carroll KC, Coffin SE, et al. Clinical practice guidelines for Clostridium difficile infection in adults and children: 2017 update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin Infect Dis. 2018; 66(7):e1–48. PMID: 29462280.14. Dubberke ER, Carling P, Carrico R, Donskey CJ, Loo VG, McDonald LC, et al. Strategies to prevent Clostridium difficile infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol. 2014; 35(6):628–645. PMID: 24799639.15. Kim JA, Yoon S, Kim LY, Kim DS. Towards actualizing the value potential of Korea Health Insurance Review and Assessment (HIRA) data as a resource for health research: strengths, limitations, applications, and strategies for optimal use of HIRA data. J Korean Med Sci. 2017; 32(5):718–728. PMID: 28378543.16. Choi HY, Park SY, Kim YA, Yoon TY, Choi JM, Choe BK, et al. The epidemiology and economic burden of Clostridium difficile infection in Korea. BioMed Res Int. 2015; 2015:510386. PMID: 25821807.17. Finn E, Andersson FL, Madin-Warburton M. Burden of Clostridioides difficile infection (CDI) - a systematic review of the epidemiology of primary and recurrent CDI. BMC Infect Dis. 2021; 21(1):456. PMID: 34016040.18. Chung HS, Park JS, Shin BM, Yoo HM, Kim H, Cho J, et al. Nationwide survey for current status of laboratory diagnosis of Clostridioides difficile infection in Korea. J Korean Med Sci. 2022; 37(5):e38. PMID: 35132844.19. Gould CV, Edwards JR, Cohen J, Bamberg WM, Clark LA, Farley MM, et al. Effect of nucleic acid amplification testing on population-based incidence rates of Clostridium difficile infection. Clin Infect Dis. 2013; 57(9):1304–1307. PMID: 23899677.20. Kutty PK, Woods CW, Sena AC, Benoit SR, Naggie S, Frederick J, et al. Risk factors for and estimated incidence of community-associated Clostridium difficile infection, North Carolina, USA. Emerg Infect Dis. 2010; 16(2):197–204. PMID: 20113547.21. Khanna S, Pardi DS, Aronson SL, Kammer PP, Orenstein R, St Sauver JL, et al. The epidemiology of community-acquired Clostridium difficile infection: a population-based study. Am J Gastroenterol. 2012; 107(1):89–95. PMID: 22108454.22. Bartlett A, Montgomery A, Hammer K, Singhal S, Lo TS. Does clinician-initiated Clostridioides difficile testing improve outcomes of patients with Clostridioides difficile infection? Am J Infect Control. 2023; 51(10):1085–1088. PMID: 37758340.23. OECD. Health at a Glance 2021. Paris, France: OECD;2021.24. Aloh HE, Onwujekwe OE, Aloh OG, Nweke CJ. Is bed turnover rate a good metric for hospital scale efficiency? A measure of resource utilization rate for hospitals in Southeast Nigeria. Cost Eff Resour Alloc. 2020; 18(1):21. PMID: 32624709.25. Dingle KE, Didelot X, Quan TP, Eyre DW, Stoesser N, Golubchik T, et al. Effects of control interventions on Clostridium difficile infection in England: an observational study. Lancet Infect Dis. 2017; 17(4):411–421. PMID: 28130063.26. Guh AY, Mu Y, Winston LG, Johnston H, Olson D, Farley MM, et al. Trends in U.S. burden of Clostridioides difficile infection and outcomes. N Engl J Med. 2020; 382(14):1320–1330. PMID: 32242357.27. Barker AK, Ngam C, Musuuza JS, Vaughn VM, Safdar N. Reducing Clostridium difficile in the inpatient setting: a systematic review of the adherence to and effectiveness of C. difficile prevention bundles. Infect Control Hosp Epidemiol. 2017; 38(6):639–650. PMID: 28343455.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Trend of Clostridioides difficile Infection in Korean Hospitals with the Analysis of Nationwide Sample Cohort
- Clinical and microbiological risk factors for severe Clostridioides difficile infections in Korea
- Clinical and microbiological risk factors for community-associated Clostridioides difficile infections in Korea
- Changes in the pattern and disease burden of acute respiratory viral infections before and during the COVID-19 pandemic
- Association between Antibiotic Consumption and Incidence of Clostridioides difficile Infection in a Hospital