Ann Hepatobiliary Pancreat Surg.
2024 Feb;28(1):59-69. 10.14701/ahbps.23-068.
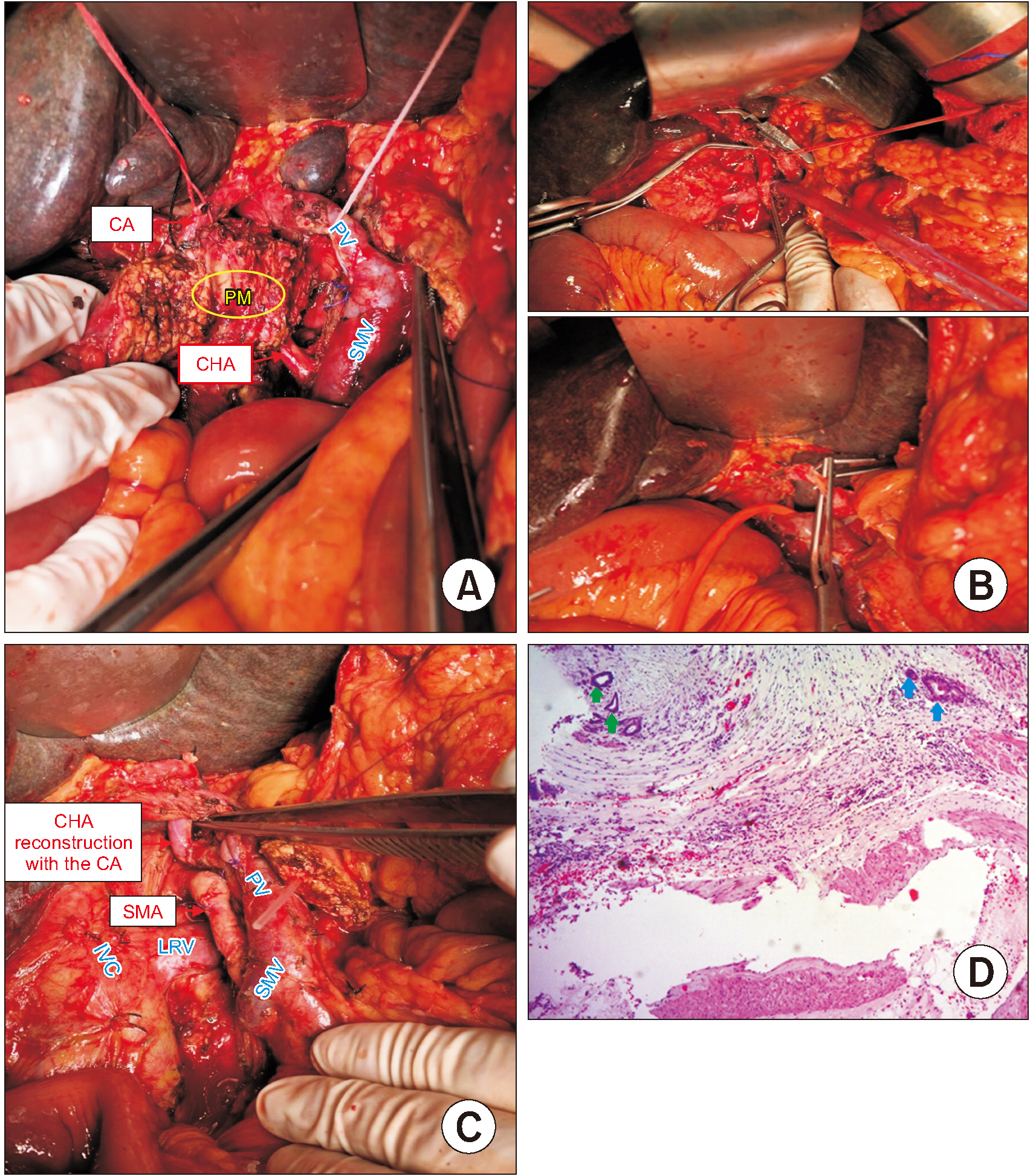
Pancreaticoduodenectomy with superior mesenteric artery first-approach combined total meso-pancreas excision for periampullary malignancies: A high-volume single-center experience with short-term outcomes
- Affiliations
-
- 1Department of Gastrointestinal and Hepato-Pancreato-Biliary Surgery, Bach Mai Hospital, Hanoi, Vietnam
- 2VinUniversity, Hanoi, Vietnam
- 3Department of Surgery, Thai Binh Medical University, Thai Binh, Vietnam
- 4Pathology Center, Bach Mai Hospital, Hanoi, Vietnam
- 5108 Institute of Clinical Medical and Pharmaceutical Sciences, Hanoi, Vietnam
- 6Department of Oncology, Viet Duc University Hospital, Hanoi, Vietnam
- 7Department of Hepato-Biliary-Pancreatic Surgery, Cancer Institute Hospital, Japanese Foundation for Cancer Research, Tokyo, Japan
- KMID: 2553367
- DOI: http://doi.org/10.14701/ahbps.23-068
Abstract
- Backgrounds/Aims
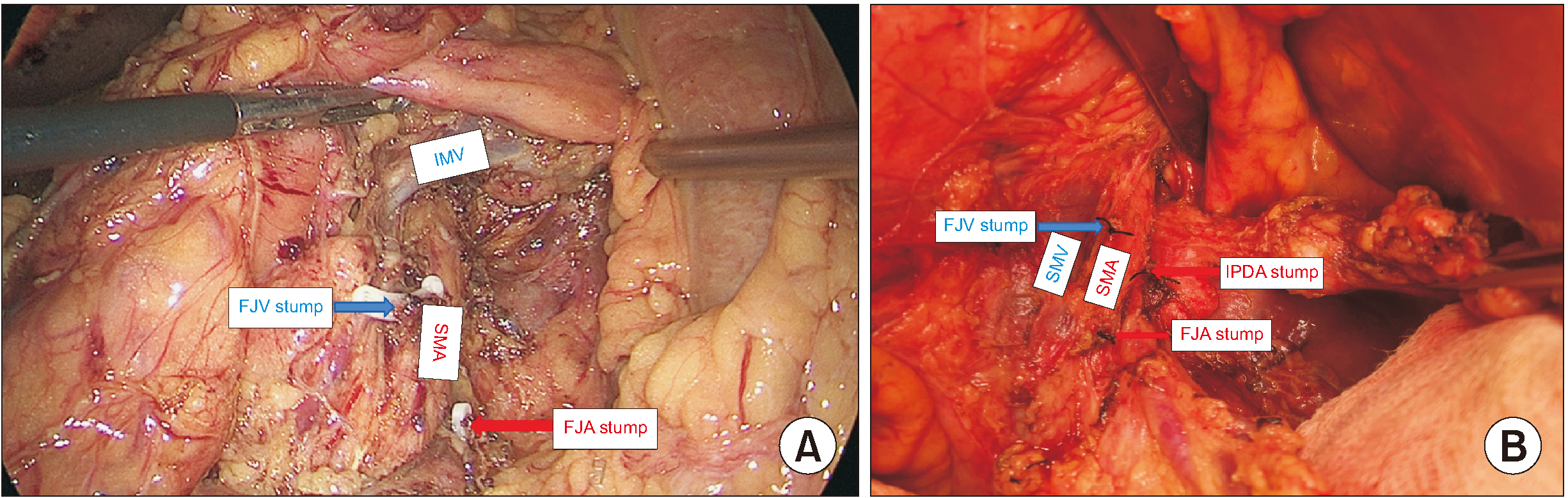
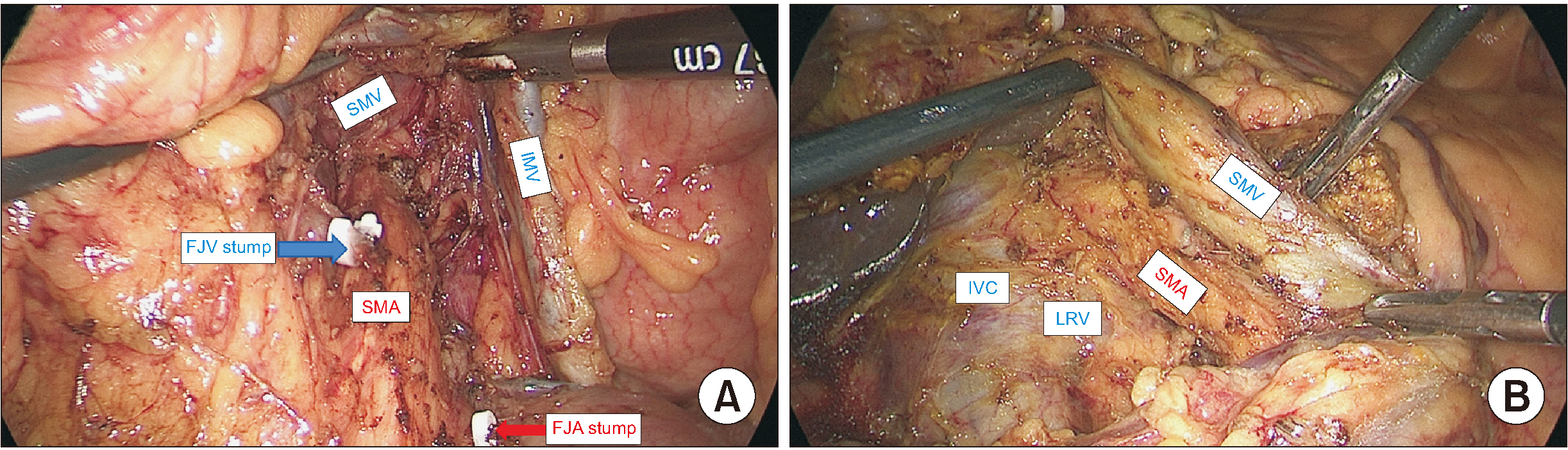
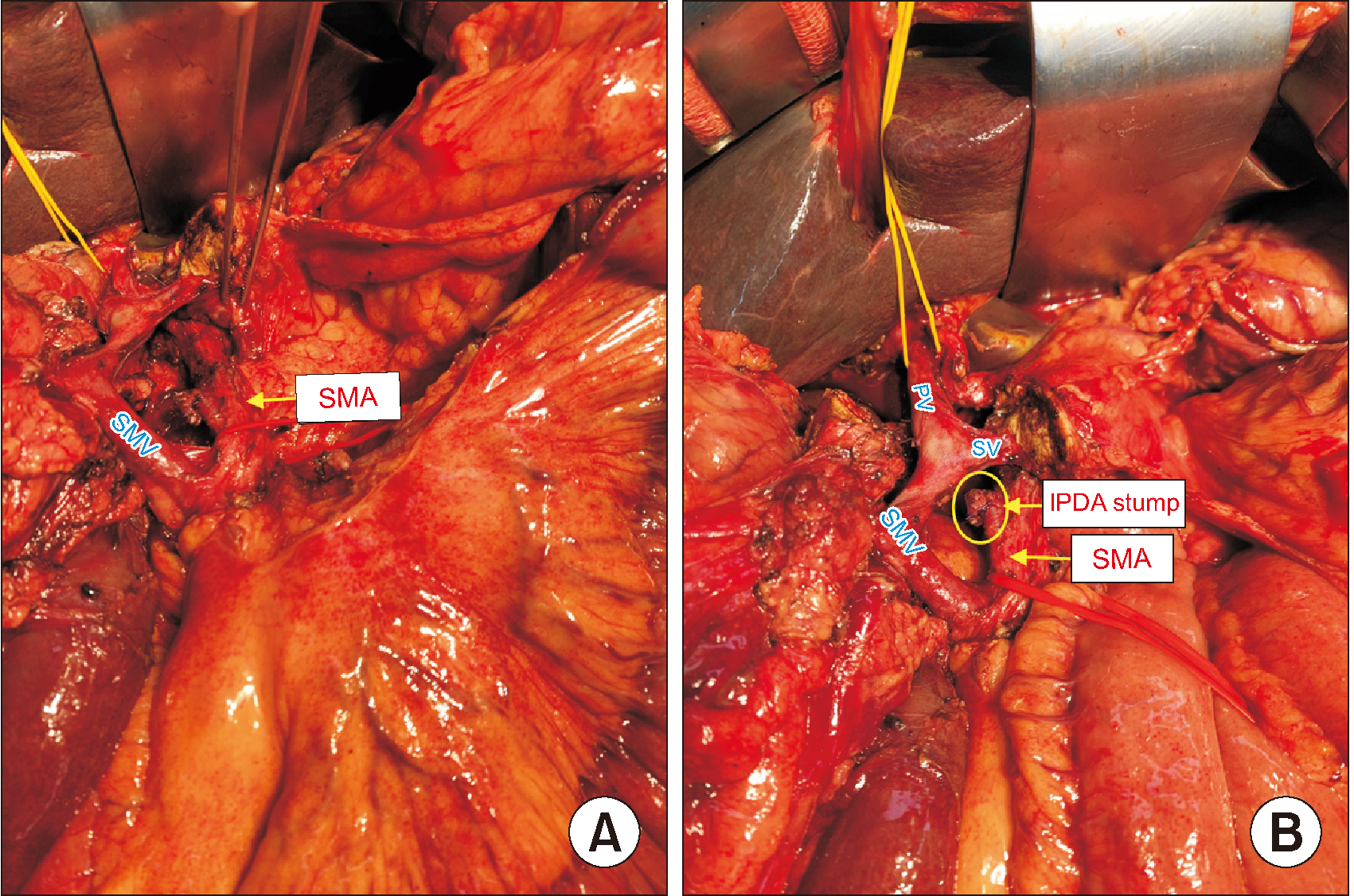
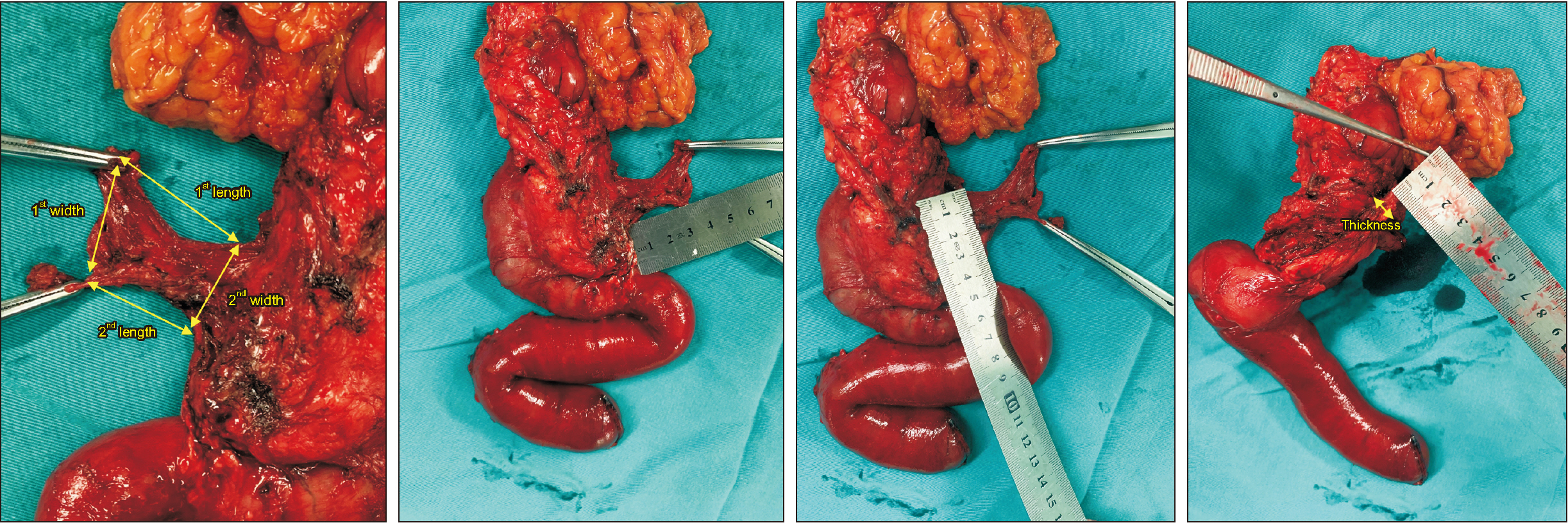
Pancreaticoduodenectomy (PD) is the only radical treatment for periampullary malignancies. Superior mesenteric artery (SMA) first approach combined with total meso-pancreas (MP) excision was conducted to improve the oncological results. There has not been any previous research of a technique that combines the SMA first approach and total MP excision with a detailed description of the MP macroscopical shape.
Methods
We prospectively assessed 77 patients with periampullary malignancies between October 2020 and March 2022 (18 months). All patients had undergone PD with SMA first approach combined total MP excision. The perioperative indications, clinical data, intra-operative index, R0 resection rate of postoperative pathological specimens (especially mesopancreatic margin), postoperative complications, and follow-up results were evaluated.
Results
The median operative time was 289.6 min (178−540 min), the median intraoperative blood loss was 209 mL (30−1,600 mL). Microscopically, there were 19 (24.7%) cases with metastatic MP, and five cases (6.5%) with R1-resection of the MP. The number of lymph nodes (LNs) harvested and metastatic LNs were 27.2 (maximum was 74) and 1.8 (maximum was 16), respectively. Some (46.8%) patients had pancreatic fistula, but mostly in grade A, with 7 patients (9.1%) who required re-operations. Some 18.2% of cases developed postoperative refractory diarrhea. The rate of in-hospital mortality was 1.3%.
Conclusions
The PD with SMA first approach combined TMpE for periampullary malignancies was effective in achieving superior oncological statistics (rate of MP R0-resection and number of total resected LNs) with non-inferior short-term outcomes. It is necessary to evaluate survival outcomes with long-term follow-up.
Keyword
Figure
Reference
-
1. Fernandez-Cruz L. Holzheimer RG, Mannick JA, editors. 2001. Periampullary carcinoma. Surgical Treatment: Evidence-Based and Problem-Oriented. Zuckschwerdt;p. 1–9.2. Rahib L, Smith BD, Aizenberg R, Rosenzweig AB, Fleshman JM, Matrisian LM. 2014; Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res. 74:2913–2921. DOI: 10.1158/0008-5472.CAN-14-0155. PMID: 24840647.
Article3. Hackert T, Sachsenmaier M, Hinz U, Schneider L, Michalski CW, Springfeld C, et al. 2016; Locally advanced pancreatic cancer: neoadjuvant therapy with folfirinox results in resectability in 60% of the patients. Ann Surg. 264:457–463. DOI: 10.1097/SLA.0000000000001850. PMID: 27355262.4. Ironside N, Barreto SG, Loveday B, Shrikhande SV, Windsor JA, Pandanaboyana S. 2018; Meta-analysis of an artery-first approach versus standard pancreatoduodenectomy on perioperative outcomes and survival. Br J Surg. 105:628–636. DOI: 10.1002/bjs.10832. PMID: 29652079.
Article5. Jiang X, Yu Z, Ma Z, Deng H, Ren W, Shi W, et al. 2020; Superior mesenteric artery first approach can improve the clinical outcomes of pancreaticoduodenectomy: a meta-analysis. Int J Surg. 73:14–24. DOI: 10.1016/j.ijsu.2019.11.007. PMID: 31751791.
Article6. Menon KV, Gomez D, Smith AM, Anthoney A, Verbeke CS. 2009; Impact of margin status on survival following pancreatoduodenectomy for cancer: the Leeds Pathology Protocol (LEEPP). HPB (Oxford). 11:18–24. DOI: 10.1111/j.1477-2574.2008.00013.x. PMID: 19590619. PMCID: PMC2697870.
Article7. Gockel I, Domeyer M, Wolloscheck T, Konerding MA, Junginger T. 2007; Resection of the mesopancreas (RMP): a new surgical classification of a known anatomical space. World J Surg Oncol. 5:44. DOI: 10.1186/1477-7819-5-44. PMID: 17459163. PMCID: PMC1865381.
Article8. Kawabata Y, Hayashi H, Ishikawa N, Tajima Y. 2016; Total meso-pancreatoduodenum excision with pancreaticoduodenectomy in lower biliary tract cancer. Langenbecks Arch Surg. 401:463–469. DOI: 10.1007/s00423-016-1435-y. PMID: 27102325.
Article9. Adham M, Singhirunnusorn J. 2012; Surgical technique and results of total mesopancreas excision (TMpE) in pancreatic tumors. Eur J Surg Oncol. 38:340–345. DOI: 10.1016/j.ejso.2011.12.015. PMID: 22264964.
Article10. Wu W, Wang X, Wu X, Li M, Weng H, Cao Y, et al. 2016; Total mesopancreas excision for pancreatic head cancer: analysis of 120 cases. Chin J Cancer Res. 28:423–428. DOI: 10.21147/j.issn.1000-9604.2016.04.05. PMID: 27647970. PMCID: PMC5018537.
Article11. Xu J, Tian X, Chen Y, Ma Y, Liu C, Tian L, et al. 2017; Total mesopancreas excision for the treatment of pancreatic head cancer. J Cancer. 8:3575–3584. DOI: 10.7150/jca.21341. PMID: 29151943. PMCID: PMC5687173.
Article12. Ramia JM, De-la-Plaza R, Manuel-Vazquez A, Lopez-Marcano A, Morales R. 2018; Systematic review of the mesopancreas: concept and clinical implications. Clin Transl Oncol. 20:1385–1391. DOI: 10.1007/s12094-018-1869-5. PMID: 29675778.
Article13. Nehme F, Lee JH. 2022; Preoperative biliary drainage for pancreatic cancer. Dig Endosc. 34:428–438. DOI: 10.1111/den.14081. PMID: 34275165.
Article14. S , Lahiri RP, Phillips M, Pinn G, Pencavel TD, Kumar R, et al. 2021; Which patients benefit from preoperative biliary drainage in resectable pancreatic cancer? Expert Rev Gastroenterol Hepatol. 15:855–863. DOI: 10.1080/17474124.2021.1915127. PMID: 34036856.
Article15. MG , van Rijssen LB, Bassi C, Dervenis C, Montorsi M, Adham M, et al. 2017; Definition and classification of chyle leak after pancreatic operation: a consensus statement by the International Study Group on Pancreatic Surgery. Surgery. 161:365–372. DOI: 10.1016/j.surg.2016.06.058. PMID: 27692778.
Article16. Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, et al. 2017; The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery. 161:584–591. DOI: 10.1016/j.surg.2016.11.014. PMID: 28040257.
Article17. Amin MB, Greene FL, Edge SB, Compton CC, Gershenwald JE, Brookland RK, et al. 2017; The Eighth Edition AJCC Cancer Staging Manual: continuing to build a bridge from a population-based to a more "personalized" approach to cancer staging. CA Cancer J Clin. 67:93–99. DOI: 10.3322/caac.21388. PMID: 28094848.
Article18. Campbell F, Foulis A, Verbeke C. 2010. Dataset for the histopathological reporting of carcinomas of the pancreas, ampulla of Vater and common bile duct [Internet]. The Royal College of Pathologists;Available from: https://www.rcpath.org/static/34910231-c106-4629-a2de9e9ae6f87ac1/g091-pancreasdataset-mar17.pdf. cited 2023 May 22.19. Isaji S, Murata Y, Kishiwada M. Neoptolemos JP, Urrutia R, Abbruzzese JL, Büchler MW, editors. 2018. New Japanese Classification of Pancreatic Cancer. Pancreatic Cancer. Springer New York;p. 1021–1037. DOI: 10.1007/978-1-4939-7193-0_84.
Article20. Peparini N. 2015; Mesopancreas: a boundless structure, namely the rationale for dissection of the paraaortic area in pancreaticoduodenectomy for pancreatic head carcinoma. World J Gastroenterol. 21:2865–2870. DOI: 10.3748/wjg.v21.i10.2865. PMID: 25780282. PMCID: PMC4356904.
Article21. Khiem T, Hoi H, Hiep T, Khue K, Duy V, Inoue Y, et al. 2022; Total laparoscopic pancreaticoduodenectomy with left posterior superior mesenteric artery first-approach and plexus-preserving circumferential lymphadenectomy: step-by-step technique with a surgical case report (with video). World J Surg Oncol. 20:269. DOI: 10.1186/s12957-022-02730-y. PMID: 36028841. PMCID: PMC9419321.
Article22. Hackert T, Werner J, Weitz J, Schmidt J, Büchler MW. 2010; Uncinate process first--a novel approach for pancreatic head resection. Langenbecks Arch Surg. 395:1161–1164. DOI: 10.1007/s00423-010-0663-9. PMID: 20582600.
Article23. Weitz J, Rahbari N, Koch M, Büchler MW. 2010; The "artery first" approach for resection of pancreatic head cancer. J Am Coll Surg. 210:e1–e4. DOI: 10.1016/j.jamcollsurg.2009.10.019. PMID: 20113929.
Article24. Tol JA, Gouma DJ, Bassi C, Dervenis C, Montorsi M, Adham M, et al. 2014; Definition of a standard lymphadenectomy in surgery for pancreatic ductal adenocarcinoma: a consensus statement by the International Study Group on Pancreatic Surgery (ISGPS). Surgery. 156:591–600. DOI: 10.1016/j.surg.2014.06.016. PMID: 25061003.
Article25. Coco D, Leanza S, Guerra F. 2019; Total pancreatectomy: indications, advantages and disadvantages - a review. Maedica (Bucur). 14:391–396.26. Nguyen TK, Nguyen HH, Nguyen CL, Luong TH, Dinh LD, Le VD, et al. 2022; Case report: Candidiasis of gastrojejunostomosis after pancreaticoduodenectomy: preliminary experience from two cases. Front Oncol. 12:888927. DOI: 10.3389/fonc.2022.888927. PMID: 36091142. PMCID: PMC9449841.
Article27. Nguyen TK, Luong TH, Nguyen NC, Nguyen HH, Le VK, Trinh HS, et al. 2021; Hepatic lymphorrhea following pancreaticoduodenectomy: preliminary diagnosis and treatment experience from case series of four patients. Ann Med Surg (Lond). 68:102648. DOI: 10.1016/j.amsu.2021.102648. PMID: 34386232. PMCID: PMC8346360.
Article28. Pessaux P, Varma D, Arnaud JP. 2006; Pancreaticoduodenectomy: superior mesenteric artery first approach. J Gastrointest Surg. 10:607–611. DOI: 10.1016/j.gassur.2005.05.001. PMID: 16627229.
Article29. Tempero MA, Malafa MP, Al-Hawary M, Behrman SW, Benson AB, Cardin DB, et al. 2021; Pancreatic Adenocarcinoma, Version 2.2021, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 19:439–457. DOI: 10.6004/jnccn.2021.0017. PMID: 33845462.
Article30. Sanjay P, Takaori K, Govil S, Shrikhande SV, Windsor JA. 2012; 'Artery- first' approaches to pancreatoduodenectomy. Br J Surg. 99:1027–1035. DOI: 10.1002/bjs.8763. PMID: 22569924.31. Nagakawa Y, Watanabe Y, Kozono S, Boggi U, Palanivelu C, Liu R, et al. 2021; Surgical approaches to the superior mesenteric artery during minimally invasive pancreaticoduodenectomy: a systematic review. J Hepatobiliary Pancreat Sci. 29:114–123. DOI: 10.1002/jhbp.905. PMID: 33523604.
Article32. Einama T, Takihata Y, Aosasa S, Konno F, Kobayashi K, Yonamine N, et al. 2023; Prognosis of pancreatic cancer based on resectability: a single center experience. Cancers (Basel). 15:1101. DOI: 10.3390/cancers15041101. PMID: 36831444. PMCID: PMC9954753.
Article33. Okada K, Murakami Y, Kondo N, Uemura K, Nakagawa N, Seo S, et al. 2019; prognostic significance of lymph node metastasis and micrometastasis along the left side of superior mesenteric artery in pancreatic head cancer. J Gastrointest Surg. 23:2100–2109. DOI: 10.1007/s11605-019-04359-x. PMID: 31410820.
Article34. Kondo N, Uemura K, Nakagawa N, Okada K, Seo S, Takahashi S, et al. 2020; Superior mesenteric artery plexus-preserving pancreatoduodenectomy with circumferential dissection of lymph nodes. J Gastrointest Surg. 24:1712–1719. DOI: 10.1007/s11605-020-04629-z. PMID: 32410173.
Article35. Kim JR, Kim H, Kwon W, Jang JY, Kim SW. 2021; Pattern of local recurrence after curative resection in pancreatic ductal adenocarcinoma according to the initial location of the tumor. J Hepatobiliary Pancreat Sci. 28:105–114. DOI: 10.1002/jhbp.854. PMID: 33084211.
Article36. Kang MJ, Kim SW. 2020; En bloc proximal peri-mesenteric clearance for pancreatic head cancer surgery. Ann Hepatobiliary Pancreat Surg. 24:389–395. DOI: 10.14701/ahbps.2020.24.4.389. PMID: 33234741. PMCID: PMC7691194.
Article37. Gaedcke J, Gunawan B, Grade M, Szöke R, Liersch T, Becker H, et al. 2010; The mesopancreas is the primary site for R1 resection in pancreatic head cancer: relevance for clinical trials. Langenbecks Arch Surg. 395:451–458. DOI: 10.1007/s00423-009-0494-8. PMID: 19418067. PMCID: PMC2848727.
Article38. Inoue Y, Saiura A, Yoshioka R, Ono Y, Takahashi M, Arita J, et al. 2015; Pancreatoduodenectomy with systematic mesopancreas dissection using a supracolic anterior artery-first approach. Ann Surg. 262:1092–1101. DOI: 10.1097/SLA.0000000000001065. PMID: 25587814.
Article39. Ramia JM, De-la-Plaza R, Manuel-Vazquez A, Lopez-Marcano A, Morales R. 2018; Systematic review of the mesopancreas: concept and clinical implications. Clin Transl Oncol. 20:1385–1391. DOI: 10.1007/s12094-018-1869-5. PMID: 29675778.
Article40. Kuroki N, Ono Y, Sato T, Inoue Y, Oba A, Ito H, et al. 2022; Long-term outcome of patients with postoperative refractory diarrhea after tailored nerve plexus dissection around the major visceral arteries during pancreatoduodenectomy for pancreatic cancer. World J Surg. 46:1172–1182. DOI: 10.1007/s00268-022-06457-5. PMID: 35119513.
Article41. Inoue Y, Saiura A, Oba A, Kawakatsu S, Ono Y, Sato T, et al. 2019; Optimal extent of superior mesenteric artery dissection during pancreaticoduodenectomy for pancreatic cancer: balancing surgical and oncological safety. J Gastrointest Surg. 23:1373–1383. DOI: 10.1007/s11605-018-3995-3. PMID: 30306451.
Article42. Hackert T, Strobel O, Michalski CW, Mihaljevic AL, Mehrabi A, Müller-Stich B, et al. 2017; The TRIANGLE operation - radical surgery after neoadjuvant treatment for advanced pancreatic cancer: a single arm observational study. HPB (Oxford). 19:1001–1007. DOI: 10.1016/j.hpb.2017.07.007. PMID: 28838632.
Article43. Nguyen LT, Do DH, Van Nguyen H, Nguyen KT, Nguyen CD. 2022; Lymph node characteristics and short-term outcomes for resectable pancreatic ductal adenocarcinoma in vietnam: a retrospective single-center study. Indian J Surg. 84:458–463. DOI: 10.1007/s12262-022-03344-0.
Article44. Torres SM, Vaz da Silva DG, Ribeiro HSC, Diniz AL, Lobo MM, de Godoy AL, et al. 2020; Short-term outcomes after vascular resection for pancreatic tumors: lessons learned from 72 cases from a single Brazilian Cancer Center. J Surg Oncol. 121:857–862. DOI: 10.1002/jso.25799. PMID: 31808559.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- En bloc proximal peri-mesenteric clearance for pancreatic head cancer surgery
- One hundred sixty pancreaticoduodenectomies for periampullary cancers in a growing-volume setting: a single-institution and a single-surgeon's experience
- Laparoscopic pancreaticoduodenectomy with excision of aberrant right hepatic artery after preoperative segmental embolization in mid-bile duct cancer
- Laparoscopic total pancreatectomy with total mesopancreas dissection using counterclockwise technique and tail-first approach
- Short Bowel Syndrome Due to Infarction of the Superior Mesenteric Artery