Arch Hand Microsurg.
2024 Mar;29(1):53-59. 10.12790/ahm.23.0047.
The role of surgical timing in upper extremity free flap reconstruction following trauma: a 10-year single-center, single-surgeon experience
- Affiliations
-
- 1W Institute for Hand and Reconstructive Microsurgery, W General Hospital, Daegu, Korea
- KMID: 2553172
- DOI: http://doi.org/10.12790/ahm.23.0047
Abstract
- Purpose
Complex traumatic upper extremity injuries often require microvascular free tissue transfer for adequate soft tissue coverage or functional reconstruction. The need for rapid coverage is acknowledged, but the optimal timing for reconstruction remains a subject of debate.
Methods
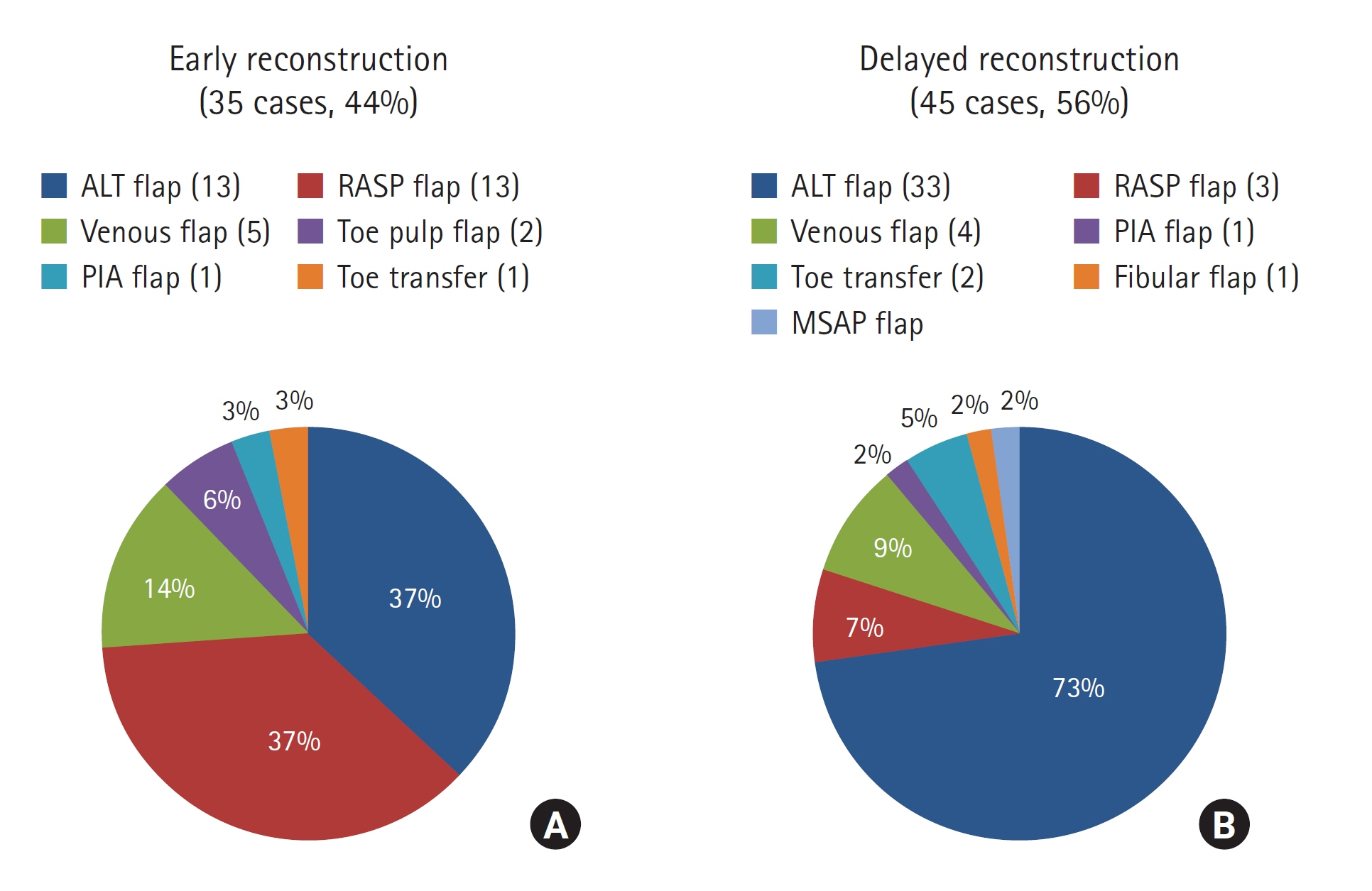
A retrospective review was conducted of patients who underwent free flap reconstruction for upper extremity injuries after trauma from March 2012 to August 2018 in South Korea at a facility specializing in extremity trauma. Surgical timing was categorized according to the classification of Godina into early (within 72 hours after injury) and delayed (from 72 hours to 3 months after injury) reconstruction. Patients’ demographic characteristics, methods of free tissue transfer, flap failure rates, postoperative infections, total hospital stays, and the number of operations required were analyzed.
Results
In total, 80 free tissue transfers were conducted on 76 patients. The demographics and characteristics of patients in the early and delayed reconstruction groups showed no significant differences. Early reconstruction was associated with a significantly lower infection rate, shorter average hospital stay, and a lower average number of operations, without showing a significant difference in the flap failure rate.
Conclusion
The results of this study indicate that early reconstruction within 72 hours after trauma significantly reduces infection rates, the length of hospital stays, and the number of required operations. This study underscores the importance of timely intervention in upper extremity free flap reconstruction for optimal patient outcomes.
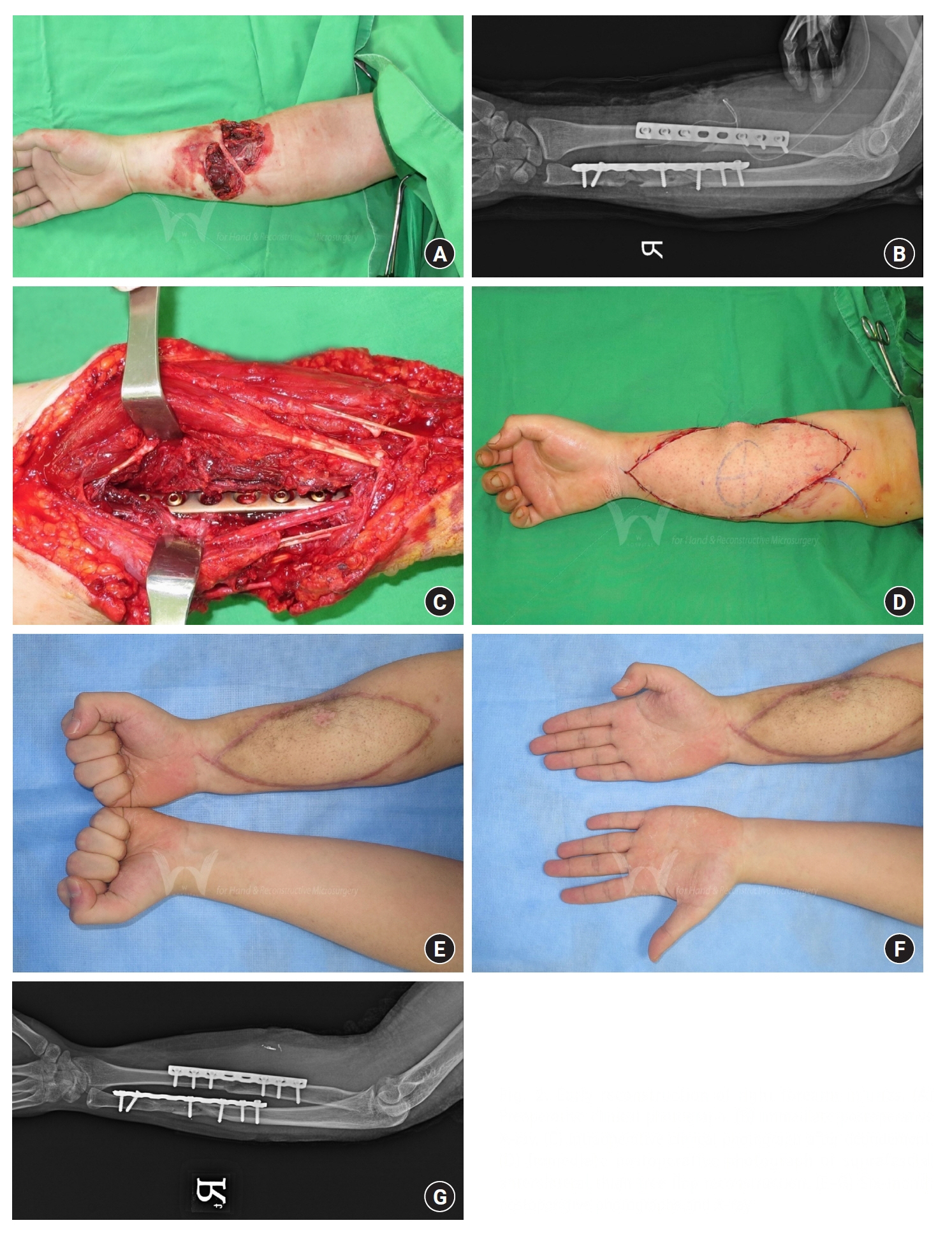
Figure
Reference
-
References
1. Hing DN, Buncke HJ, Alpert BS, Gordon L. Free flap coverage of the hand. Hand Clin. 1985; 1:741–58.
Article2. Chen HC, Buchman MT, Wei FC. Free flaps for soft tissue coverage in the hand and fingers. Hand Clin. 1999; 15:541–54.
Article3. Woo SJ, Park KH, Woo SH. Simultaneous or delayed free tissue transfer in combination with replantation surgery. Hand Clin. 2023 Sep 11 [Epub]. https://doi.org/10.1016/j.hcl.2023.08.013.
Article4. McCabe SJ, Breidenbach WC. The role of emergency free flaps for hand trauma. Hand Clin. 1999; 15:275–88.
Article5. Gupta A, Lakhiani C, Lim BH, et al. Free tissue transfer to the traumatized upper extremity: risk factors for postoperative complications in 282 cases. J Plast Reconstr Aesthet Surg. 2015; 68:1184–90.
Article6. Godina M. Early microsurgical reconstruction of complex trauma of the extremities. Plast Reconstr Surg. 1986; 78:285–92.
Article7. Georgescu AV, Ivan O. Emergency free flaps. Microsurgery. 2003; 23:206–16.
Article8. Derderian CA, Olivier WA, Baux G, Levine J, Gurtner GC. Microvascular free-tissue transfer for traumatic defects of the upper extremity: a 25-year experience. J Reconstr Microsurg. 2003; 19:455–62.
Article9. Kumar AR, Grewal NS, Chung TL, Bradley JP. Lessons from operation Iraqi freedom: successful subacute reconstruction of complex lower extremity battle injuries. Plast Reconstr Surg. 2009; 123:218–29.
Article10. Lee ZH, Stranix JT, Rifkin WJ, et al. Timing of microsurgical reconstruction in lower extremity trauma: an update of the Godina paradigm. Plast Reconstr Surg. 2019; 144:759–67.
Article11. Steiert AE, Gohritz A, Schreiber TC, Krettek C, Vogt PM. Delayed flap coverage of open extremity fractures after previous vacuum-assisted closure (VAC) therapy: worse or worth? J Plast Reconstr Aesthet Surg. 2009; 62:675–83.12. Harrison BL, Lakhiani C, Lee MR, Saint-Cyr M. Timing of traumatic upper extremity free flap reconstruction: a systematic review and progress report. Plast Reconstr Surg. 2013; 132:591–6.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Forecasting the flap: predictors for pediatric lower extremity trauma reconstruction
- Comparing Outcomes of Single Versus Double Venous Anastomosis in Free Flap Operation for Lower Extremity Defect Reconstruction: A Meta-Analysis
- Safety of a Single Venous Anastomosis in Anterolateral Thigh Free Flap for Extremity Reconstruction
- Division of a single free flap in multiple digit reconstruction
- Preoperative Identification of Perforator Using CT Angiography in Fibular Osteocutaneous Free Flap Head and Neck Reconstruction