Ann Rehabil Med.
2024 Feb;48(1):5-21. 10.5535/arm.23148.
Effectiveness of Community-Based Rehabilitation (CBR) Centers for Improving Physical Fitness for Community-Dwelling Older Adults: A Systematic Review and Meta-Analysis
- Affiliations
-
- 1Curtin Medical School, Curtin University, Perth, Australia
- 2Department of Rehabilitation Medicine, The Third Affiliated Hospital of Sun Yat-Sen University, Guangzhou, China
- 3Curtin School of Population Health, Faculty of Health Sciences, Curtin University, Perth, Australia
- 4Department of General Family Medicine, The First Affiliated Hospital of Sun Yat-Sen University, Guangzhou, China
- 5Institute for Health Research, The University of Notre Dame Australia, Perth, Australia
- 6School of Allied Health, The University of Western Australia, Perth, Australia
- KMID: 2553157
- DOI: http://doi.org/10.5535/arm.23148
Abstract
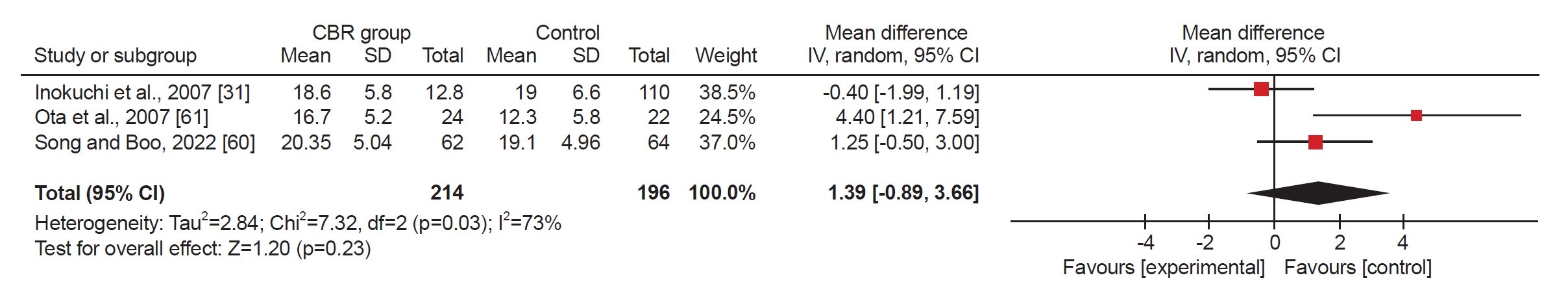
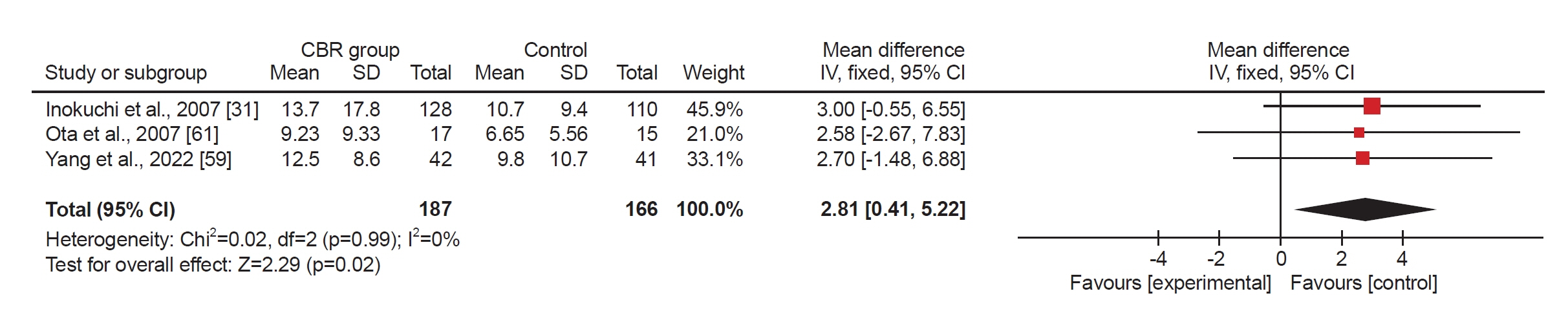
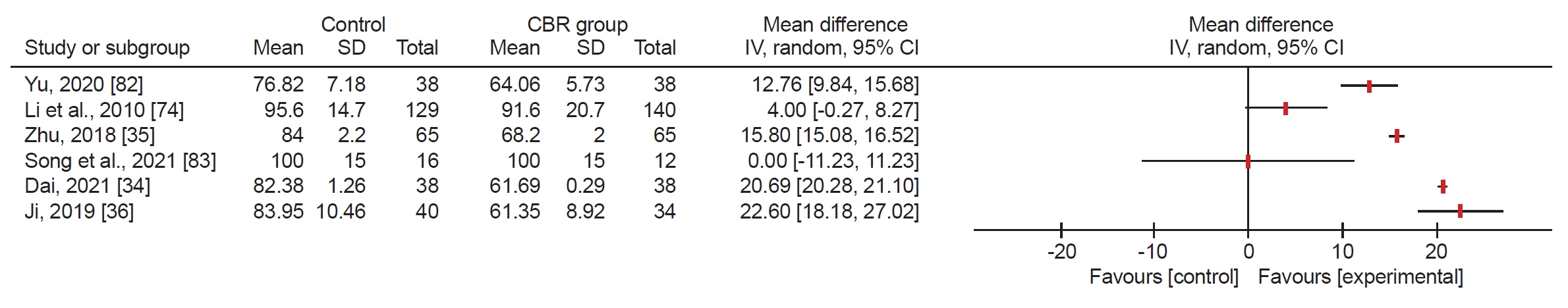
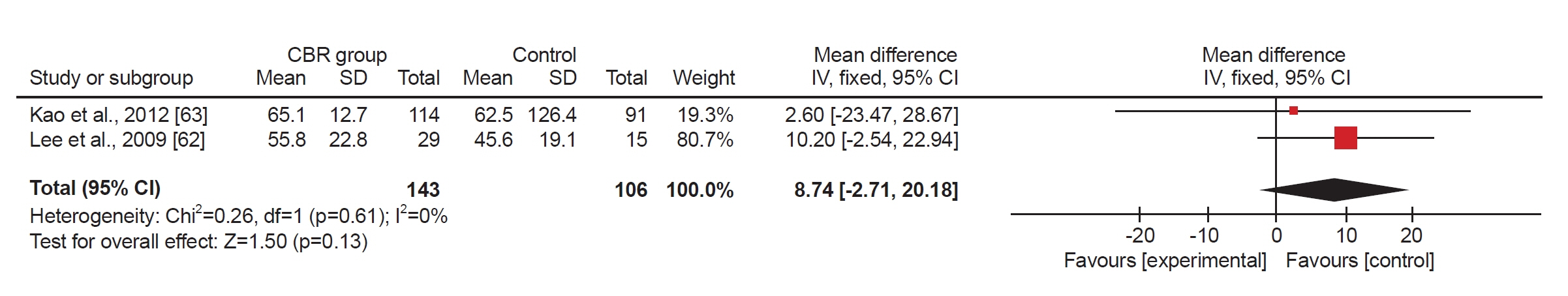
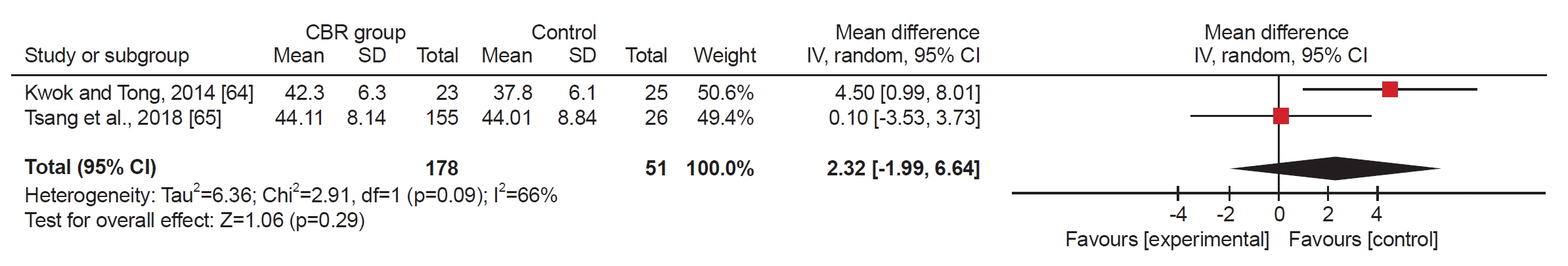
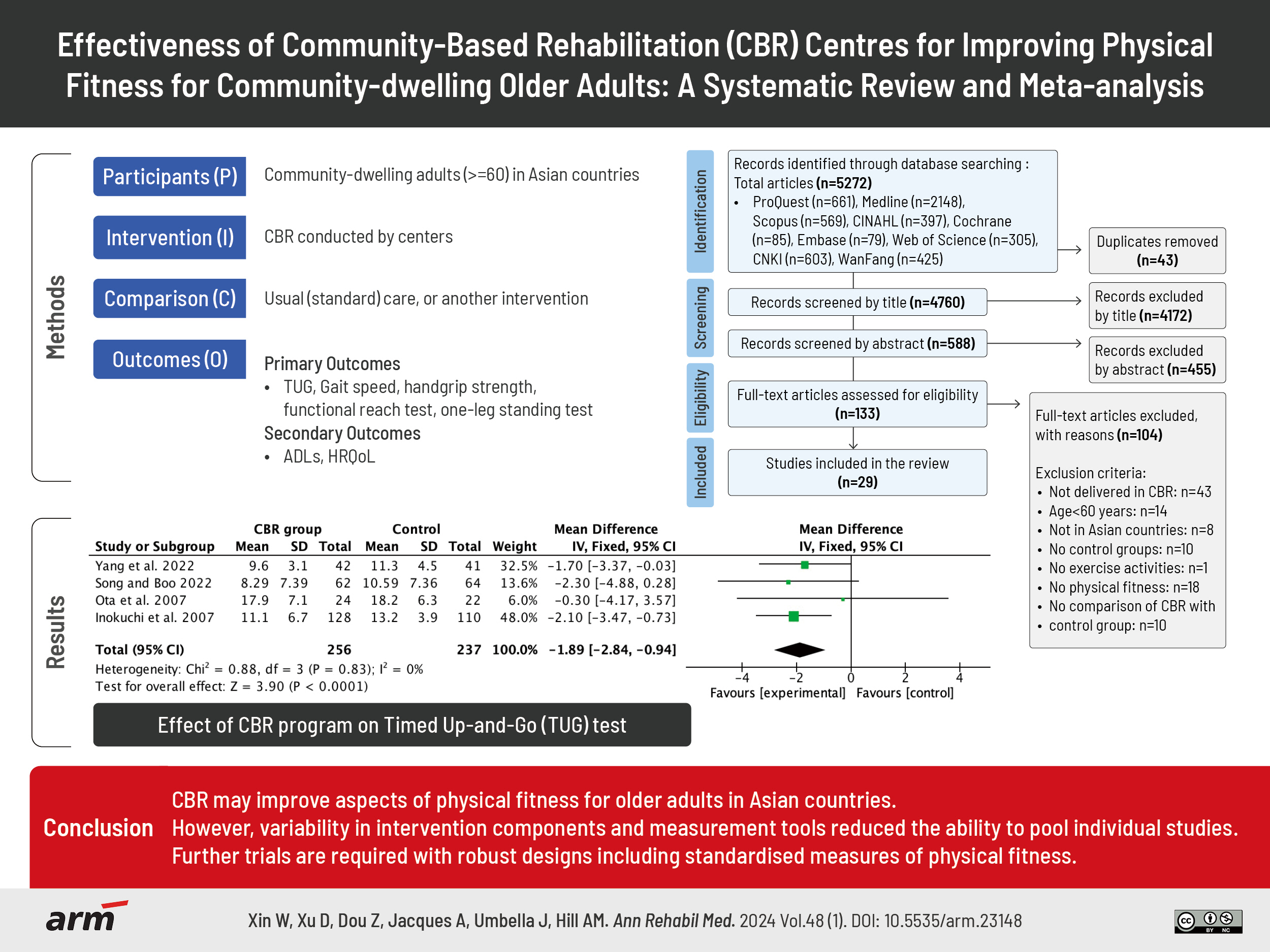
- To synthesise the best available evidence for the effectiveness of interventions delivered in community-based rehabilitation (CBR) centers on physical fitness, for community-dwelling older adults living in Asian countries. This study is a systematic review and meta-analysis. Seven English and two Chinese electronic databases were searched for randomised controlled trials (RCTs) and quasi-experimental studies that were conducted by centers providing CBR. Independent reviewers screened, quality-appraised and extracted data. The primary outcome was physical fitness measured by validated assessment tools, including the Timed Up and Go Test (TUG), gait speed, hand grip strength, Functional Reach Test (FRT), and one-leg standing test. Assessments of activity of daily living and quality of life using tools including the Barthel Index, Short Form (SF)-12, and SF-36 were secondary outcomes. After screening 5,272 studies, 29 studies were included (16 RCTs, 13 quasi-experimental studies) from four countries. Meta-analyses found that CBR programs significantly decreased TUG time (mean difference [MD], -1.89 seconds; 95% confidence interval [95% CI], -2.84 to -0.94; I2=0%; Z=3.90, p<0.0001), improved gait speed (MD, 0.10 m/s; 95% CI, 0.01–0.18; I2=0%; Z=2.26, p=0.02), and increased one-leg standing time (MD, 2.81 seconds; 95% CI, 0.41–5.22; I2=0%; Z=2.29, p=0.02). Handgrip strength and FRT showed no statistically significant improvement in the meta-analyses. CBR may improve aspects of physical fitness for older adults in Asian countries. However, variability in intervention components and measurement tools reduced the ability to pool individual studies. Further trials are required with robust designs including standardised measures of physical fitness.
Keyword
Figure
Reference
-
1. Partridge L, Deelen J, Slagboom PE. Facing up to the global challenges of ageing. Nature. 2018; 561:45–56.2. United Nations; Department of Economic and Social Affairs, Population Division. World population prospects 2019: highlights. United Nations; 2019. p. 1-46.3. Pan CW, Dirani M, Cheng CY, Wong TY, Saw SM. The age-specific prevalence of myopia in Asia: a meta-analysis. Optom Vis Sci. 2015; 92:258–66.4. Ye L, Luo J, Shia BC, Fang Y. Multidimensional health groups and healthcare utilization among elderly Chinese: based on the 2014 CLHLS dataset. Int J Environ Res Public Health. 2019; 16:3884.5. Zhou Y, Wushouer H, Vuillermin D, Ni B, Guan X, Shi L. Medical insurance and healthcare utilization among the middle-aged and elderly in China: evidence from the China health and retirement longitudinal study 2011, 2013 and 2015. BMC Health Serv Res. 2020; 20:654.6. Bloom DE, Chen S, Kuhn M, McGovern ME, Oxley L, Prettner K. The economic burden of chronic diseases: estimates and projections for China, Japan, and South Korea. J Econ Ageing. 2020; 17:100163.7. Sangeetha T, Chen Y, Sasidharan S. Oxidative stress and aging and medicinal plants as antiaging agents. J Complement Med Res. 2020; 11:1–5.8. Shmakova NN, Puzin SN, Zarariy NS, Abol AV. The characteristics of impaired functions and life limitations of disabled people due to coronary heart disease. J Popul Ther Clin Pharmacol. 2022; 29:e62–70.9. Hou C, Ping Z, Yang K, Chen S, Liu X, Li H, et al. Trends of activities of daily living disability situation and association with chronic conditions among elderly aged 80 years and over in China. J Nutr Health Aging. 2018; 22:439–45.10. World Health Organization (WHO). Healthy ageing and functional ability [Internet]. WHO; 2020 [cited 2023 Jan 2]. Available from: https://www.who.int/news-room/questions-and-answers/item/healthy-ageing-and-functional-ability.11. National Library of Medicine (NLM). Physical fitness [Internet]. NLM; 2022 [cited 2023 Jan 2]. Available from: https://www.ncbi.nlm.nih.gov/mesh/68010809.12. Vaish K, Patra S, Chhabra P. Functional disability among elderly: a community-based cross-sectional study. J Family Med Prim Care. 2020; 9:253–8.13. Oztürk A, Simşek TT, Yümin ET, Sertel M, Yümin M. The relationship between physical, functional capacity and quality of life (QoL) among elderly people with a chronic disease. Arch Gerontol Geriatr. 2011; 53:278–83.14. Cunningham C, O' Sullivan R, Caserotti P, Tully MA. Consequences of physical inactivity in older adults: a systematic review of reviews and meta-analyses. Scand J Med Sci Sports. 2020; 30:816–27.15. Sherrington C, Fairhall NJ, Wallbank GK, Tiedemann A, Michaleff ZA, Howard K, et al. Exercise for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2019; 1:CD012424.16. Valdés-Badilla PA, Gutiérrez-García C, Pérez-Gutiérrez M, Vargas-Vitoria R, López-Fuenzalida A. Effects of physical activity governmental programs on health status in independent older adults: a systematic review. J Aging Phys Act. 2019; 27:265–75.17. Papalia GF, Papalia R, Diaz Balzani LA, Torre G, Zampogna B, Vasta S, et al. The effects of physical exercise on balance and prevention of falls in older people: a systematic review and meta-analysis. J Clin Med. 2020; 9:2595.18. Liu CJ, Latham NK. Progressive resistance strength training for improving physical function in older adults. Cochrane Database Syst Rev. 2009; 2009:CD002759.19. Liu X, Shen PL, Tsai YS. Dance intervention effects on physical function in healthy older adults: a systematic review and meta-analysis. Aging Clin Exp Res. 2021; 33:253–63.20. Choo YT, Jiang Y, Hong J, Wang W. Effectiveness of Tai Chi on quality of life, depressive symptoms and physical function among community-dwelling older adults with chronic disease: a systematic review and meta-analysis. Int J Nurs Stud. 2020; 111:103737.21. Higashimoto Y, Ando M, Sano A, Saeki S, Nishikawa Y, Fukuda K, et al. Effect of pulmonary rehabilitation programs including lower limb endurance training on dyspnea in stable COPD: a systematic review and meta-analysis. Respir Investig. 2020; 58:355–66.22. Winsper C, Crawford-Docherty A, Weich S, Fenton SJ, Singh SP. How do recovery-oriented interventions contribute to personal mental health recovery? A systematic review and logic model. Clin Psychol Rev. 2020; 76:101815.23. Zacharias A, Green RA, Semciw AI, Kingsley MI, Pizzari T. Efficacy of rehabilitation programs for improving muscle strength in people with hip or knee osteoarthritis: a systematic review with meta-analysis. Osteoarthritis Cartilage. 2014; 22:1752–73.24. Izquierdo M, Merchant RA, Morley JE, Anker SD, Aprahamian I, Arai H, et al. International exercise recommendations in older adults (ICFSR): expert consensus guidelines. J Nutr Health Aging. 2021; 25:824–53.25. Fried TR, Bradley EH, Williams CS, Tinetti ME. Functional disability and health care expenditures for older persons. Arch Intern Med. 2001; 161:2602–7.26. Shi J, Liu X. Demands and determinants of community rehabilitation services for older adults. Chin J Rehabil Theory Pract. 2021; 27:334–40.27. World Health Organization (WHO). The global action plan on physical activity 2018 - 2030 [Internet]. WHO; 2019 [cited 2023 Jan 2]. Available from: https://www.who.int/initiatives/gappa/action-plan.28. World Health Organization (WHO). Community-based rehabilitation: CBR guidelines [Internet]. WHO; 2010 [cited 2023 Jan 2]. Available from: https://www.who.int/publications/i/item/9789241548052.29. Iemmi V, Gibson L, Blanchet K, Kumar KS, Rath S, Hartley S, et al. Community-based rehabilitation for people with disabilities in low- and middle-income countries: a systematic review. Campbell Syst Rev. 2015; 11:1–177.30. Kiblasan JIIA, Tukaki GB, Chakas RF. Community-based rehabilitation program in the municipality of Bauko, Mountain Province, Philippines. Med Leg Update. 2020; 20:255–60.31. Inokuchi S, Matsusaka N, Hayashi T, Shindo H. Feasibility and effectiveness of a nurse-led community exercise programme for prevention of falls among frail elderly people: a multi-centre controlled trial. J Rehabil Med. 2007; 39:479–85.32. Shrivastava S, Shrivastava P, Ramasamy J. Exploring the scope of community-based rehabilitation in ensuring the holistic development of differently-abled people. Afr Health Sci. 2015; 15:278–80.33. Vaughan K, Thapa A, Paudel R. Cost-effectiveness assessment of the Inspire2Care program in Ilam. Bang for Buck Consulting;2018. p. 3–36.34. Dai G. Effect analysis of community comprehensive rehabilitation nursing pathway in elderly patients with hemiplegia caused by cerebral infarction. Med Front. 2021; 11:2.35. Zhu Q. Effect of community comprehensive rehabilitation nursing pathway in elderly patients with hemiplegia caused by cerebral infarction. China Health Care Nutr. 2018; 28:2.36. Ji R. Effect of community comprehensive rehabilitation nursing pathway in elderly patients with hemiplegia caused by cerebral infarction. World's Latest Med Inf Dig. 2019; 19:2.37. Booth A, Clarke M, Dooley G, Ghersi D, Moher D, Petticrew M, et al. The nuts and bolts of PROSPERO: an international prospective register of systematic reviews. Syst Rev. 2012; 1:2.38. Xin W, Xu D, Dou Z, Jacques A, Umbella J, Hill AM. Effectiveness of community-based rehabilitation (CBR) centres for improving physical fitness for community-dwelling older adults: a systematic review protocol. BMJ Open. 2022; 12:e062992.39. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021; 10:89.40. Peters MDJ, Godfrey CM, McInerney P, Soares CB, Khalil H, Parker D. The Joanna Briggs Institute reviewers' manual 2015: methodology for JBI scoping reviews. The Joanna Briggs Institute;2015. p. 10–22.41. Bodenreider O. The Unified Medical Language System (UMLS): integrating biomedical terminology. Nucleic Acids Res. 2004; 32:D267–70.42. Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions. John Wiley & Sons;2019. p. 33–65.43. Pearson A, Wiechula R, Court A, Lockwood C. The JBI model of evidence-based healthcare. Int J Evid Based Healthc. 2005; 3:207–15.44. Podsiadlo D, Richardson S. The timed "Up & Go": a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991; 39:142–8.45. Studenski S, Perera S, Patel K, Rosano C, Faulkner K, Inzitari M, et al. Gait speed and survival in older adults. JAMA. 2011; 305:50–8.46. Wang YC, Bohannon RW, Li X, Sindhu B, Kapellusch J. Hand-grip strength: normative reference values and equations for individuals 18 to 85 years of age residing in the United States. J Orthop Sports Phys Ther. 2018; 48:685–93.47. Jonsson E, Henriksson M, Hirschfeld H. Does the Functional Reach Test reflect stability limits in elderly people? J Rehabil Med. 2003; 35:26–30.48. Springer BA, Marin R, Cyhan T, Roberts H, Gill NW. Normative values for the unipedal stance test with eyes open and closed. J Geriatr Phys Ther. 2007; 30:8–15.49. Katz S. Assessing self-maintenance: activities of daily living, mobility, and instrumental activities of daily living. J Am Geriatr Soc. 1983; 31:721–7.50. National Library of Medicine (NLM). Activities of daily living [Internet]. NLM; 2022 [cited 2023 Jan 2]. Available from: https://www.ncbi.nlm.nih.gov/mesh/?term=Activities+of+Daily+Living.51. Shah S, Vanclay F, Cooper B. Improving the sensitivity of the Barthel Index for stroke rehabilitation. J Clin Epidemiol. 1989; 42:703–9.52. Burdine JN, Felix MR, Abel AL, Wiltraut CJ, Musselman YJ. The SF-12 as a population health measure: an exploratory examination of potential for application. Health Serv Res. 2000; 35:885–904.53. Ware JE Jr. SF-36 health survey update. Spine (Phila Pa 1976). 2000; 25:3130–9.54. Deeks JJ, Higgins JPT. Statistical algorithms in review manager 5. Statistical Methods Group of the Cochrane Collaboration. The Cochrane Collaboration;2010. p. 1–11.55. Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005; 5:13.56. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003; 327:557–60.57. McMaster University. GRADEpro GDT. GRADEpro guideline development tool [Internet]. McMaster University; 2015 [cited 2023 Jan 21]. Available from: https://cebgrade.mcmaster.ca/gradepro.html.58. Schünemann HJ, Mustafa RA, Brozek J, Steingart KR, Leeflang M, Murad MH, et al. GRADE guidelines: 21 part 2. Test accuracy: inconsistency, imprecision, publication bias, and other domains for rating the certainty of evidence and presenting it in evidence profiles and summary of findings tables. J Clin Epidemiol. 2020; 122:142–52.59. Yang SH, Chang QX, Liang CC, Chen JC. The effects of using a low-cost and easily accessible exercise toolkit incorporated to the governmental health program on community-dwelling older adults: a quasi-experimental study. Int J Environ Res Public Health. 2022; 19:9614.60. Song MS, Boo S. Effects of a nurse-led multicomponent intervention for frail older adults living alone in a community: a quasi-experimental study. BMC Nurs. 2022; 21:20.61. Ota A, Yasuda N, Horikawa S, Fujimura T, Ohara H. Differential effects of power rehabilitation on physical performance and higher-level functional capacity among community-dwelling older adults with a slight degree of frailty. J Epidemiol. 2007; 17:61–7.62. Lee HJ, Park HJ, Chae Y, Kim SY, Kim SN, Kim ST, et al. Tai Chi Qigong for the quality of life of patients with knee osteoarthritis: a pilot, randomized, waiting list controlled trial. Clin Rehabil. 2009; 23:504–11.63. Kao MJ, Wu MP, Tsai MW, Chang WW, Wu SF. The effectiveness of a self-management program on quality of life for knee osteoarthritis (OA) patients. Arch Gerontol Geriatr. 2012; 54:317–24.64. Kwok TM, Tong CY. Effects on centre-based training and home-based training on physical function, quality of life and fall incidence in community dwelling older adults. Physiother Theory Pract. 2014; 30:243–8.65. Tsang EW, Kwok H, Chan AKY, Choo KL, Chan KS, Lau KS, et al. Outcomes of community-based and home-based pulmonary rehabilitation for pneumoconiosis patients: a retrospective study. BMC Pulm Med. 2018; 18:133.66. Hasegawa M, Yamazaki S, Kimura M, Nakano K, Yasumura S. Community-based exercise program reduces chronic knee pain in elderly Japanese women at high risk of requiring long-term care: a non-randomized controlled trial. Geriatr Gerontol Int. 2013; 13:167–74.67. Harel-Katz H, Adar T, Milman U, Carmeli E. Examining the feasibility and effectiveness of a culturally adapted participation-focused stroke self-management program in a day-rehabilitation setting: a randomized pilot study. Top Stroke Rehabil. 2020; 27:577–89.68. Gong J, Chen X, Li S. Efficacy of a community-based physical activity program KM2H2 for stroke and heart attack prevention among senior hypertensive patients: a cluster randomized controlled phase-II trial. PLoS One. 2015; 10:e0139442.69. Kamada M, Kitayuguchi J, Abe T, Taguri M, Inoue S, Ishikawa Y, et al. Community-wide promotion of physical activity in middle-aged and older Japanese: a 3-year evaluation of a cluster randomized trial. Int J Behav Nutr Phys Act. 2015; 12:82.70. Yoo IG, Yoo WG. Effects of a multidisciplinary supervised exercise program on motor performance and quality of life in community-dwelling chronic stroke survivors in Korean. Southeast Asian J Trop Med Public Health. 2011; 42:436–43.71. Wang L, Chen CM, Liao WC, Hsiao CY. Evaluating a community-based stroke nursing education and rehabilitation programme for patients with mild stroke. Int J Nurs Pract. 2013; 19:249–56.72. Sun FC, Li HC, Wang HH. The effect of group music therapy with physical activities to prevent frailty in older people living in the community. Int J Environ Res Public Health. 2021; 18:8791.73. Ru X, Dai H, Jiang B, Li N, Zhao X, Hong Z, et al. Community-based rehabilitation to improve stroke survivors' rehabilitation participation and functional recovery. Am J Phys Med Rehabil. 2017; 96:e123–9.74. Li CM, Chen CY, Li CY, Wang WD, Wu SC. The effectiveness of a comprehensive geriatric assessment intervention program for frailty in community-dwelling older people: a randomized, controlled trial. Arch Gerontol Geriatr. 2010; 50 Suppl 1:S39–42.75. Zhang L, Zhang L, Wang J, Ding F, Zhang S. Community health service center-based cardiac rehabilitation in patients with coronary heart disease: a prospective study. BMC Health Serv Res. 2017; 17:128.76. Dun Y, Hu P, Ripley-Gonzalez JW, Zhou N, Li H, Zhang W, et al. Effectiveness of a multicomponent exercise program to reverse pre-frailty in community-dwelling Chinese older adults: a randomised controlled trial. Age Ageing. 2022; 51:afac026.77. Liang CK, Lee WJ, Hwang AC, Lin CS, Chou MY, Peng LN, et al. Efficacy of multidomain intervention against physio-cognitive decline syndrome: a cluster-randomized trial. Arch Gerontol Geriatr. 2021; 95:104392.78. Lee JG, Kim WJ, Kyoung KJ. Effects of resistance exercise program on pain, stress, range of motion, and body composition of older adults: a randomized controlled trial. Altern Ther Health Med. 2022; 28:95–103.79. Tong C, Du Y, Liu X. Curative effect evaluation of community health management to Taiyuan elderly health cadres with stable chronic obstructive pulmonary disease. Chin J Geriatr Res. 2016; 3:38–43.80. Cui K, Zhang R. Comprehensive management mode intervention in elderly patients with moderate/severe chronic obstructive pulmonary disease at stable stage. J Public Health Prev Med. 2020; 3:126–9.81. Cao L. Application of community rehabilitation nursing pathway in the nursing of elderly patients with hemiplegia caused by cerebral infarction. Health Vis. 2020; 19:120.82. Yu E. Observation on the effect of community rehabilitation nursing pathway in elderly patients with hemiplegia caused by cerebral infarction. Sci Health. 2020; 6:146.83. Song CY, Lin PS, Hung PL, ADLers Occupational Therapy Clinic. Effects of community-based physical-cognitive training, health education, and reablement among rural community-dwelling older adults with mobility deficits. Int J Environ Res Public Health. 2021; 18:9374.84. Li L, Dai JX, Xu L, Huang ZX, Pan Q, Zhang X, et al. The effect of a rehabilitation nursing intervention model on improving the comprehensive health status of patients with hand burns. Burns. 2017; 43:877–85.85. Yu J, Hu Y, Wu Y, Chen W, Zhu Y, Cui X, et al. The effects of community-based rehabilitation on stroke patients in China: a single-blind, randomized controlled multicentre trial. Clin Rehabil. 2009; 23:408–17.86. Wang L, Chen H, Lu H, Wang Y, Liu C, Dong X, et al. The effect of transtheoretical model-lead intervention for knee osteoarthritis in older adults: a cluster randomized trial. Arthritis Res Ther. 2020; 22:134.87. Chen Y, Li X, Jing G, Pan B, Ge L, Bing Z, et al. Health education interventions for older adults with hypertension: a systematic review and meta-analysis. Public Health Nurs. 2020; 37:461–9.88. Zhu LY, Chan R, Kwok T, Cheng KC, Ha A, Woo J. Effects of exercise and nutrition supplementation in community-dwelling older Chinese people with sarcopenia: a randomized controlled trial. Age Ageing. 2019; 48:220–8.89. Littlewood C. The RCT means nothing to me! Man Ther. 2011; 16:614–7.90. Wright AA, Cook CE, Baxter GD, Dockerty JD, Abbott JH. A comparison of 3 methodological approaches to defining major clinically important improvement of 4 performance measures in patients with hip osteoarthritis. J Orthop Sports Phys Ther. 2011; 41:319–27.91. Krumpoch S, Lindemann U, Rappl A, Becker C, Sieber CC, Freiberger E. The effect of different test protocols and walking distances on gait speed in older persons. Aging Clin Exp Res. 2021; 33:141–6.92. Bohannon RW. Minimal clinically important difference for grip strength: a systematic review. J Phys Ther Sci. 2019; 31:75–8.93. Bohannon RW. Grip strength: an indispensable biomarker for older adults. Clin Interv Aging. 2019; 14:1681–91.94. McGrath RP, Kraemer WJ, Snih SA, Peterson MD. Handgrip strength and health in aging adults. Sports Med. 2018; 48:1993–2000.95. Bobos P, Nazari G, Lu Z, MacDermid JC. Measurement properties of the hand grip strength assessment: a systematic review with meta-analysis. Arch Phys Med Rehabil. 2020; 101:553–65.96. Bogle Thorbahn LD, Newton RA. Use of the Berg Balance Test to predict falls in elderly persons. Phys Ther. 1996; 76:576–83.97. Dohrn IM, Hagströmer M, Hellénius ML, Ståhle A. Short- and long-term effects of balance training on physical activity in older adults with osteoporosis: a randomized controlled trial. J Geriatr Phys Ther. 2017; 40:102–11.98. Farrance C, Tsofliou F, Clark C. Adherence to community based group exercise interventions for older people: a mixed-methods systematic review. Prev Med. 2016; 87:155–66.99. Ntoumanis N, Thøgersen-Ntoumani C, Quested E, Hancox J. The effects of training group exercise class instructors to adopt a motivationally adaptive communication style. Scand J Med Sci Sports. 2017; 27:1026–34.100. Unnanuntana A, Jarusriwanna A, Nepal S. Validity and responsiveness of Barthel Index for measuring functional recovery after hemiarthroplasty for femoral neck fracture. Arch Orthop Trauma Surg. 2018; 138:1671–7.101. Elsawy B, Higgins KE. Physical activity guidelines for older adults. Am Fam Physician. 2010; 81:55–9.102. Kruschke C, Butcher HK. Evidence-based practice guideline: fall prevention for older adults. J Gerontol Nurs. 2017; 43:15–21.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The effectiveness of protein supplementation combined with resistance exercise programs among community-dwelling older adults with sarcopenia: a systematic review and meta-analysis
- Effects of a Fall Prevention Program on Physical Fitness, Fall Efficacy and Fall Prevention Behavior among Community-dwelling Older Adults
- Association between Dynapenia and Multimorbidity in Community-Dwelling Older Adults: A Systematic Review
- Prevalence of Depression and its Risk Factors among Aged at Social Service Centers in One Urban Community
- Effectiveness of community-based interventions for older adults living alone: a systematic review and meta-analysis