Korean Circ J.
2024 Mar;54(3):126-137. 10.4070/kcj.2023.0266.
Off-hours Surgery and Mortality in Patients With Type A Aortic Dissection Repair: A Systematic Review and Meta-Analysis
- Affiliations
-
- 1Institute of Medical Sciences, Tzu Chi University, Hualien, Taiwan
- 2Center for Healthy Longevity, Hualien Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, Hualien, Taiwan
- 3Department of Surgery, Hualien Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, Hualien, Taiwan
- 4Department of Surgery, School of Medicine, Tzu Chi University, Hualien, Taiwan
- 5Center for Aging and Health, Hualien Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, Hualien, Taiwan
- 6School of Medicine, Tzu Chi University, Hualien, Taiwan
- 7Department of Family Medicine, Hualien Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, Hualien, Taiwan
- 8Department of Medical Research, Hualien Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, Hualien, Taiwan
- KMID: 2554140
- DOI: http://doi.org/10.4070/kcj.2023.0266
Abstract
- Background and Objectives
The impact of off-hours admission (such as weekends, nighttime, and non-working hours) vs. regular hours (weekdays and daytime working hours) on the mortality risk of patients undergoing surgery for type A aortic dissection (TAAD) repair is still uncertain. To address this uncertainty, we undertook a comprehensive systematic review and meta-analysis. We aimed to assess the potential link between off-hours admission and the risk of mortality in patients undergoing TAAD repair surgery.
Methods
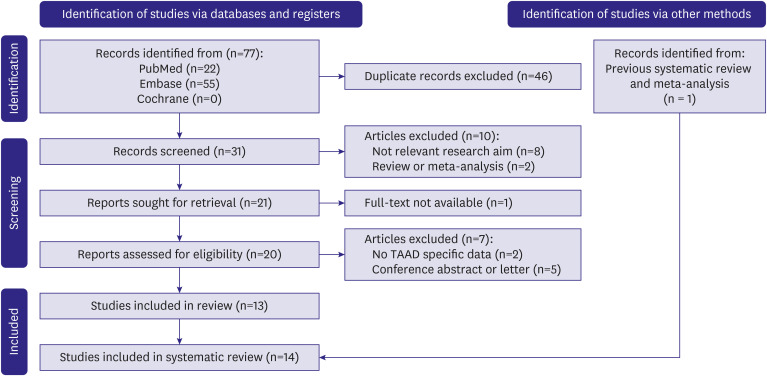
We conducted a thorough search of the PubMed, Embase, and Cochrane Library databases, covering the period from their inception to May 20, 2023. Our inclusion criteria encompassed all studies that examined the potential relationship between off-hour admission and mortality in individuals who had undergone surgery for TAAD repair. The odds ratios (ORs) were extracted and combined utilizing a random effects model for our synthesis.
Results
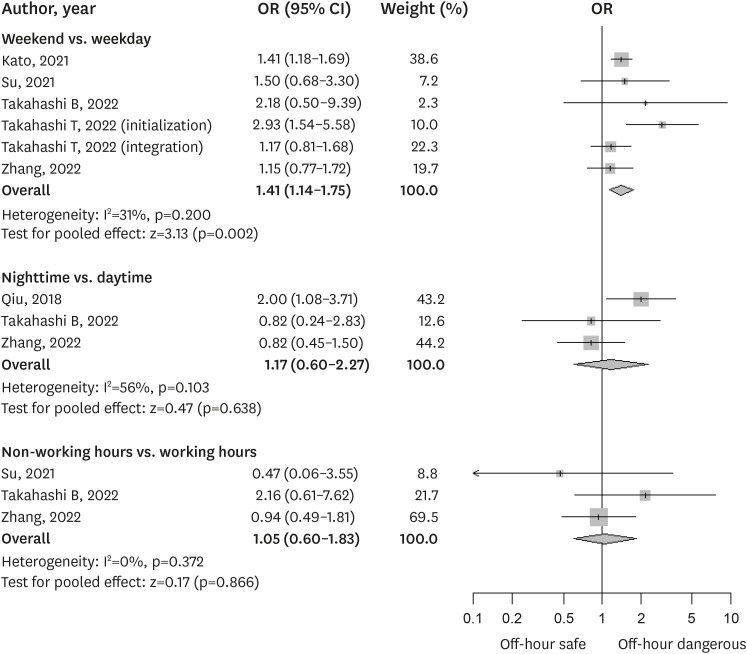
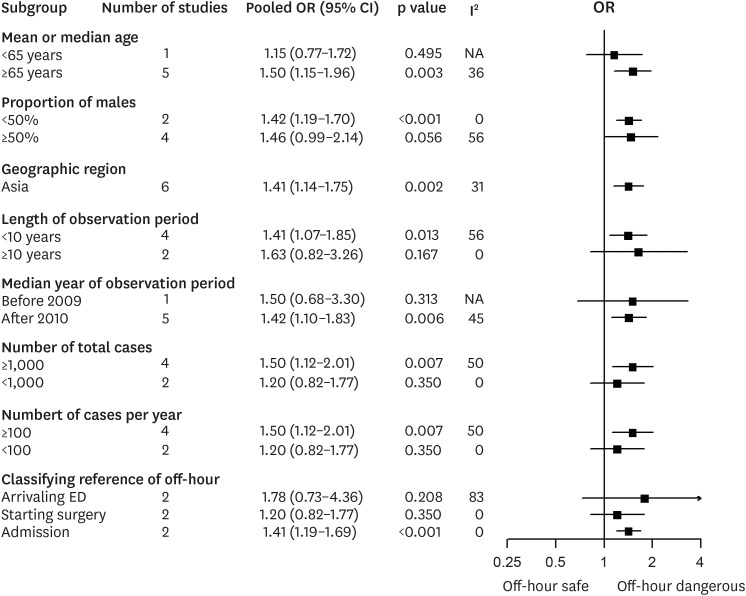
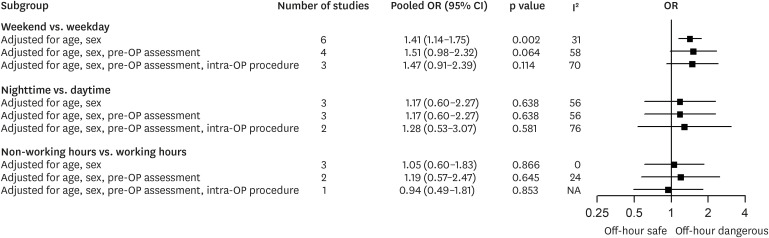
Nine studies with 16,501 patients undergoing TAAD repair surgery were included in the meta-analysis. Overall, patients who underwent surgery during the weekend had higher in-hospital mortality (pooled OR, 1.41; 95% confidence interval [CI], 1.14–1.75; p=0.002) than those treated on weekdays. However, the mortality risks among patients who underwent TAAD surgery during nighttime and non-working hours were not significantly elevated compared to daytime and working hours admission.
Conclusions
Weekend surgery for TAAD was associated with a higher in-hospital mortality risk than weekday surgery. However, further studies are warranted to identify and develop strategies to improve the quality of round-the-clock care for patients with TAAD.
Figure
Reference
-
1. Hiratzka LF, Bakris GL, Beckman JA, et al. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with thoracic aortic disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine. Circulation. 2010; 121:e266–e369. PMID: 20233780.2. Erbel R, Aboyans V, Boileau C, et al. 2014 ESC guidelines on the diagnosis and treatment of aortic diseases: document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. Eur Heart J. 2014; 35:2873–2926. PMID: 25173340.3. Kato K, Otsuka T, Nakai M, Sumita Y, Seino Y, Kawada T. Effect of holiday admission for acute aortic dissection on in-hospital mortality in Japan: a nationwide study. PLoS One. 2021; 16:e0260152. PMID: 34793535.4. Takahashi T, Yoshino H, Akutsu K, et al. In-hospital mortality of patients with acute type a aortic dissection hospitalized on weekends versus weekdays. JACC Asia. 2022; 2:369–381. PMID: 36338400.5. Ahlsson A, Wickbom A, Geirsson A, et al. Is there a weekend effect in surgery for type A dissection? Results from the Nordic consortium for acute type a aortic dissection database. Ann Thorac Surg. 2019; 108:770–776. PMID: 30953648.6. Qiu J, Zhang L, Luo X, et al. Higher mortality in patients undergoing nighttime surgical procedures for acute type A aortic dissection. Ann Thorac Surg. 2018; 106:1164–1170. PMID: 29807008.7. Takahashi B, Kamohara K, Amamoto S, Kawaguchi A. Impact of after-hours surgery on outcomes of acute type A aortic dissection repair. Surg Today. 2022; 52:1453–1462. PMID: 35338427.8. Pupovac SS, Hemli JM, Seetharam K, et al. Acute type A aortic dissection repair after hours: does it influence outcomes? Ann Thorac Surg. 2020; 110:1622–1628. PMID: 32234321.9. Su IM, Huang HK, Liu PP, Hsu JY, Lin SM, Loh CH. Mortality risk from acute aortic dissection among hospital admissions during weekends and holiday season. PLoS One. 2021; 16:e0255942. PMID: 34469438.10. Zhang X, Lv W, Liu X, Liu K, Yang S. Impact of shift work on surgical outcomes at different times in patients with acute type A aortic dissection: a retrospective cohort study. Front Cardiovasc Med. 2022; 9:1000619. PMID: 36386350.11. Toh S, Yew DCM, Choong JJ, Chong TL, Harky A. Acute type A aortic dissection in-hours versus out-of-hours: a systematic review and meta-analysis. J Card Surg. 2020; 35:3432–3439. PMID: 33001480.12. Arnaoutakis G, Bianco V, Estrera AL, et al. Time of day does not influence outcomes in acute type A aortic dissection: results from the IRAD. J Card Surg. 2020; 35:3467–3473. PMID: 32939836.13. Gasser S, Stastny L, Kofler M, et al. Surgery out of office hours for type A aortic dissection: does night-time and weekend surgery worsen outcome? Interact Cardiovasc Thorac Surg. 2020; 31:806–812. PMID: 33001169.14. Harky A, Mason S, Othman A, et al. Outcomes of acute type A aortic dissection repair: daytime versus nighttime. JTCVS Open. 2021; 7:12–20. PMID: 36003743.15. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021; 88:105906. PMID: 33789826.16. Wells G, Shea B, O'Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses [Internet]. Ottawa: Ottawa Hospital Research Institute;2011. cited 2023 May 30. Available from: https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.17. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003; 327:557–560. PMID: 12958120.18. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997; 315:629–634. PMID: 9310563.19. Isaac E, Habib A, Hussain A, Crispi V, Chaudhry M, Loubani M. Does the timing of acute type a aortic dissection surgery impact on immediate and long term patient outcomes? a retrospective single centre study. Clin Surg. 2019; 4:2504.20. Gokalp O, Yilik L, Besir Y, et al. “Overtime hours effect” on emergency surgery of acute type A aortic dissection. Rev Bras Cir Cardiovasc. 2019; 34:680–686.21. Narayan P, Benedetto U, Caputo M, Guida G, Bryan AJ, Angelini GD. Type A acute aortic dissection repair during night time: is it safe? Indian J Thorac Cardiovasc Surg. 2020; 36:114–118. PMID: 33061109.22. Hamilton P, Eschiti VS, Hernandez K, Neill D. Differences between weekend and weekday nurse work environments and patient outcomes: a focus group approach to model testing. J Perinat Neonatal Nurs. 2007; 21:331–341. PMID: 18004171.23. McKee M, Black N. Does the current use of junior doctors in the United Kingdom affect the quality of medical care? Soc Sci Med. 1992; 34:549–558. PMID: 1604361.24. Aujesky D, Jiménez D, Mor MK, Geng M, Fine MJ, Ibrahim SA. Weekend versus weekday admission and mortality after acute pulmonary embolism. Circulation. 2009; 119:962–968. PMID: 19204300.25. Kane RL, Shamliyan TA, Mueller C, Duval S, Wilt TJ. The association of registered nurse staffing levels and patient outcomes: systematic review and meta-analysis. Med Care. 2007; 45:1195–1204. PMID: 18007170.26. Harless DW, Mark BA. Nurse staffing and quality of care with direct measurement of inpatient staffing. Med Care. 2010; 48:659–663. PMID: 20548254.27. Schilling PL, Campbell DA Jr, Englesbe MJ, Davis MM. A comparison of in-hospital mortality risk conferred by high hospital occupancy, differences in nurse staffing levels, weekend admission, and seasonal influenza. Med Care. 2010; 48:224–232. PMID: 20168260.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Repair of Retrograde Type A Aortic Dissection after Thoracic Endovascular Aortic Repair
- Retrograde Aortic Dissection after Thoracic Endovascular Aortic Repair for Descending Aorta: 2 case reports
- A Case of Total Aortic Arch Replacement with Root Plasty with Right Coronary Artery Bypass and Distal Open Stent-graft Insertion in Acute Type I Aortic Dissection
- Short-term Mortality and Postoperative Complications of Abdominal Aortic Aneurysm Repair in Obese versus Non-obese Patients
- Distal Aortic Remodeling after Type A Dissection Repair: An Ongoing Mirage