Diabetes Metab J.
2024 Mar;48(2):290-301. 10.4093/dmj.2022.0299.
Risk of Depression according to Cumulative Exposure to a Low-Household Income Status in Individuals with Type 2 Diabetes Mellitus: A Nationwide Population- Based Study
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Department of Biomedicine & Health Sciences, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 3Department of Statistics and Actuarial Science, Soongsil University, Seoul, Korea
- 4Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 5Division of Endocrinology and Metabolism, Department of Internal Medicine, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea
- 6Department of Clinical Research Design and Evaluation, Samsung Advanced Institute for Health Sciences & Technology, Sungkyunkwan University, Seoul, Korea
- KMID: 2553599
- DOI: http://doi.org/10.4093/dmj.2022.0299
Abstract
- Background
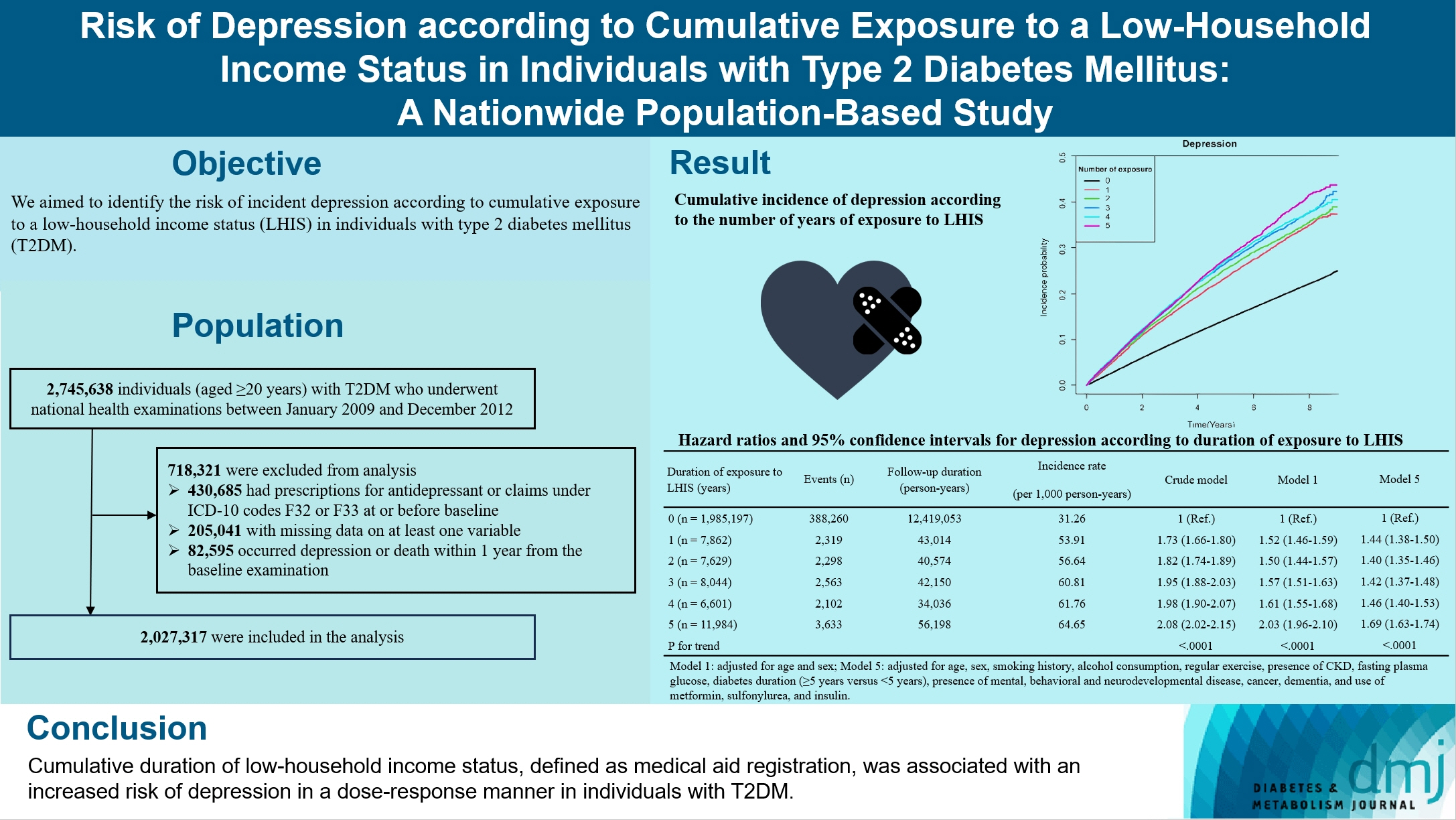
We aimed to identify the risk of incident depression according to cumulative exposure to a low-household income status in individuals with type 2 diabetes mellitus (T2DM).
Methods
For this retrospective longitudinal population-based cohort study, we used Korean National Health Insurance Service data from 2002 to 2018. Risk of depression was assessed according to cumulative exposure to low-household income status (defined as Medical Aid registration) during the previous 5 years among adults (aged ≥20 years) with T2DM and without baseline depression who underwent health examinations from 2009 to 2012 (n=2,027,317).
Results
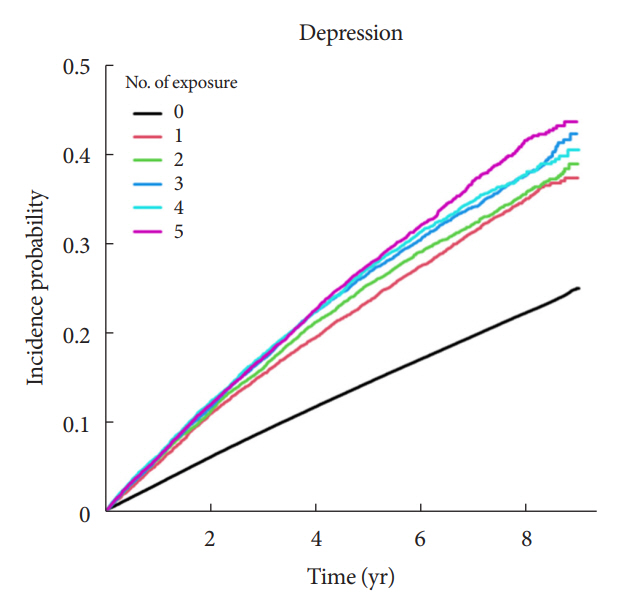
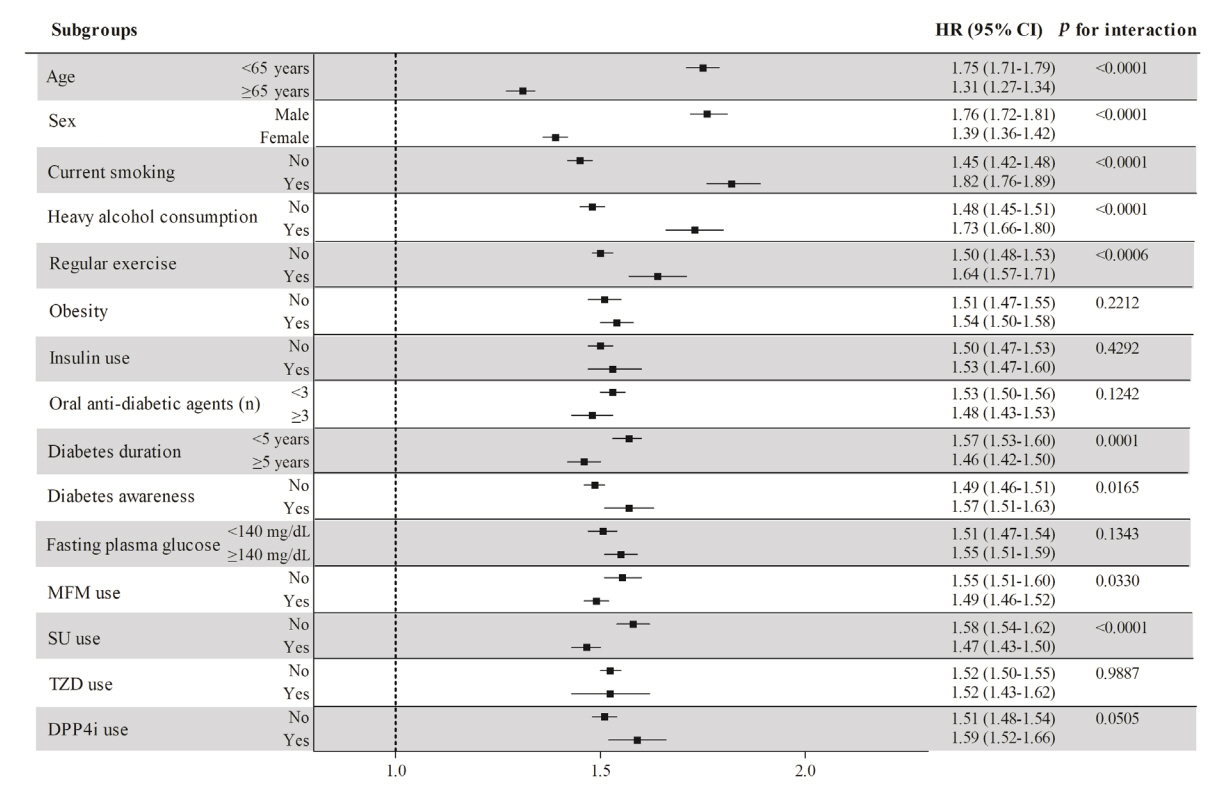
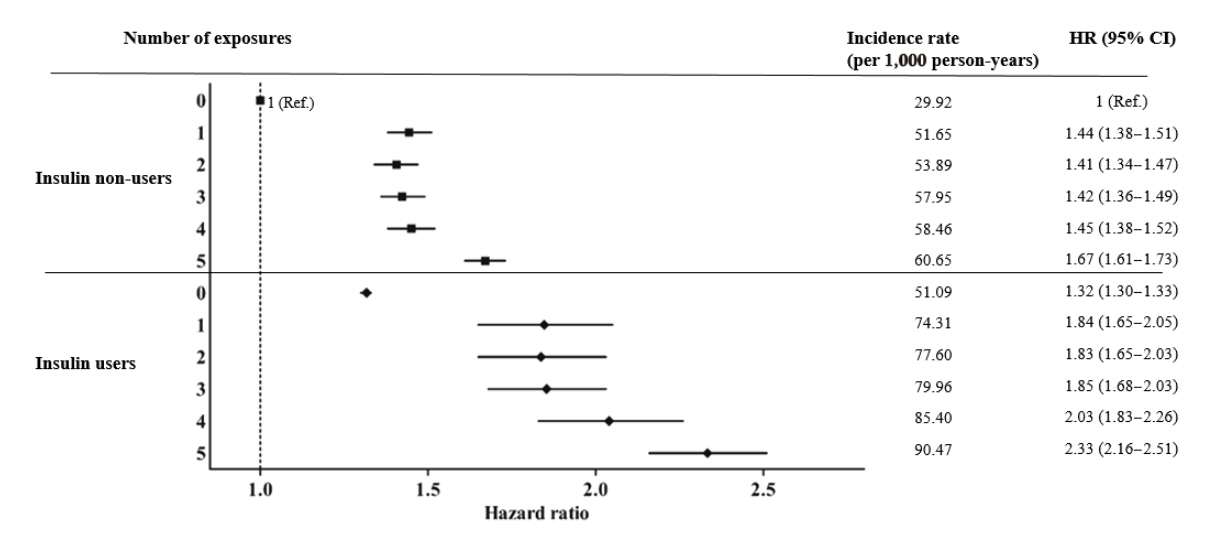
During an average 6.23 years of follow-up, 401,175 incident depression cases occurred. Advance in cumulative number of years registered for medical aid during the previous 5 years from baseline was associated with an increased risk of depression in a dose-dependent manner (hazard ratio [HR], 1.44 [95% confidence interval (CI), 1.38 to 1.50]; HR, 1.40 [95% CI, 1.35 to 1.46]; HR, 1.42, [95% CI, 1.37 to 1.48]; HR, 1.46, [95% CI, 1.40 to 1.53]; HR, 1.69, [95% CI, 1.63 to 1.74] in groups with 1 to 5 exposed years, respectively). Insulin users exposed for 5 years to a low-household income state had the highest risk of depression among groups categorized by insulin use and duration of low-household income status.
Conclusion
Cumulative duration of low-household income status, defined as medical aid registration, was associated with an increased risk of depression in a dose-response manner in individuals with T2DM.
Keyword
Figure
Reference
-
1. Spijker J, Graaf R, Bijl RV, Beekman AT, Ormel J, Nolen WA. Functional disability and depression in the general population: results from the Netherlands Mental Health Survey and Incidence Study (NEMESIS). Acta Psychiatr Scand. 2004; 110:208–14.
Article2. Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: a metaanalysis. Diabetes Care. 2001; 24:1069–78.3. Roy T, Lloyd CE. Epidemiology of depression and diabetes: a systematic review. J Affect Disord. 2012; 142 Suppl:S8–21.
Article4. Robinson ME, Simard M, Larocque I, Shah J, Nakhla M, Rahme E. Risk of psychiatric disorders and suicide attempts in emerging adults with diabetes. Diabetes Care. 2020; 43:484–6.
Article5. Ascher-Svanum H, Zagar A, Jiang D, Schuster D, Schmitt H, Dennehy EB, et al. Associations between glycemic control, depressed mood, clinical depression, and diabetes distress before and after insulin initiation: an exploratory, post hoc analysis. Diabetes Ther. 2015; 6:303–16.
Article6. Park CY, Kim SY, Gil JW, Park MH, Park JH, Kim Y. Depression among Korean adults with type 2 diabetes mellitus: Ansan-Community-Based Epidemiological Study. Osong Public Health Res Perspect. 2015; 6:224–32.
Article7. Lorant V, Deliege D, Eaton W, Robert A, Philippot P, Ansseau M. Socioeconomic inequalities in depression: a meta-analysis. Am J Epidemiol. 2003; 157:98–112.
Article8. Leone T, Coast E, Narayanan S, de Graft Aikins A. Diabetes and depression comorbidity and socio-economic status in low and middle income countries (LMICs): a mapping of the evidence. Global Health. 2012; 8:39.
Article9. Ell K, Katon W, Cabassa LJ, Xie B, Lee PJ, Kapetanovic S, et al. Depression and diabetes among low-income Hispanics: design elements of a socioculturally adapted collaborative care model randomized controlled trial. Int J Psychiatry Med. 2009; 39:113–32.
Article10. Tellez-Zenteno JF, Cardiel MH. Risk factors associated with depression in patients with type 2 diabetes mellitus. Arch Med Res. 2002; 33:53–60.
Article11. Egede LE, Zheng D. Independent factors associated with major depressive disorder in a national sample of individuals with diabetes. Diabetes Care. 2003; 26:104–11.
Article12. Butwicka A, Frisen L, Almqvist C, Zethelius B, Lichtenstein P. Risks of psychiatric disorders and suicide attempts in children and adolescents with type 1 diabetes: a population-based cohort study. Diabetes Care. 2015; 38:453–9.
Article13. Bai X, Liu Z, Li Z, Yan D. The association between insulin therapy and depression in patients with type 2 diabetes mellitus: a meta-analysis. BMJ Open. 2018; 8:e020062.
Article14. Lee YH, Han K, Ko SH, Ko KS, Lee KU; Taskforce Team of Diabetes Fact Sheet of the Korean Diabetes Association. Data analytic process of a nationwide population-based study using National Health Information Database established by National Health Insurance Service. Diabetes Metab J. 2016; 40:79–82.
Article15. Lee YB, Han K, Kim B, Lee SE, Jun JE, Ahn J, et al. Risk of early mortality and cardiovascular disease in type 1 diabetes: a comparison with type 2 diabetes, a nationwide study. Cardiovasc Diabetol. 2019; 18:157.
Article16. Lee YB, Han K, Kim B, Jin SM, Lee SE, Jun JE, et al. High proportion of adult cases and prevalence of metabolic syndrome in type 1 diabetes mellitus population in Korea: a nationwide study. Diabetes Metab J. 2019; 43:76–89.
Article17. Noh J, Han KD, Ko SH, Ko KS, Park CY. Trends in the pervasiveness of type 2 diabetes, impaired fasting glucose and comorbidities during an 8-year-follow-up of nationwide Korean population. Sci Rep. 2017; 7:46656.
Article18. Jin EH, Han K, Lee DH, Shin CM, Lim JH, Yoon H, et al. Increased risk of major depressive disorder after cholecystectomy: a nationwide population-based cohort study in Korea. Clin Transl Gastroenterol. 2021; 12:e00339.
Article19. Stampfer MJ, Kang JH, Chen J, Cherry R, Grodstein F. Effects of moderate alcohol consumption on cognitive function in women. N Engl J Med. 2005; 352:245–53.
Article20. Lee YB, Kim DH, Kim SM, Kim NH, Choi KM, Baik SH, et al. Hospitalization for heart failure incidence according to the transition in metabolic health and obesity status: a nationwide population-based study. Cardiovasc Diabetol. 2020; 19:77.
Article21. Kim MK, Han K, Kim HS, Park YM, Kwon HS, Yoon KH, et al. Cholesterol variability and the risk of mortality, myocardial infarction, and stroke: a nationwide population-based study. Eur Heart J. 2017; 38:3560–6.
Article22. Lee YB, Han K, Kim B, Jun JE, Lee SE, Ahn J, et al. Risk of endstage renal disease from chronic kidney disease defined by decreased glomerular filtration rate in type 1 diabetes: a comparison with type 2 diabetes and the effect of metabolic syndrome. Diabetes Metab Res Rev. 2019; 35:e3197.
Article23. Lee YB, Han K, Kim B, Choi MS, Park J, Kim M, et al. Risk of early mortality and cardiovascular disease according to the presence of recently diagnosed diabetes and requirement for insulin treatment: a nationwide study. J Diabetes Investig. 2021; 12:1855–63.
Article24. Nam GE, Park YG, Han K, Kim MK, Koh ES, Kim ES, et al. BMI, weight change, and dementia risk in patients with newonset type 2 diabetes: a nationwide cohort study. Diabetes Care. 2019; 42:1217–24.
Article25. Kim MK, Han K, Lee SH. Current trends of big data research using the Korean National Health Information Database. Diabetes Metab J. 2022; 46:552–63.
Article26. Katon W, von Korff M, Ciechanowski P, Russo J, Lin E, Simon G, et al. Behavioral and clinical factors associated with depression among individuals with diabetes. Diabetes Care. 2004; 27:914–20.
Article27. Ali S, Stone MA, Peters JL, Davies MJ, Khunti K. The prevalence of co-morbid depression in adults with type 2 diabetes: a systematic review and meta-analysis. Diabet Med. 2006; 23:1165–73.28. Kim MK, Lee WY, Kang JH, Kang JH, Kim BT, Kim SM, et al. 2014 Clinical practice guidelines for overweight and obesity in Korea. Endocrinol Metab (Seoul). 2014; 29:405–9.
Article29. Mendenhall E, Shivashankar R, Tandon N, Ali MK, Narayan KM, Prabhakaran D. Stress and diabetes in socioeconomic context: a qualitative study of urban Indians. Soc Sci Med. 2012; 75:2522–9.
Article30. Neupert SD, Almeida DM, Charles ST. Age differences in reactivity to daily stressors: the role of personal control. J Gerontol B Psychol Sci Soc Sci. 2007; 62:P216–25.
Article31. Fiske A, Wetherell JL, Gatz M. Depression in older adults. Annu Rev Clin Psychol. 2009; 5:363–89.
Article32. Andres AR, Collings S, Qin P. Sex-specific impact of socioeconomic factors on suicide risk: a population-based case-control study in Denmark. Eur J Public Health. 2010; 20:265–70.
Article33. Ogunwole SM, Golden SH. Social determinants of health and structural inequities: root causes of diabetes disparities. Diabetes Care. 2021; 44:11–3.34. Wium-Andersen IK, Osler M, Jorgensen MB, Rungby J, Wium-Andersen MK. Diabetes, antidiabetic medications and risk of depression: a population-based cohort and nested case-control study. Psychoneuroendocrinology. 2022; 140:105715.35. Khaledi M, Haghighatdoost F, Feizi A, Aminorroaya A. The prevalence of comorbid depression in patients with type 2 diabetes: an updated systematic review and meta-analysis on huge number of observational studies. Acta Diabetol. 2019; 56:631–50.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Do Type 1 and Type 2 Diabetes Have the Same Vascular Complications?
- Low Household Income Status and Death from Pneumonia in People with Type 2 Diabetes Mellitus: A Nationwide Study
- Association between asthma and depression in Korean adults
- Factors Associated with Depression among Working-Age Household Heads in Korea: A Cross-Sectional Household Study
- Depressive Symptoms Are Negatively Associated with Glucose Testing and Eating Meals on Time among Individuals with Diabetes in Zambia