Korean J Sports Med.
2024 Mar;42(1):55-58. 10.5763/kjsm.2024.42.1.55.
Regeneration of Acromion Osteolysis after Hook Plate Fixation for Distal Clavicle Fracture: A Case Report
- Affiliations
-
- 1Department of Orthopaedic Surgery, Dankook University College of Medicine, Cheonan, Korea
- KMID: 2553557
- DOI: http://doi.org/10.5763/kjsm.2024.42.1.55
Abstract
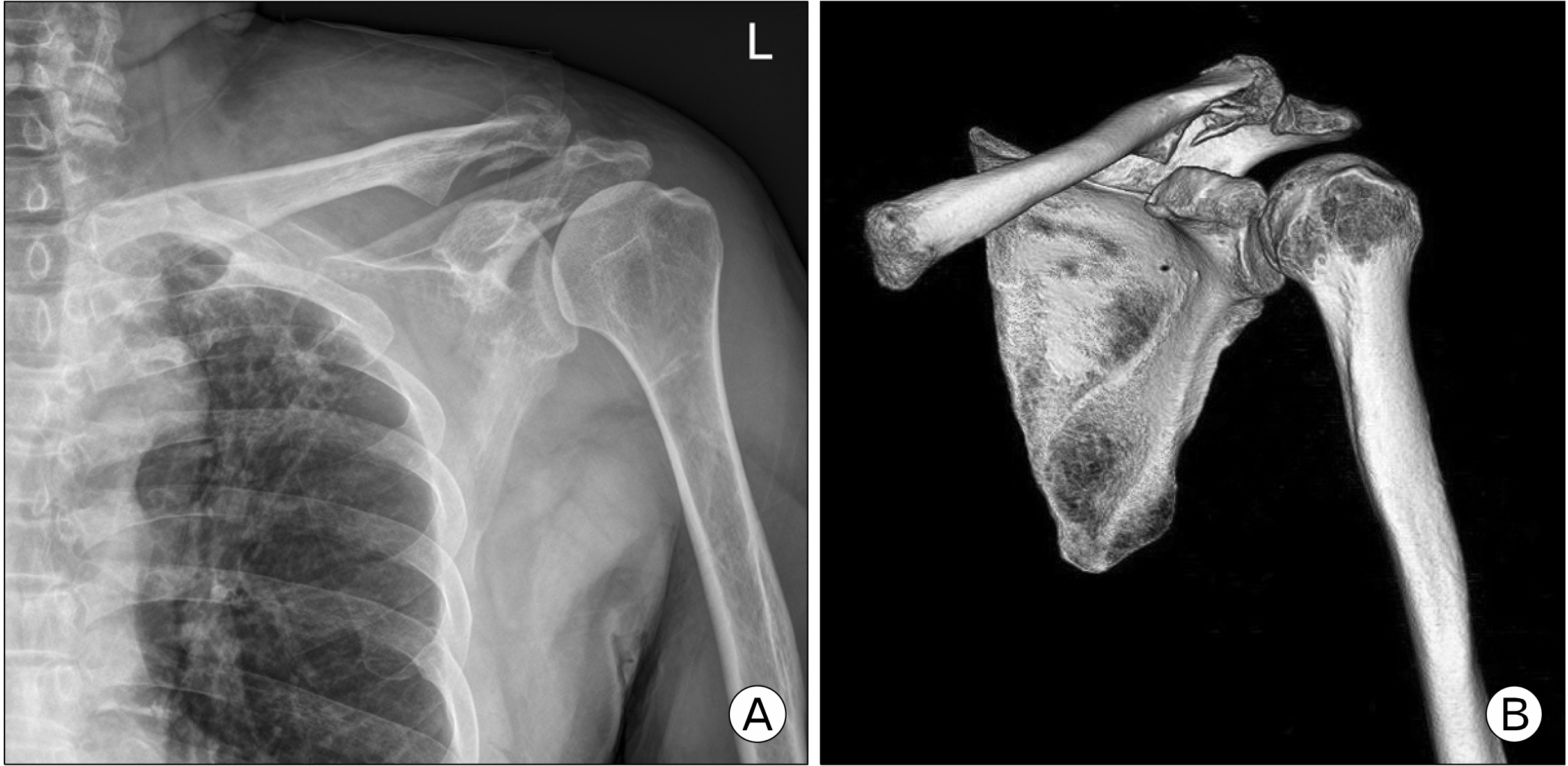
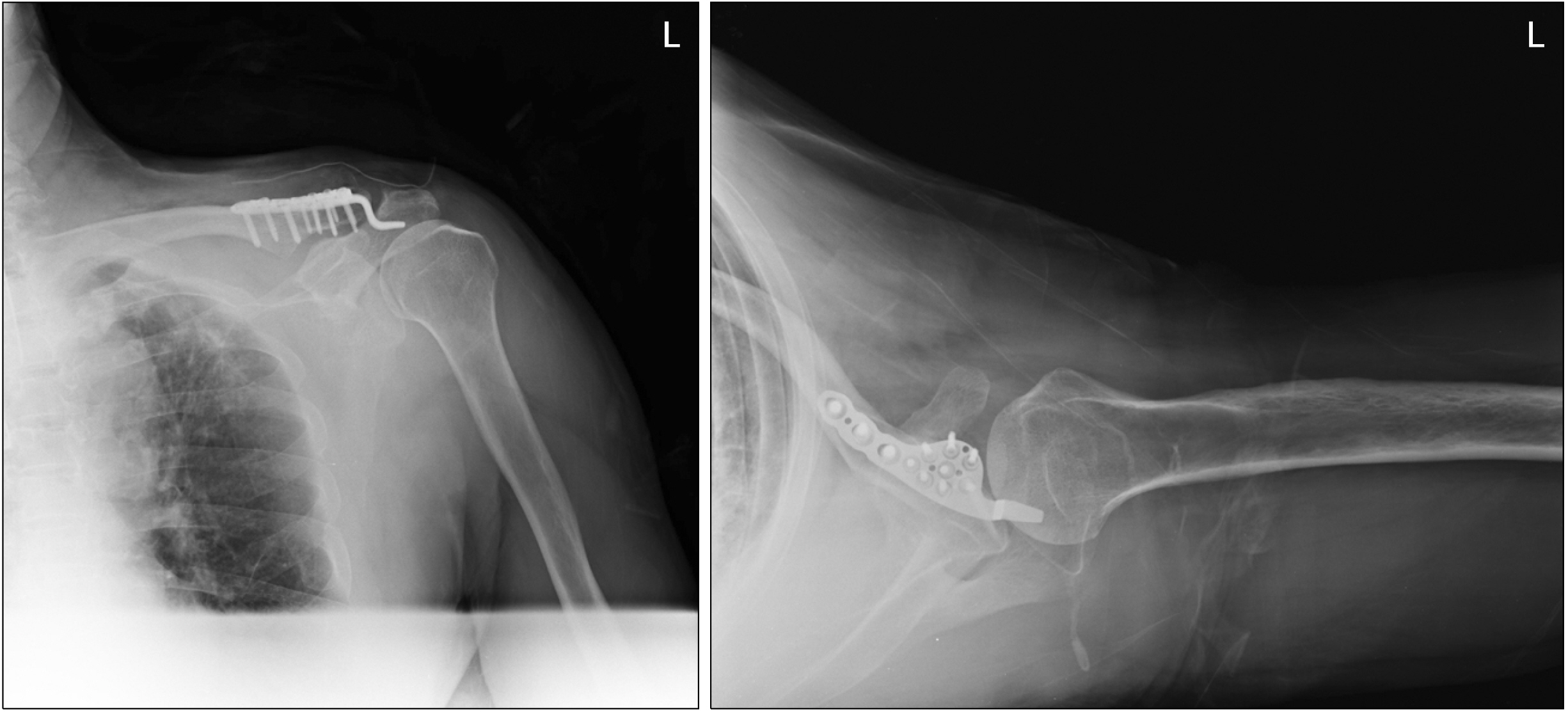
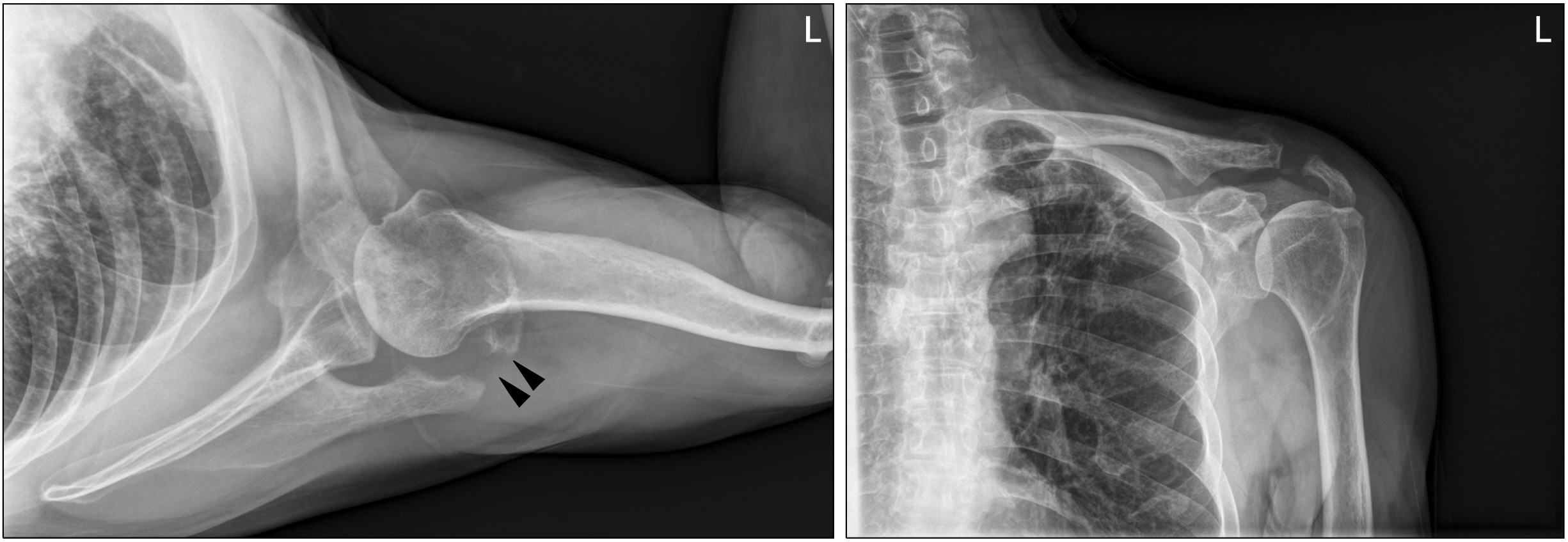
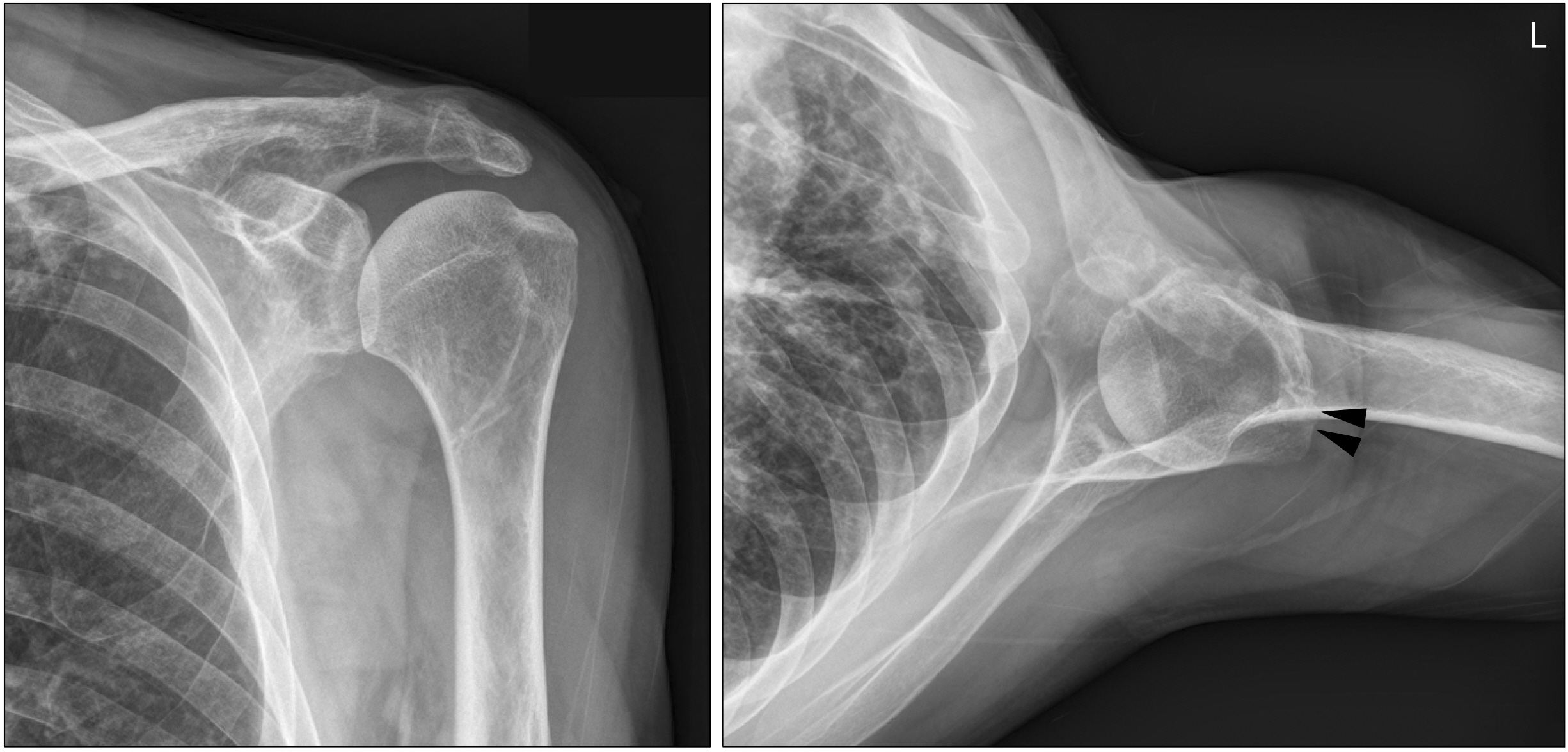
- We presented the case of a 60-year-old man with an unexpected complication of acromial osteolysis with subsequent regeneration of the acromion. To our knowledge, this case report represents the first description of the regeneration of acromion after osteolysis. He underwent open reduction and internal fixation with a novel hybrid hook locking compression plate 6 days after the injury. No procedure was undertaken for the coracoclavicular ligament in this case. Five months after internal fixation with a hook plate, the patient underwent surgery for the removal of the hook plate. Radiographs after removal of the hook plate showed erosion of the acromion. We decided to perform a conservative treatment for acromion osteolysis and observed the progress. A final radiograph that was obtained 10 months after hook plate removal shows regeneration of the acromion. We thought that the periosteum played a significant role in the acromion regeneration despite no special treatment.
Keyword
Figure
Reference
-
1. Court-Brown CM, Heckman JD, McQueen MM, Ricci WM, Tornetta P, McKee MD. Rockwood and Green's fractures in adults. Wolters Kluwer Health;2015.2. Chiang CL, Yang SW, Tsai MY, Kuen-Huang Chen C. 2010; Acromion osteolysis and fracture after hook plate fixation for acromioclavicular joint dislocation: a case report. J Shoulder Elbow Surg. 19:e13–5. DOI: 10.1016/j.jse.2009.12.005. PMID: 20303294.
Article3. Hoffler CE, Karas SG. 2010; Transacromial erosion of a locked subacromial hook plate: case report and review of literature. J Shoulder Elbow Surg. 19:e12–5. DOI: 10.1016/j.jse.2009.10.019. PMID: 20189416.4. Nadarajah R, Mahaluxmivala J, Amin A, Goodier DW. 2005; Clavicular hook-plate: complications of retaining the implant. Injury. 36:681–3. DOI: 10.1016/j.injury.2004.08.010. PMID: 15826633.5. Seo J, Heo K, Kim SJ, Kim JK, Ham HJ, Yoo J. 2020; Comparison of a novel hybrid hook locking plate fixation method with the conventional AO hook plate fixation method for Neer type V distal clavicle fractures. Orthop Traumatol Surg Res. 106:67–75. DOI: 10.1016/j.otsr.2019.10.014. PMID: 31826826.6. Li L, Li TY, Jiang P, et al. 2019; Clavicle hook plate versus distal clavicle locking plate for Neer type II distal clavicle fractures. J Orthop Surg Res. 14:472. DOI: 10.1186/s13018-019-1518-x. PMID: 31888668. PMCID: PMC6936130.7. Sarda P. 2019; Lateral clavicle fractures with coracoclavicular ligament disruption (Neer's type IIB): review of literature and a new technique for all-suture fixation. Indian J Orthop. 53:465–71. DOI: 10.4103/ortho.IJOrtho_485_18. PMID: 31080289. PMCID: PMC6501619.
Article8. Fox HM, Ramsey DC, Thompson AR, Hoekstra CJ, Mirarchi AJ, Nazir OF. 2020; Neer type-II distal clavicle fractures: a cost-effectiveness analysis of fixation techniques. J Bone Joint Surg Am. 102:254–61. DOI: 10.2106/JBJS.19.00590. PMID: 31809393.9. Singh A, Schultzel M, Fleming JF, Navarro RA. 2019; Complications after surgical treatment of distal clavicle fractures. Orthop Traumatol Surg Res. 105:853–9. DOI: 10.1016/j.otsr.2019.03.012. PMID: 31202717.10. Matsumura N, Takada Y, Seto T, Suzuki T, Iwamoto T, Sato K. 2019; Cerclage wiring fixation for the treatment of long oblique fractures of the distal clavicle: a report of 2 cases. JBJS Case Connect. 9:e0085. DOI: 10.2106/JBJS.CC.19.00085. PMID: 31850913.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Acromion Fracture after Hook Plate Fixation for Distal Clavicle Injury: A Report of 2 Cases
- Complications of Hook-Plate Fixation for Distal Clavicle Fractures
- Internal Fixation Using Clavicle Hook Plates for Distal Clavicle Fractures
- Periprosthetic Clavicle Shaft Fracture After Treatment of Type V Distal Clavicle Fracture Using a Hook Plate: A Report of Two Cases
- The Radiologic Comparison of Operative Treatment Using a Hook Plate versus a Distal Clavicle Locking Plate of Distal Clavicle Fracture