J Cerebrovasc Endovasc Neurosurg.
2024 Mar;26(1):71-78. 10.7461/jcen.2023.E2023.05.009.
Navigation guided small craniectomy and direct cannulation of pure isolated sigmoid sinus for treatment of dural arteriovenous fistula
- Affiliations
-
- 1Department of Neurosurgery, Soonchunhyang University Cheonan Hospital, Cheonan, Korea
- KMID: 2554049
- DOI: http://doi.org/10.7461/jcen.2023.E2023.05.009
Abstract
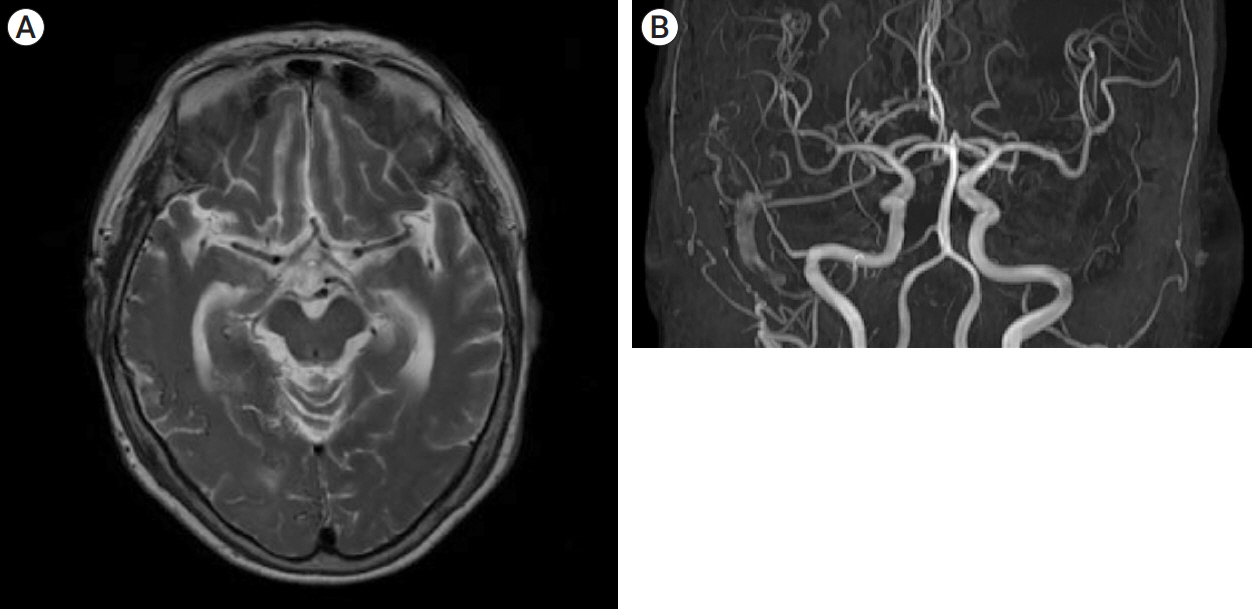
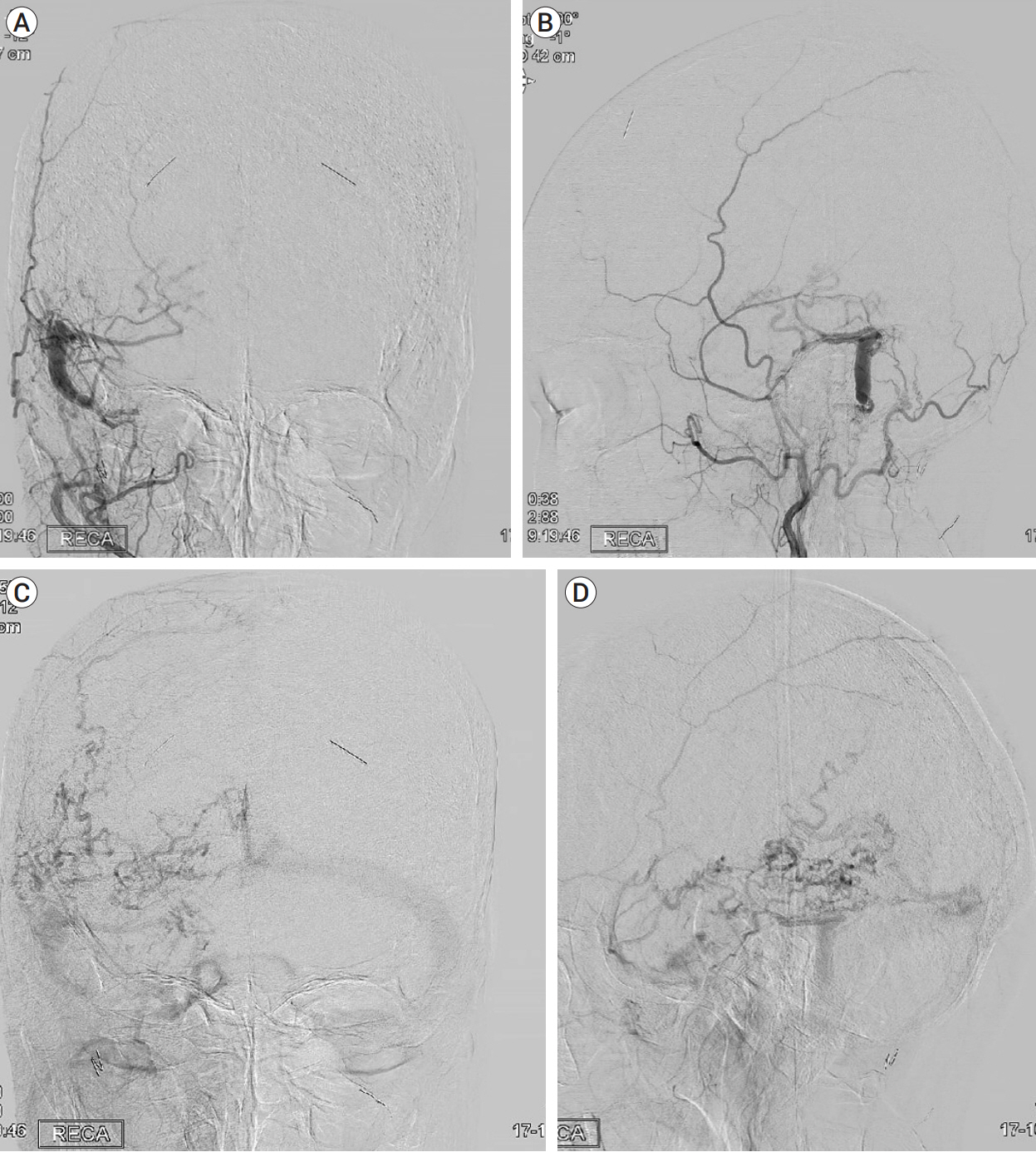
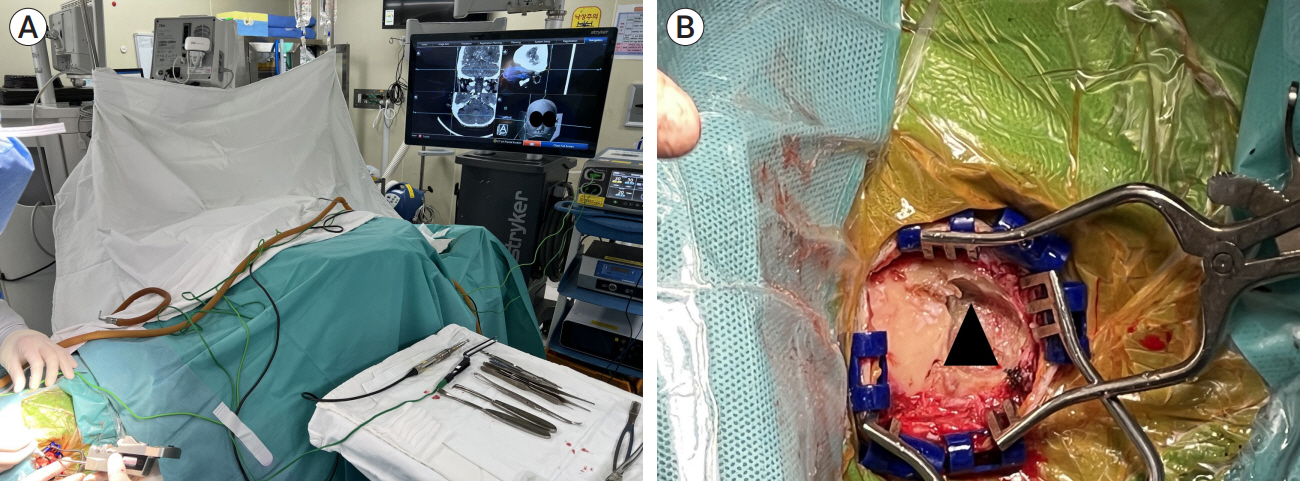
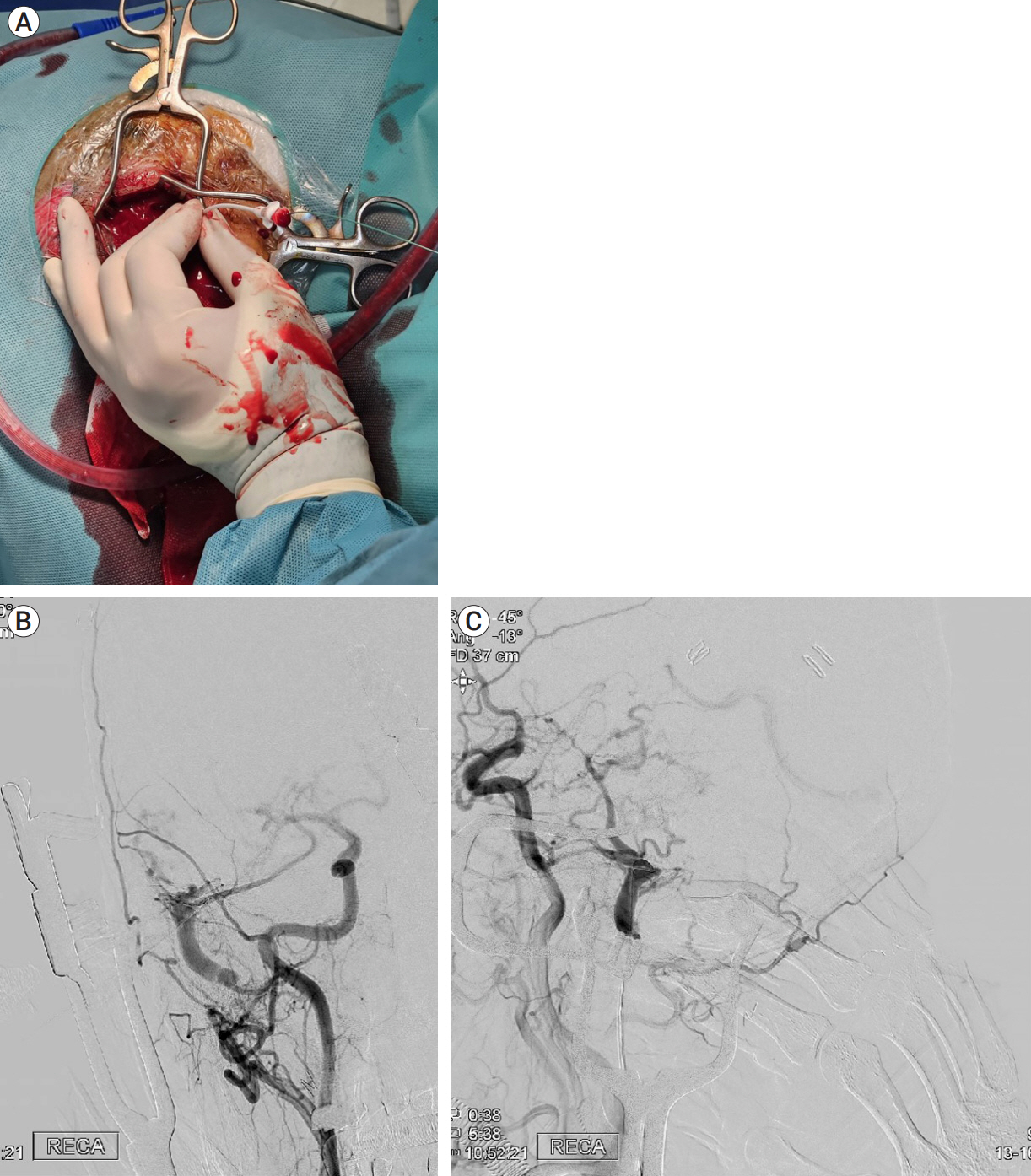
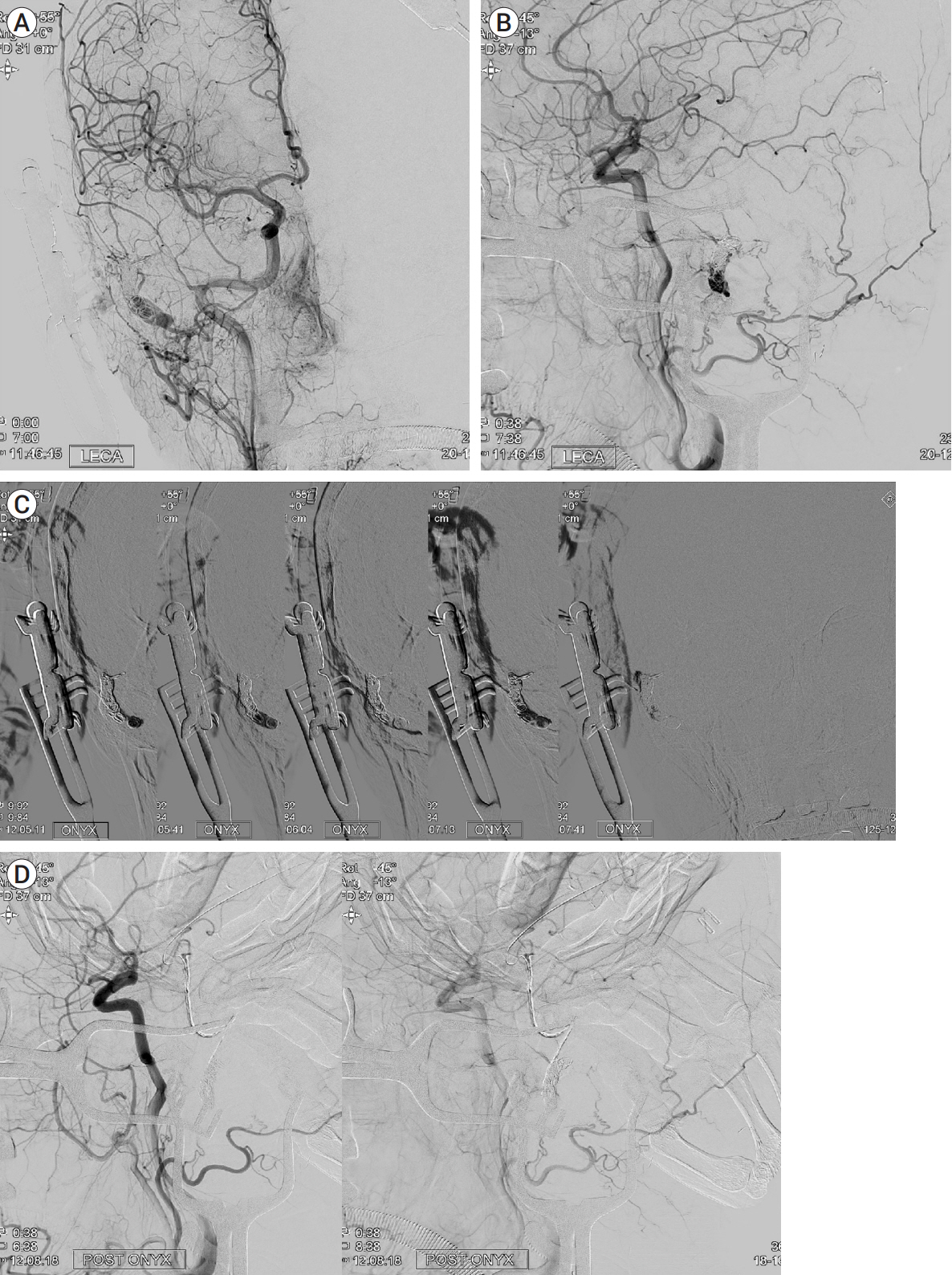
- Dural arteriovenous fistula (DAVF) is a rare condition affecting approximately 1.5% of 1,000,000 individuals annually. It frequently occurs in the transsigmoid and cavernous sinuses. An isolated sigmoid sinus is extremely rare and is treated by performing transfemoral transvenous embolization along the opposite transverse sinus. A 69-year-old woman presented with asymptomatic Borden type III/Cognard type III DAVF involving an isolated sigmoid sinus. She underwent a staged operation in which a navigation system was used to expose the sigmoid sinus in the operating room before transferring the patient to the angio suite for transvenous embolization. Various modalities have been used to treat DAVF, including surgical disconnection, transarterial embolization, transvenous embolization, and stereotactic radiosurgery. However, treating DAVF cases where the affected sinus is isolated can be challenging because an easily accessible surgical route may not be available. In this case, direct sinus cannulation and transvenous embolization were the most effective treatments.
Figure
Reference
-
1. Baharvahdat H, Ooi YC, Kim WJ, Mowla A, Coon AL, Colby GP. Updates in the management of cranial dural arteriovenous fistula. Stroke Vasc Neurol. 2019; Nov. 5(1):50–8.
Article2. Cheng AC, Li EY, Chan TC, Wong AC, Chan PC, Poon WW, et al. Hybrid procedure for orbital venous malformation in the endovascular operation room. Eye (Lond). 2015; Aug. 29(8):1069–75.
Article3. Choi JH, Jo KI, Kim KH, Jeon P, Yeon JY, Kim JS, et al. Early rebleeding of intracranial dural arteriovenous fistulas after an intracranial hemorrhage. Acta Neurochir (Wien). 2017; Aug. 159(8):1479–87.
Article4. Cognard C, Gobin YP, Pierot L, Bailly AL, Houdart E, Casasco A, et al. Cerebral dural arteriovenous fistulas: Clinical and angiographic correlation with a revised classification of venous drainage. Radiology. 1995; Mar. 194(3):671–80.
Article5. Cognard C, Januel AC, Silva NA Jr, Tall P. Endovascular treatment of intracranial dural arteriovenous fistulas with cortical venous drainage: New management using Onyx. AJNR Am J Neuroradiol. 2008; Feb. 29(2):235–41.
Article6. Duffau H, Lopes M, Janosevic V, Sichez JP, Faillot T, Capelle L, et al. Early rebleeding from intracranial dural arteriovenous fistulas: Report of 20 cases and review of the literature. J Neurosurg. 1999; Jan. 90(1):78–84.
Article7. Elhammady MS, Ambekar S, Heros RC. Epidemiology, clinical presentation, diagnostic evaluation, and prognosis of cerebral dural arteriovenous fistulas. Handb Clin Neurol. 2017; 143:99–105.
Article8. Endo S, Kuwayama N, Takaku A, Nishijima M. Direct packing of the isolated sinus in patients with dural arteriovenous fistulas of the transverse-sigmoid sinus. J Neurosurg. 1998; Mar. 88(3):449–56.
Article9. Gandhi D, Chen J, Pearl M, Huang J, Gemmete JJ, Kathuria S. Intracranial dural arteriovenous fistulas: Classification, imaging findings, and treatment. AJNR Am J Neuroradiol. 2012; Jun. 33(6):1007–13.
Article10. Gross BA, Du R. Surgical treatment of high grade dural arteriovenous fistulae. J Clin Neurosci. 2013; Nov. 20(11):1527–32.
Article11. Komiyama M, Ishiguro T, Matsusaka Y, Yasui T, Nishio A. Nishio A. Transfemoral, transvenous embolisation of dural arteriovenous fistula involving the isolated transverse-sigmoid sinus from the contralateral side. Acta Neurochir (Wien). 2002; Oct. 144(10):1041–6. discussion 1046.
Article12. Micieli JA, Derkatch S, Pereira VM, Margolin EA. Development of dural arteriovenous fistulas after cerebral venous sinus thrombosis. J Neuroophthalmol. 2016; Mar. 36(1):53–7.
Article13. Murayama Y, Arakawa H, Ishibashi T, Kawamura D, Ebara M, Irie K, et al. Combined surgical and endovascular treatment of complex cerebrovascular diseases in the hybrid operating room. J Neurointerv Surg. 2013; Sep. 5(5):489–93.
Article14. Neki H, Yonezawa A, Shibata A, Tsukagoshi E, Yamane F, Ishihara S, et al. A minimally invasive approach for the treatment of isolated type intracranial dural arteriovenous fistula in a neurosurgical hybrid operating room. Interdiscip Neurosurg. 2020; Sep. 21:100762.
Article15. Vougioukas VI, Coulin CJ, Shah M, Berlis A, Hubbe U, Van Velthoven V. Benefits and limitations of image guidance in the surgical treatment of intracranial dural arteriovenous fistulas. Acta Neurochir (Wien). 2006; Feb. 148(2):145–53. discussion 153.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Contralateral Transverse Sinus Occlusion After Treatment of Transverse-Sigmoid Sinus Dural Arteriovenous Fistula: A Case Report
- Infantile Dural Arteriovenous Fistula of the Transverse Sinus Presenting with Ocular Symptoms, Case Reports and Review of Literature
- Borden Type I Sigmoid Sinus Dural Arteriovenous Fistula Presenting as Subarachnoid Hemorrhage from a Feeding Artery Aneurysm of the Anterior Inferior Cerebellar Artery: A Case Report
- Dural Arteriovenous Fistula Involving an Isolated Sinus Treated Using Transarterial Onyx Embolization
- Endovascular management of cavernous sinus dural arteriovenous fistulas: Overall review and considerations