J Korean Med Sci.
2024 Mar;39(9):e82. 10.3346/jkms.2024.39.e82.
Opioid Prescription and Long-Term Survival Outcomes in Adults: A Nationwide Cohort Study in Korea
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
- 2Department of Anesthesiology and Pain Medicine, College of Medicine, Seoul National University, Seoul, Korea
- KMID: 2553334
- DOI: http://doi.org/10.3346/jkms.2024.39.e82
Abstract
- Background
We aimed to investigate the association between short- and long-term opioid use and long-term mortality in Korea.
Methods
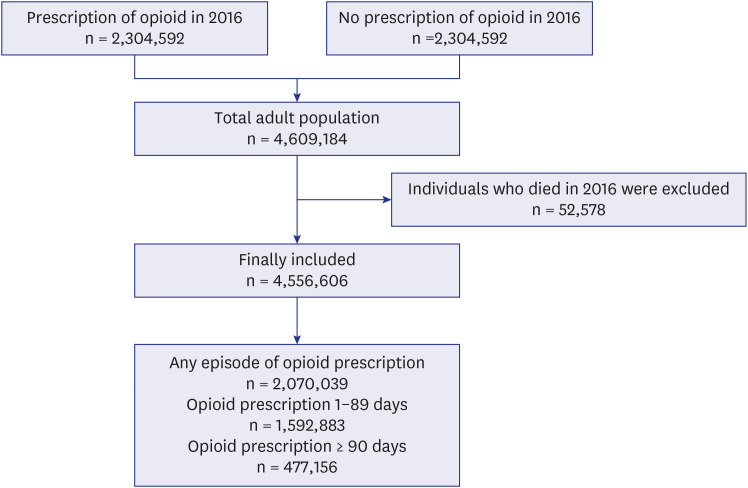
In this population-based retrospective cohort study, data were obtained from the National Health Insurance Service of South Korea. The study included all adult individuals who were prescribed opioids in 2016. The control group comprised adults not prescribed opioids in 2016 selected using a 1:1 stratified random sampling technique. Participants were categorized into three groups: non-user, opioid 1–89 days user (short-term), and opioid ≥ 90 days user (long-term) groups. The primary endpoint in this study was 5-year all-cause mortality, evaluated from January 1, 2017 to December 31, 2021.
Results
In total, 4,556,606 adults were included in this study. Of these, 2,070,039 were prescribed opioids at least once. Specifically, 1,592,883 adult individuals were prescribed opioids for 1–89 days, while 477,156 adults were prescribed opioid for ≥ 90 days. In the multivariable Cox regression modelling, the opioid user group had a 28% (hazard ratio [HR], 1.28; 95% confidence interval [95% CI], 1.26–1.29; P < 0.001) higher risk of 5-year all-cause mortality than had the non-user group. Moreover, the opioid 1–89 days and opioid ≥ 90 days user groups had 15% (HR, 1.15; 95% CI, 1.14–1.17; P < 0.001) and 49% (HR, 1.49; 95% CI, 1.47–1.51; P < 0.001) higher risks of 5-year all-cause mortality than had the non-user group, respectively.
Conclusion
Both short and long-term opioid prescriptions were associated with increased long-term mortality among the Korean adult population.
Keyword
Figure
Reference
-
1. Judd D, King CR, Galke C. The opioid epidemic: a review of the contributing factors, negative consequences, and best practices. Cureus. 2023; 15(7):e41621. PMID: 37565101.2. Ballantyne JC, LaForge SK. Opioid dependence and addiction during opioid treatment of chronic pain. Pain. 2007; 129(3):235–255. PMID: 17482363.3. Celentano D. The worldwide opioid pandemic: epidemiologic perspectives. Epidemiol Rev. 2020; 42(1):1–3. PMID: 33355347.4. Robert M, Jouanjus E, Khouri C, Fouilhé Sam-Laï N, Revol B. The opioid epidemic: a worldwide exploratory study using the WHO pharmacovigilance database. Addiction. 2023; 118(4):771–775. PMID: 36331523.5. Benyamin R, Trescot AM, Datta S, Buenaventura R, Adlaka R, Sehgal N, et al. Opioid complications and side effects. Pain Physician. 2008; 11(2):Suppl. S105–S120. PMID: 18443635.6. Rogers TJ, Roy S. Editorial: The role of opioid receptors in immune system function. Front Immunol. 2022; 12:832292. PMID: 35082800.7. Baldini A, Von Korff M, Lin EH. A review of potential adverse effects of long-term opioid therapy: a practitioner’s guide. Prim Care Companion CNS Disord. 2012; 14(3):27252.8. Ekholm O, Kurita GP, Hjsted J, Juel K, Sjgren P. Chronic pain, opioid prescriptions, and mortality in Denmark: a population-based cohort study. Pain. 2014; 155(12):2486–2490. PMID: 25020002.9. Lee PF, Li CY, Liu YC, Chiu CT, Hou WH. Population-based study on the all-cause and cause-specific risks of mortality among long-term opioid analgesics users without cancer in Taiwan. Healthcare (Basel). 2021; 9(11):1402. PMID: 34828449.10. Pearce LA, Min JE, Piske M, Zhou H, Homayra F, Slaunwhite A, et al. Opioid agonist treatment and risk of mortality during opioid overdose public health emergency: population based retrospective cohort study. BMJ. 2020; 368:m772. PMID: 32234712.11. Oh TK, Jeon YT, Choi JW. Trends in chronic opioid use and association with five-year survival in South Korea: a population-based cohort study. Br J Anaesth. 2019; 123(5):655–663. PMID: 31558315.12. Song IA, Choi HR, Oh TK. Long-term opioid use and mortality in patients with chronic non-cancer pain: Ten-year follow-up study in South Korea from 2010 through 2019. EClinicalMedicine. 2022; 51:101558. PMID: 35875817.13. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007; 370(9596):1453–1457. PMID: 18064739.14. Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort profile: the national health insurance service–national sample cohort (NHIS-NSC), South Korea. Int J Epidemiol. 2017; 46(2):e15. PMID: 26822938.15. Zin CS, Nazar NI, Rahman NS, Ahmad WR, Rani NS, Ng KS. Patterns of initial opioid prescription and its association with short-term and long-term use among opioid-naïve patients in Malaysia: a retrospective cohort study. BMJ Open. 2019; 9(7):e027203.16. van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care. 2009; 47(6):626–633. PMID: 19433995.17. Martell BA, O’Connor PG, Kerns RD, Becker WC, Morales KH, Kosten TR, et al. Systematic review: opioid treatment for chronic back pain: prevalence, efficacy, and association with addiction. Ann Intern Med. 2007; 146(2):116–127. PMID: 17227935.18. Chen Q, Larochelle MR, Weaver DT, Lietz AP, Mueller PP, Mercaldo S, et al. Prevention of prescription opioid misuse and projected overdose deaths in the United States. JAMA Netw Open. 2019; 2(2):e187621. PMID: 30707224.19. Florence CS, Zhou C, Luo F, Xu L. The economic burden of prescription opioid overdose, abuse, and dependence in the United States, 2013. Med Care. 2016; 54(10):901–906. PMID: 27623005.20. Kim J, Shin SJ, Yoon J, Kim HS, Lee JW, Kim YS, et al. Recent trends in opioid prescriptions in Korea from 2002 to 2015 based on the Korean NHIS-NSC cohort. Epidemiol Health. 2022; 44:e2022029. PMID: 35209705.21. Von Korff M, Kolodny A, Deyo RA, Chou R. Long-term opioid therapy reconsidered. Ann Intern Med. 2011; 155(5):325–328. PMID: 21893626.22. Bateman JT, Saunders SE, Levitt ES. Understanding and countering opioid-induced respiratory depression. Br J Pharmacol. 2023; 180(7):813–828. PMID: 34089181.23. Freire C, Sennes LU, Polotsky VY. Opioids and obstructive sleep apnea. J Clin Sleep Med. 2022; 18(2):647–652. PMID: 34672945.24. Diasso PD, Birke H, Nielsen SD, Main KM, Højsted J, Sjøgren P, et al. The effects of long-term opioid treatment on the immune system in chronic non-cancer pain patients: a systematic review. Eur J Pain. 2020; 24(3):481–496. PMID: 31705699.25. Edelman EJ, Gordon KS, Crothers K, Akgün K, Bryant KJ, Becker WC, et al. Association of prescribed opioids with increased risk of community-acquired pneumonia among patients with and without HIV. JAMA Intern Med. 2019; 179(3):297–304. PMID: 30615036.26. Kosciuczuk U, Knapp P, Lotowska-Cwiklewska AM. Opioid-induced immunosuppression and carcinogenesis promotion theories create the newest trend in acute and chronic pain pharmacotherapy. Clinics (Sao Paulo). 2020; 75:e1554. PMID: 32215455.27. Carman WJ, Su S, Cook SF, Wurzelmann JI, McAfee A. Coronary heart disease outcomes among chronic opioid and cyclooxygenase-2 users compared with a general population cohort. Pharmacoepidemiol Drug Saf. 2011; 20(7):754–762. PMID: 21567652.28. Solin AV, Lyashev AY, Lyashev YD. Effects of opioid peptides on changes in lipid metabolism in rats subjected to swimming stress. Bull Exp Biol Med. 2017; 162(3):313–315. PMID: 28091903.29. Foley HE, Knight JC, Ploughman M, Asghari S, Audas R. Association of chronic pain with comorbidities and health care utilization: a retrospective cohort study using health administrative data. Pain. 2021; 162(11):2737–2749. PMID: 33902092.30. King LK, Marshall DA, Jones CA, Woodhouse LJ, Ravi B, Faris PD, et al. Are medical comorbidities contributing to the use of opioid analgesics in patients with knee osteoarthritis? Osteoarthritis Cartilage. 2020; 28(8):1030–1037. PMID: 32387761.31. Kaplan GA, Pamuk ER, Lynch JW, Cohen RD, Balfour JL. Inequality in income and mortality in the United States: analysis of mortality and potential pathways. BMJ. 1996; 312(7037):999–1003. PMID: 8616393.32. GBD 2015 Healthcare Access and Quality Collaborators. Healthcare Access and Quality Index based on mortality from causes amenable to personal health care in 195 countries and territories, 1990–2015: a novel analysis from the Global Burden of Disease Study 2015. Lancet. 2017; 390(10091):231–266. PMID: 28528753.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Association between Levetiracetam Use and Survival in Patients with Glioblastoma: A Nationwide Population-Based Study
- Trends in the prescription of opioids and gabapentinoids in patients with failed back surgery syndrome in Korea: a population-based study
- Education regarding opioid prescription within oral and maxillofacial surgery residency programs: a survey study
- Proportion of Non-Medical Opioid Use of Prescription Opioids among Cancer Patients in Korea
- Effect of Opioids on All-cause Mortality and Opioid Addiction in Total Hip Arthroplasty: a Korea Nationwide Cohort Study