Ann Hepatobiliary Pancreat Surg.
2024 Feb;28(1):53-58. 10.14701/ahbps.23-063.
Incidental double duct sign: Should we be worried? Results from a long-term follow-up study
- Affiliations
-
- 1Department of HPB Surgery, University of Plymouth, Plymouth, UK
- KMID: 2553366
- DOI: http://doi.org/10.14701/ahbps.23-063
Abstract
- Backgrounds/Aims
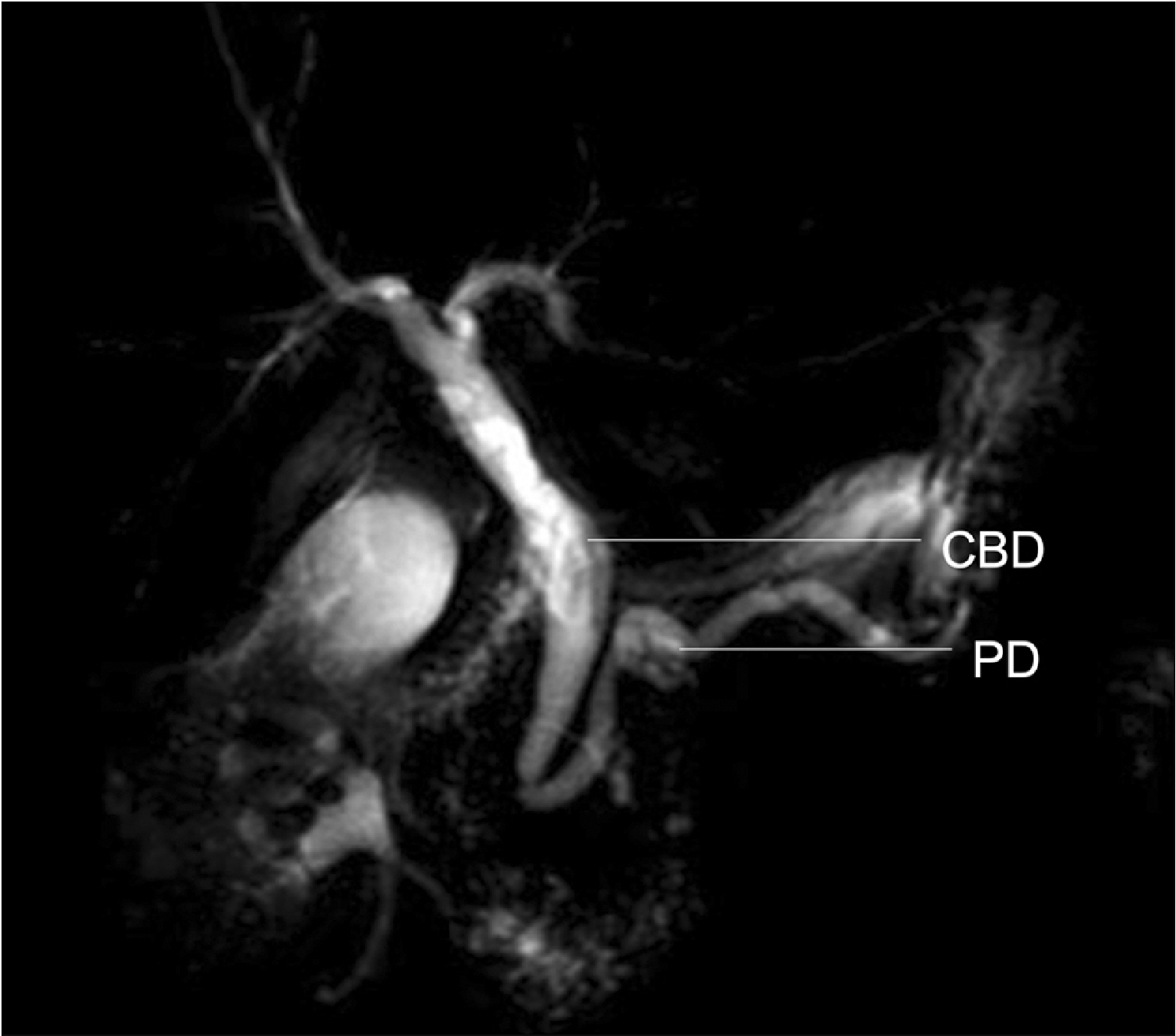
Double duct sign (DDS) (dilated common bile and pancreatic duct) is synonymous with pancreatic head/ peri-ampullary tumor (PHPAT). There is limited evidence on whether incidental DDS (I-DDS) is associated with an increased risk of malignancy. This study aimed to evaluate 5-year outcomes of I-DDS.
Methods
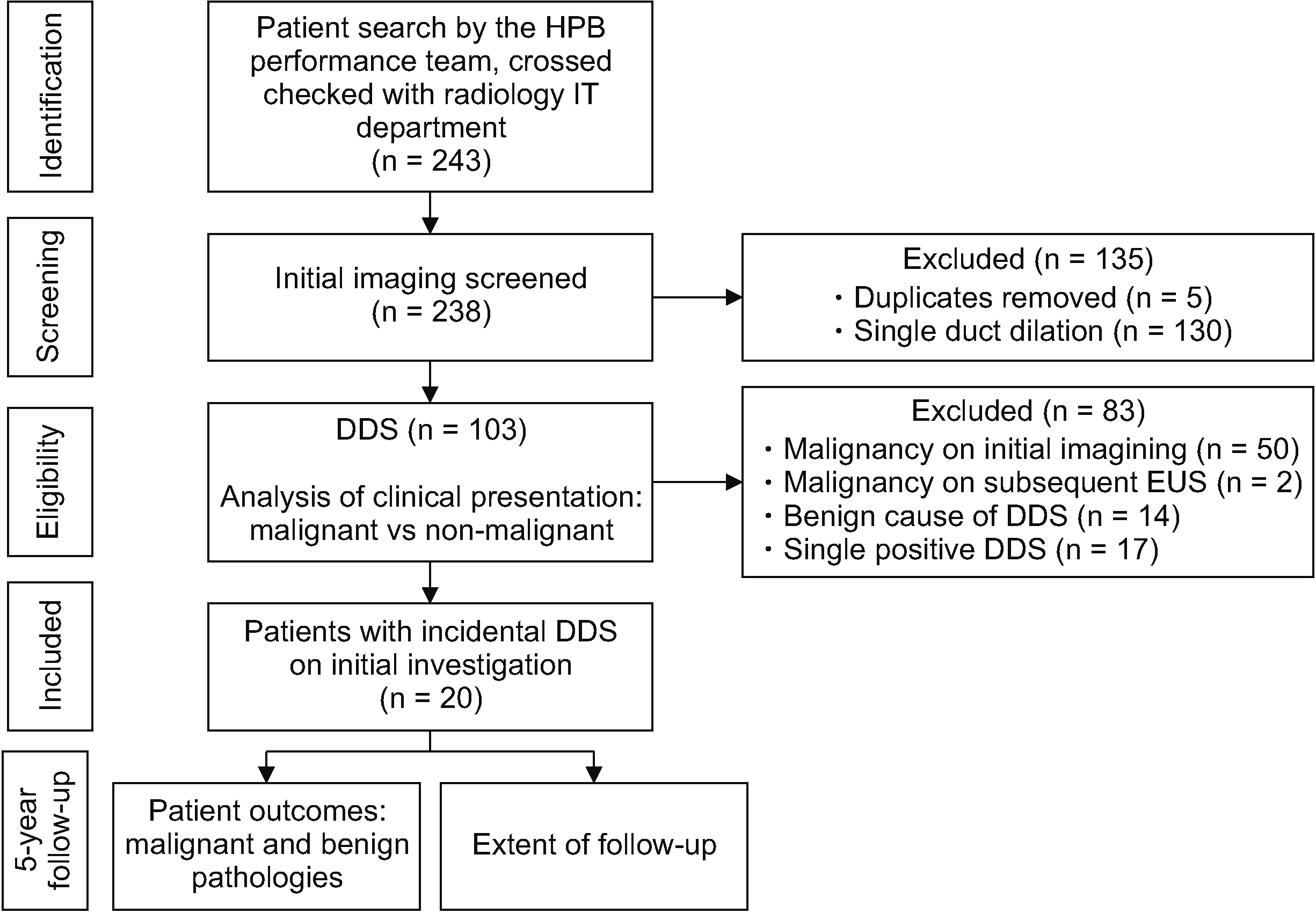
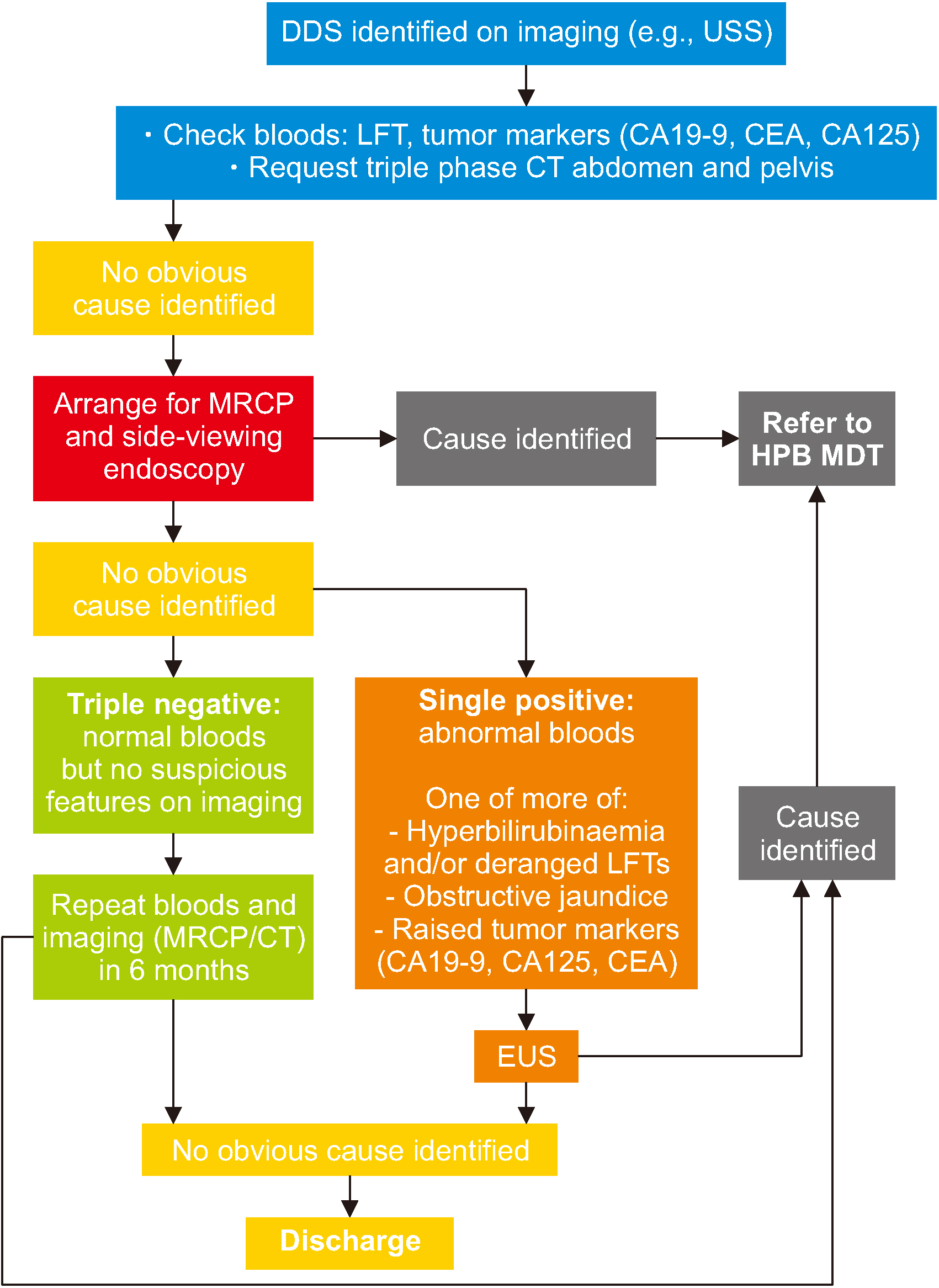
Patients were categorized according to their risk of malignancy. ‘Low-risk’ patients, including those with I-DDS between 2010 and 2015, were analyzed in this study. The primary outcome was incidence of PHPAT within five years of identification of DDS. Histology results from endoscopic ultrasound-guided biopsy were considered diagnostic. Secondary outcomes were incidence of benign causes, extent of follow-up investigations, and clinical indicators of malignancy in patients with DDS.
Results
Among 103 patients with DDS, 20 had I-DDS. Subsequent follow-up of these 20 patients found no patient with PHPAT, two (10%) patients with chronic pancreatitis, and 18 (90%) patients with no cause found. The median follow-up duration for ‘low-risk’ patients was 7.3 years (range, 6–11 years). The mean number of follow-up investigations per patient was two (range, 0–9). Investigations included computed tomography (n = 27), magnetic resonance cholangiopancreatography (n = 23), endoscopy (n = 16), and ultrasound (n = 14). Patients with jaundice were more likely to have malignancy (p < 0.01). Those with abdominal pain were more likely to have a benign cause (p < 0.01). Hyperbilirubinemia and/or deranged liver enzymes and raised CA19-9 were more likely to be associated with PHPAT (p < 0.01).
Conclusions
Patients with I-DDS have a low risk of developing PHPAT within five years.
Keyword
Figure
Reference
-
1. Ahualli J. 2007; The double duct sign. Radiology. 244:314–315. DOI: 10.1148/radiol.2441041978. PMID: 17581912.
Article2. Yadav P, Lal H. 2017; Double duct sign. Abdom Radiol (NY). 42:1283–1284. DOI: 10.1007/s00261-016-0979-1. PMID: 27837241.
Article3. Sinha R, Gardner T, Padala K, Greenaway JR, Joy D. 2015; Double-duct sign in the clinical context. Pancreas. 44:967–970. DOI: 10.1097/MPA.0000000000000372. PMID: 26087354.
Article4. Baillie J, Paulson EK, Vitellas KM. 2003; Biliary imaging: a review. Gastroenterology. 124:1686–1699. DOI: 10.1016/S0016-5085(03)00390-1. PMID: 12761726.5. Cohen J, Sawhney MS, Pleskow DK, Chuttani R, Patel NJ, Sheridan J, et al. 2014; Double-duct sign in the era of endoscopic ultrasound: the prevalence of occult pancreaticobiliary malignancy. Dig Dis Sci. 59:2280–2285. DOI: 10.1007/s10620-014-3133-3. PMID: 24705640.
Article6. Wolske KM, Ponnatapura J, Kolokythas O, Burke LMB, Tappouni R, Lalwani N. 2019; Chronic pancreatitis or pancreatic tumor? a problem- solving approach. Radiographics. 39:1965–1982. DOI: 10.1148/rg.2019190011. PMID: 31584860.
Article7. Menges M, Lerch MM, Zeitz M. 2000; The double duct sign in patients with malignant and benign pancreatic lesions. Gastrointest Endosc. 52:74–77. DOI: 10.1067/mge.2000.105775. PMID: 10882966.
Article8. Gangi S, Fletcher JG, Nathan MA, Christensen JA, Harmsen WS, Crownhart BS, et al. 2004; Time interval between abnormalities seen on CT and the clinical diagnosis of pancreatic cancer: retrospective review of CT scans obtained before diagnosis. AJR Am J Roentgenol. 182:897–903. DOI: 10.2214/ajr.182.4.1820897. PMID: 15039161.
Article9. Krishna N, Tummala P, Reddy AV, Mehra M, Agarwal B. 2012; Dilation of both pancreatic duct and the common bile duct on computed tomography and magnetic resonance imaging scans in patients with or without obstructive jaundice. Pancreas. 41:767–772. DOI: 10.1097/MPA.0b013e31823ba536. PMID: 22450366.
Article10. Malik S, Kaushik N, Khalid A, Bauer K, Brody D, Slivka A, et al. 2007; EUS yield in evaluating biliary dilatation in patients with normal serum liver enzymes. Dig Dis Sci. 52:508–512. DOI: 10.1007/s10620-006-9582-6. PMID: 17211694.
Article11. Coss A, Enns R. 2009; The investigation of unexplained biliary dilatation. Curr Gastroenterol Rep. 11:155–159. DOI: 10.1007/s11894-009-0024-4. PMID: 19281704.
Article12. Agarwal B, Krishna NB, Labundy J, Safdar R, Akduman EI. 2008; EUS and/or EUS-guided FNA in patients with CT and/or magnetic resonance imaging findings of enlarged pancreatic head or dilated pancreatic duct with or without a dilated common bile duct. Gastrointest Endosc. 68:237–242. DOI: 10.1016/j.gie.2008.01.026. PMID: 18423464.
Article13. Thomasset SC, Saunders D, Holland A, Dennison AR, Garcea G. 2015; Malignant biliary strictures in patients with a normal bilirubin and/or normal liver enzymes. HPB (Oxford). 17:969–974. DOI: 10.1111/hpb.12468. PMID: 26256123. PMCID: PMC4605334.
Article14. Natalucci V, Virgili E, Calcagnoli F, Valli G, Agostini D, Zeppa SD, et al. 2021; Cancer related anemia: an integrated multitarget approach and lifestyle interventions. Nutrients. 13:482. DOI: 10.3390/nu13020482. PMID: 33535496. PMCID: PMC7912724.
Article15. McGuigan A, Kelly P, Turkington R, Jones C, Coleman HG, McCain RS. 2018; Pancreatic cancer: a review of clinical diagnosis, epidemiology, treatment and outcomes. World J Gastroenterol. 24:4846–4861. DOI: 10.3748/wjg.v24.i43.4846. PMID: 30487695. PMCID: PMC6250924.
Article16. Paluri RK, Kasi A. 2022. Ampullary Cancer [Internet]. StatPearls Publishing;Available from: https://www.ncbi.nlm.nih.gov/books/NBK555958/. cited 2022 Dec 22.17. Gardner T, Padala K, Sinha R, Greenaway J, Joy D. 2014; PTH-105 how ominous is the "double-duct" sign? a single centre experience. Gut. 63:A257. DOI: 10.1136/gutjnl-2014-307263.551.18. Safi F, Roscher R, Bittner R, Schenkluhn B, Dopfer HP, Beger HG. 1987; High sensitivity and specificity of CA 19-9 for pancreatic carcinoma in comparison to chronic pancreatitis. Serological and immunohistochemical findings. Pancreas. 2:398–403. DOI: 10.1097/00006676-198707000-00006. PMID: 3306667.
Article19. Ni XG, Bai XF, Mao YL, Shao YF, Wu JX, Shan Y, et al. 2005; The clinical value of serum CEA, CA19-9, and CA242 in the diagnosis and prognosis of pancreatic cancer. Eur J Surg Oncol. 31:164–169. DOI: 10.1016/j.ejso.2004.09.007. PMID: 15698733.
Article20. Mizuide M, Ryozawa S, Fujita A, Ogawa T, Katsuda H, Suzuki M, et al. 2020; Complications of endoscopic ultrasound-guided fine needle aspiration: a narrative review. Diagnostics (Basel). 10:964. DOI: 10.3390/diagnostics10110964. PMID: 33213103. PMCID: PMC7698484.
Article21. National Institute for Health and Care Excellence (NICE). 2015. The SpyGlass direct visualisation system for diagnostic and therapeutic procedures during endoscopy of the biliary system [MIB21] [Internet]. NICE;Available from: https://www.nice.org.uk/advice/mib21. cited 2022 Dec 22.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Long Term Effect of Double Silicone Tube Intubation for Acquired Nasolacrimal Duct Obstruction
- The Double Papilla of Vater
- A Case of Synchronous Double Primary Cancer Associated with the Biliary Tract
- Long-term follow-up study and long-term care of childhood cancer survivors
- Double Primary Cancer of the Gallbladder and Cystic Duct: A Case Report