Child Kidney Dis.
2024 Feb;28(1):1-7. 10.3339/ckd.24.002.
Antenatally detected urinary tract dilatation: a pediatric nephrologist's point of view
- KMID: 2553174
- DOI: http://doi.org/10.3339/ckd.24.002
Abstract
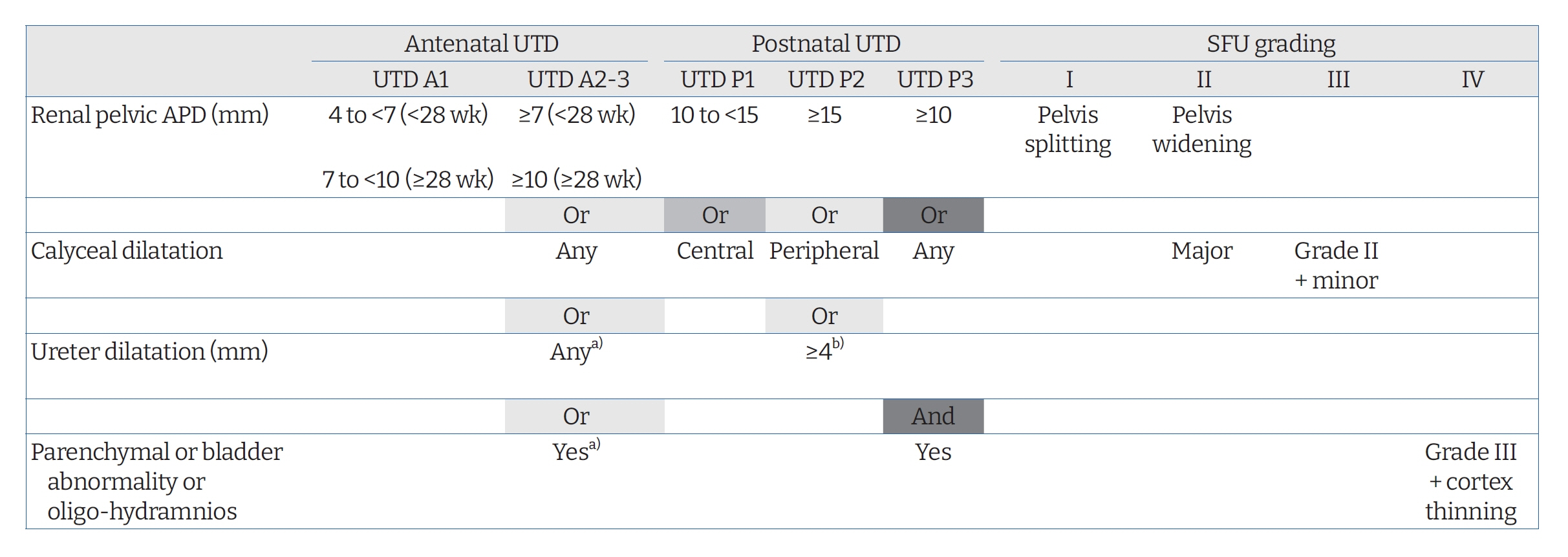
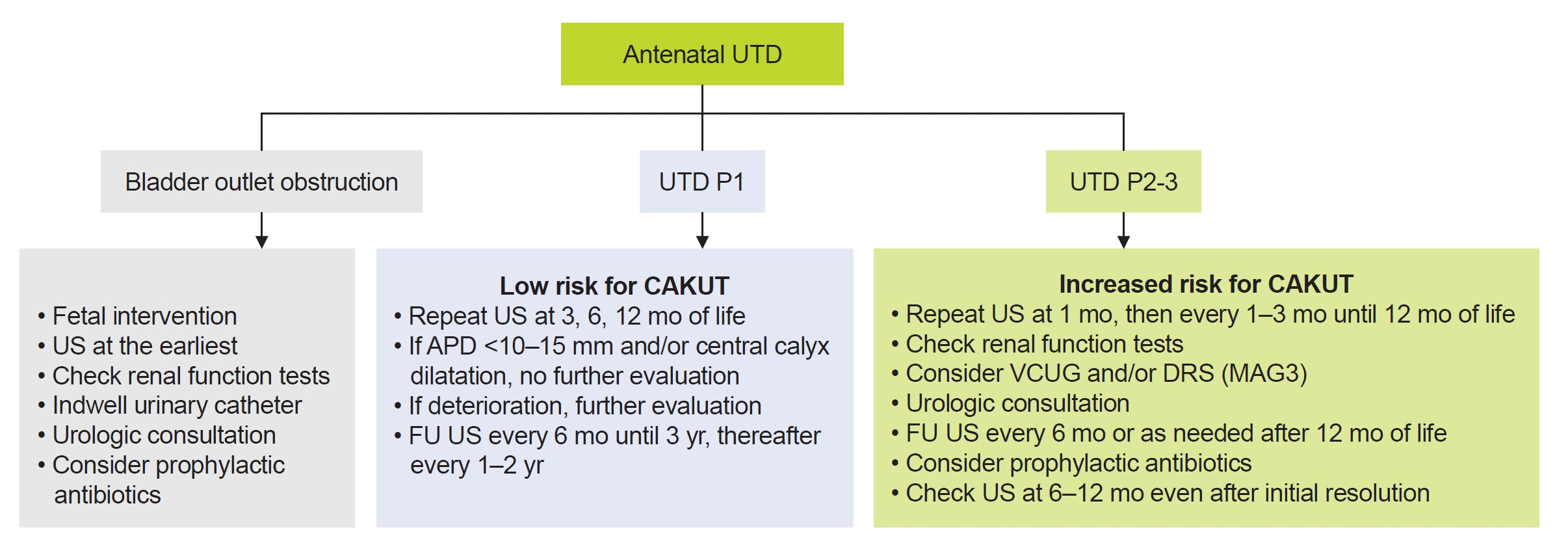
- Antenatally diagnosed urinary tract dilatation (UTD), previously referred to as antenatal hydronephrosis, is the most commonly detected abnormality by prenatal ultrasonography. Several grading systems have been developed for the classification of antenatal UTD using prenatal and postnatal ultrasonography. UTD comprises a wide variety of congenital abnormalities of the kidney and urinary tract ranging from transient UTD to more significant abnormalities such as vesicoureteral reflux, ureteropelvic junction obstruction, ureterocele, ureterovesical junction obstruction, posterior urethral valves, and non-refluxing megaureter. Optimizing the evaluation of antenatally detected UTD is essential to recognize children with important disorders while avoiding excessive investigations. Conservative approach with close follow-up is increasingly accepted as an appropriate treatment option for patients with asymptomatic vesicoureteral reflux and ureteropelvic junction obstruction in recent years. However, predicting permanent kidney damage in an unselected group of children with antenatal UTD is still challenging. The management and follow-up of children with UTD should be individualized based on recommendations from a pediatric nephrologist, a pediatric urologist, or both. Future research directed at predicting long-term outcomes of children diagnosed with UTD from mild findings to severe disease is needed to refine management for those at higher risk of kidney disease progression.
Figure
Reference
-
References
1. Ismaili K, Hall M, Donner C, Thomas D, Vermeylen D, Avni FE, et al. Results of systematic screening for minor degrees of fetal renal pelvis dilatation in an unselected population. Am J Obstet Gynecol. 2003; 188:242–6.
Article2. Feldman DM, DeCambre M, Kong E, Borgida A, Jamil M, McKenna P, et al. Evaluation and follow-up of fetal hydronephrosis. J Ultrasound Med. 2001; 20:1065–9.
Article3. Herthelius M. Antenatally detected urinary tract dilatation: long-term outcome. Pediatr Nephrol. 2023; 38:3221–7.
Article4. Nguyen HT, Phelps A, Coley B, Darge K, Rhee A, Chow JS. 2021 update on the urinary tract dilation (UTD) classification system: clarifications, review of the literature, and practical suggestions. Pediatr Radiol. 2022; 52:740–51.
Article5. Kim SY, Kim MJ, Yoon CS, Lee MS, Han KH, Lee MJ. Comparison of the reliability of two hydronephrosis grading systems: the Society for Foetal Urology grading system vs. the Onen grading system. Clin Radiol. 2013; 68:e484–90.
Article6. Melo FF, Mak RH, Simoes E Silva AC, Vasconcelos MA, Dias CS, Rosa LC, et al. Evaluation of urinary tract dilation classification system for prediction of long-term outcomes in isolated antenatal hydronephrosis: a cohort study. J Urol. 2021; 206:1022–30.
Article7. Melo FF, Vasconcelos MA, Mak RH, Silva AC, Dias CS, Colosimo EA, et al. Postnatal urinary tract dilatation classification: improvement of the accuracy in predicting kidney injury. Pediatr Nephrol. 2022; 37:613–23.
Article8. Hwang J, Kim PH, Yoon HM, Song SH, Jung AY, Lee JS, et al. Application of the postnatal urinary tract dilation classification system to predict the need for surgical intervention among neonates and young infants. Ultrasonography. 2023; 42:136–46.
Article9. Nguyen HT, Benson CB, Bromley B, Campbell JB, Chow J, Coleman B, et al. Multidisciplinary consensus on the classification of prenatal and postnatal urinary tract dilation (UTD classification system). J Pediatr Urol. 2014; 10:982–98.
Article10. Lee RS, Cendron M, Kinnamon DD, Nguyen HT. Antenatal hydronephrosis as a predictor of postnatal outcome: a meta-analysis. Pediatrics. 2006; 118:586–93.
Article11. Jain S, Chen F. Developmental pathology of congenital kidney and urinary tract anomalies. Clin Kidney J. 2018; 12:382–99.
Article12. Mallik M, Watson AR. Antenatally detected urinary tract abnormalities: more detection but less action. Pediatr Nephrol. 2008; 23:897–904.
Article13. Aksu N, Yavascan O, Kangin M, Kara OD, Aydin Y, Erdogan H, et al. Postnatal management of infants with antenatally detected hydronephrosis. Pediatr Nephrol. 2005; 20:1253–9.
Article14. Deshpande AV. Conversations for the future in the follow-up of antenatally diagnosed renal pelvicalyceal dilatation. Pediatr Nephrol. 2021; 36:5–8.
Article15. Roos JF, Doust J, Tett SE, Kirkpatrick CM. Diagnostic accuracy of cystatin C compared to serum creatinine for the estimation of renal dysfunction in adults and children: a meta-analysis. Clin Biochem. 2007; 40:383–91.16. Matsui F, Shimada K, Matsumoto F, Takano S. Late recurrence of symptomatic hydronephrosis in patients with prenatally detected hydronephrosis and spontaneous improvement. J Urol. 2008; 180:322–5.
Article17. Zee RS, Herndon CD, Cooper CS, Kim C, McKenna PH, Khoury A, et al. Time to resolution: a prospective evaluation from the Society for Fetal Urology hydronephrosis registry. J Pediatr Urol. 2017; 13:316.
Article18. Yang Y, Hou Y, Niu ZB, Wang CL. Long-term follow-up and management of prenatally detected, isolated hydronephrosis. J Pediatr Surg. 2010; 45:1701–6.
Article19. Costa FP, Simoes E Silva AC, Mak RH, Ix JH, Vasconcelos MA, Dias CS, et al. A clinical predictive model of renal injury in children with isolated antenatal hydronephrosis. Clin Kidney J. 2019; 13:834–41.
Article20. Herthelius M, Axelsson R, Lidefelt KJ. Antenatally detected urinary tract dilatation: a 12-15-year follow-up. Pediatr Nephrol. 2020; 35:2129–35.
Article21. Dias CS, Silva JM, Pereira AK, Marino VS, Silva LA, Coelho AM, et al. Diagnostic accuracy of renal pelvic dilatation for detecting surgically managed ureteropelvic junction obstruction. J Urol. 2013; 190:661–6.
Article22. Song SH, Park S, Chae SY, Moon DH, Park S, Kim KS. Predictors of renal functional improvement after pyeloplasty in ureteropelvic junction obstruction: clinical value of visually assessed renal tissue tracer transit in 99mTc-mercaptoacetyltriglycine renography. Urology. 2017; 108:149–54.
Article23. Hodhod A, Capolicchio JP, Jednak R, Eid H, El-Doray AE, El-Sherbiny M. Is the renal pyramidal thickness a good predictor for pyeloplasty in postnatal hydronephrosis? J Pediatr Urol. 2018; 14:277.
Article24. Rickard M, Lorenzo AJ, Braga LH. Renal parenchyma to hydronephrosis area ratio (PHAR) as a predictor of future surgical intervention for infants with high-grade prenatal hydronephrosis. Urology. 2017; 101:85–9.
Article25. Walsh TJ, Hsieh S, Grady R, Mueller BA. Antenatal hydronephrosis and the risk of pyelonephritis hospitalization during the first year of life. Urology. 2007; 69:970–4.
Article26. Zareba P, Lorenzo AJ, Braga LH. Risk factors for febrile urinary tract infection in infants with prenatal hydronephrosis: comprehensive single center analysis. J Urol. 2014; 191:1614–8.
Article27. Zee RS, Herbst KW, Kim C, McKenna PH, Bentley T, Cooper CS, et al. Urinary tract infections in children with prenatal hydronephrosis: a risk assessment from the Society for Fetal Urology Hydronephrosis Registry. J Pediatr Urol. 2016; 12:261.
Article28. Visuri S, Jahnukainen T, Taskinen S. Incidence of urinary tract infections in infants with antenatally diagnosed hydronephrosis: a retrospective single center study. J Pediatr Surg. 2017; 52:1503–6.29. Lee JH, Choi HS, Kim JK, Won HS, Kim KS, Moon DH, et al. Nonrefluxing neonatal hydronephrosis and the risk of urinary tract infection. J Urol. 2008; 179:1524–8.
Article30. Coelho GM, Bouzada MC, Pereira AK, Figueiredo BF, Leite MR, Oliveira DS, et al. Outcome of isolated antenatal hydronephrosis: a prospective cohort study. Pediatr Nephrol. 2007; 22:1727–34.
Article31. Sencan A, Carvas F, Hekimoglu IC, Caf N, Sencan A, Chow J, et al. Urinary tract infection and vesicoureteral reflux in children with mild antenatal hydronephrosis. J Pediatr Urol. 2014; 10:1008–13.
Article32. Pennesi M, Amoroso S, Bassanese G, Pintaldi S, Giacomini G, Barbi E. Frequency of urinary tract infection in children with antenatal diagnosis of urinary tract dilatation. Arch Dis Child. 2020; 105:260–3.
Article33. Braga LH, Easterbrook B, Jegatheeswaran K, Lorenzo AJ. From research question to conducting a randomized controlled trial on continuous antibiotic prophylaxis in prenatal hydronephrosis: a rational stepwise process. Front Pediatr. 2016; 4:27.
Article34. Silay MS, Undre S, Nambiar AK, Dogan HS, Kocvara R, Nijman RJ, et al. Role of antibiotic prophylaxis in antenatal hydronephrosis: a systematic review from the European Association of Urology/European Society for Paediatric Urology Guidelines Panel. J Pediatr Urol. 2017; 13:306–15.
Article35. Rianthavorn P, Phithaklimnuwong S. The role of antibiotic prophylaxis in mild to moderate isolated hydronephrosis detected in antenatal screening. Investig Clin Urol. 2020; 61:200–6.
Article36. Nef S, Neuhaus TJ, Sparta G, Weitz M, Buder K, Wisser J, et al. Outcome after prenatal diagnosis of congenital anomalies of the kidney and urinary tract. Eur J Pediatr. 2016; 175:667–76.
Article37. Sarhan OM, Helaly AE, Al Otay A, Ghanbar MA, Nakshabandi Z. Isolated low grade prenatally detected unilateral hydronephrosis: do we need long term follow-up? Int Braz J Urol. 2018; 44:812–8.
Article38. Sanna-Cherchi S, Ravani P, Corbani V, Parodi S, Haupt R, Piaggio G, et al. Renal outcome in patients with congenital anomalies of the kidney and urinary tract. Kidney Int. 2009; 76:528–33.
Article39. Wuhl E, van Stralen KJ, Verrina E, Bjerre A, Wanner C, Heaf JG, et al. Timing and outcome of renal replacement therapy in patients with congenital malformations of the kidney and urinary tract. Clin J Am Soc Nephrol. 2013; 8:67–74.
Article40. Murugapoopathy V, Gupta IR. A primer on congenital anomalies of the kidneys and urinary tracts (CAKUT). Clin J Am Soc Nephrol. 2020; 15:723–31.
Article41. Pavlaki A, Printza N, Farmaki E, Stabouli S, Taparkou A, Sterpi M, et al. The role of urinary NGAL and serum cystatin C in assessing the severity of ureteropelvic junction obstruction in infants. Pediatr Nephrol. 2020; 35:163–70.
Article42. Gavrilovici C, Dusa CP, Iliescu Halitchi C, Lupu VV, Spoiala EL, Bogos RA, et al. The role of urinary NGAL in the management of primary vesicoureteral reflux in children. Int J Mol Sci. 2023; 24:7904.
Article43. Kazlauskas V, Bilius V, Jakutis V, Komiagiene R, Burnyte B, Verkauskas G. Urine biomarkers combined with ultrasound for the diagnosis of obstruction in pediatric hydronephrosis. Front Pediatr. 2022; 9:762417.
Article44. Karakus S, Oktar T, Kucukgergin C, Kalelioglu I, Seckin S, Atar A, et al. Urinary IP-10, MCP-1, NGAL, Cystatin-C, and KIM-1 levels in prenatally diagnosed unilateral hydronephrosis: the search for an ideal biomarker. Urology. 2016; 87:185–92.
Article45. Smail LC, Dhindsa K, Braga LH, Becker S, Sonnadara RR. Using deep learning algorithms to grade hydronephrosis severity: toward a clinical adjunct. Front Pediatr. 2020; 8:1.
Article46. Ostrowski DA, Logan JR, Antony M, Broms R, Weiss DA, Van Batavia J, et al. Automated Society of Fetal Urology (SFU) grading of hydronephrosis on ultrasound imaging using a convolutional neural network. J Pediatr Urol. 2023; 19:566.
Article47. Weaver JK, Logan J, Broms R, Antony M, Rickard M, Erdman L, et al. Deep learning of renal scans in children with antenatal hydronephrosis. J Pediatr Urol. 2023; 19:514.
Article48. Son MH, Park E, Yim HE, Nam YJ, Lee YS, Choi EK, et al. Maternal exposure to airborne particulate matter during pregnancy and lactation induces kidney injury in rat dams and their male offspring: the role of vitamin D in pregnancy and beyond. Kidney Res Clin Pract. 2024 Jan 2 [Epub]. https://doi.org/10.23876/j.krcp.23.106.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pediatric Neuropathic Bladder: A Clinical Study
- Screening of urinary tract infection in high-risk neonates
- Urinary Tract Infection and Its Diagnosis in Children
- Study of Urinary Lactic Dehydrogenase and Isoenzyme Patterns in Patients with Urinary Tract Infection
- A Clinical Study of Infants and Children with Urinary Tract Infection