Clin Endosc.
2024 Mar;57(2):263-267. 10.5946/ce.2022.213.
Single-pigtail plastic stent made from endoscopic nasobiliary drainage tubes in endoscopic ultrasound-guided gallbladder drainage: a retrospective case series
- KMID: 2553764
- DOI: http://doi.org/10.5946/ce.2022.213
Abstract
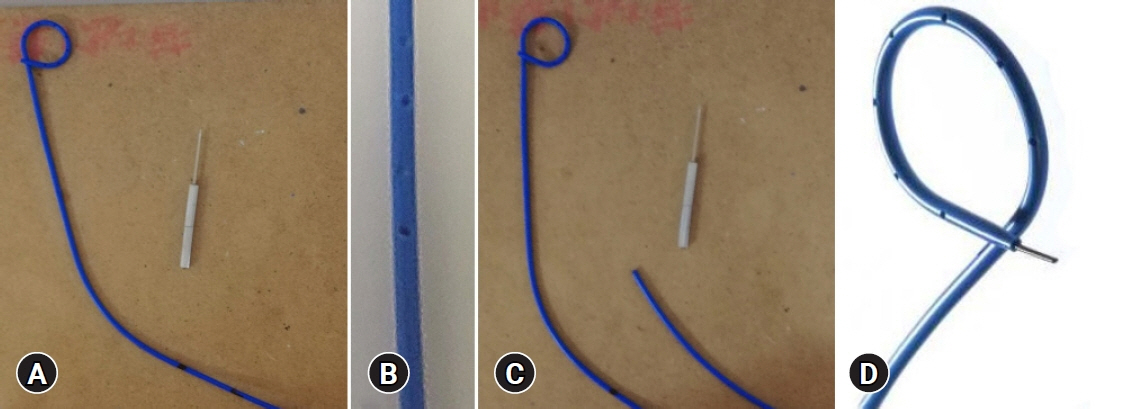
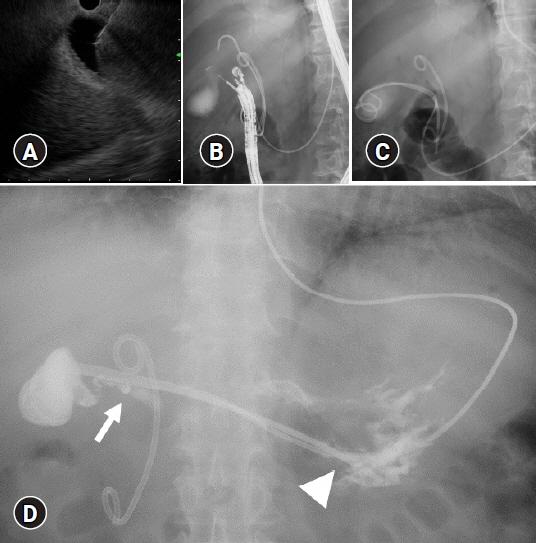
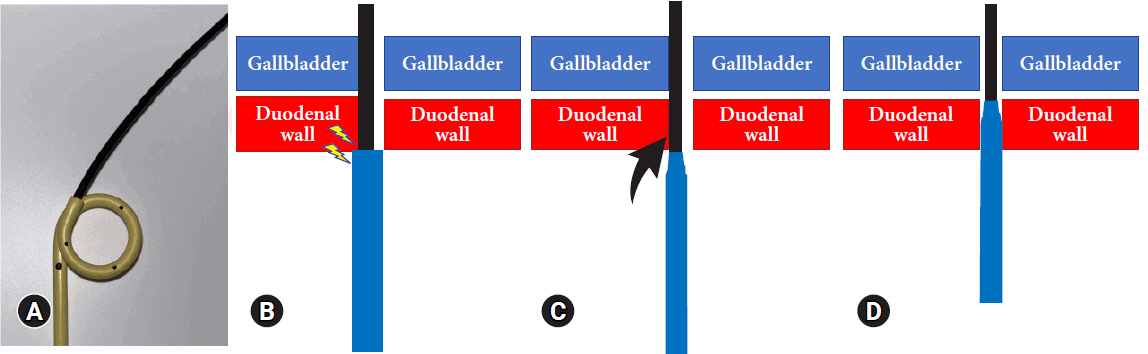
- Technical failure of endoscopic ultrasound-guided gallbladder drainage (EUS-GBD) is often attributed to device failure. To rectify this problem, we developed a single-pigtail plastic stent (SPPS) for EUS-GBD. We retrospectively reviewed the cases of four patients who underwent EUS-GBD for acute cholecystitis. To prepare the SPPS, a 7.5-Fr endoscopic nasobiliary drainage tube was cut to an appropriate length. The use of SPPS during EUS-GBD was successful from both technical and clinical standpoints. The SPPS spontaneously detached 57 days after the procedure in patient 4 and 412 days after the procedure in patient 1. Patient 1 developed cholecystitis after 426 days and was managed with antibiotics. The other three patients did not develop any complications after surgery. In conclusion, we designed a new SPPS dedicated to EUS-GBD and established its technical feasibility and clinical effectiveness.
Figure
Reference
-
1. van der Merwe SW, van Wanrooij RL, et al. Therapeutic endoscopic ultrasound: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2022; 54:185–205.2. Nishiguchi K, Ogura T, Okuda A, et al. Endoscopic gallbladder drainage for acute cholecystitis with high-risk surgical patients between transduodenal and transpapillary stenting. Endosc Ultrasound. 2021; 10:448–454.3. Park SW, Lee SS. Current status of endoscopic management of cholecystitis. Dig Endosc. 2022; 34:439–450.4. Yang MJ, Hwang JC, Yoo BM, et al. Tips for dealing with common beginner's mistakes made during endoscopic ultrasound-guided gallbladder drainage. Dig Dis. 2020; 38:542–546.5. ASA Physical Status Classification System [Internet]. American Society of Anesthesiologists;2020. [cited 2022 Aug 14]. Available from: https://www.asahq.org/standards-and-guidelines/asa-physical-status-classification-system.6. Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987; 40:373–383.7. Kanda M, Mizuno A, Tanaka C, et al. Nutritional predictors for postoperative short-term and long-term outcomes of patients with gastric cancer. Medicine (Baltimore). 2016; 95:e3781.8. Rana SS. Endoscopic ultrasound-guided gallbladder drainage: a technical review. Ann Gastroenterol. 2021; 34:142–148.9. James TW, Baron TH. EUS-guided gallbladder drainage: a review of current practices and procedures. Endosc Ultrasound. 2019; 8(Suppl 1):S28–S34.10. Flexima Plus [Internet]. Boston Scientific Corporation;2022. [cited 2022 Aug 14]. Available from: https://www.bostonscientific.com/jp-JP/products/stent/FleximaPlus.html. Japanese.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Stent occlusion in endoscopic ultrasound-guided gallbladder drainage from bleeding mitigated by double pigtail plastic stent deployment within lumen apposing metal stent
- Endoscopic Transpapillary Gallbladder Stenting for Acute Cholecystitis in a Patient with Metastatic Pancreatic Cancer
- Practical Approaches for High-Risk Surgical Patients with Acute Cholecystitis: The Percutaneous Approach versus Endoscopic Alternatives
- Endoscopic Ultrasound-Guided Perirectal Abscess Drainage without Drainage Catheter: A Case Series
- Endoscopic Ultrasound-Guided Hepaticogastrostomy: Technical Review and Tips to Prevent Adverse Events