J Korean Neurosurg Soc.
2024 Mar;67(2):217-226. 10.3340/jkns.2023.0166.
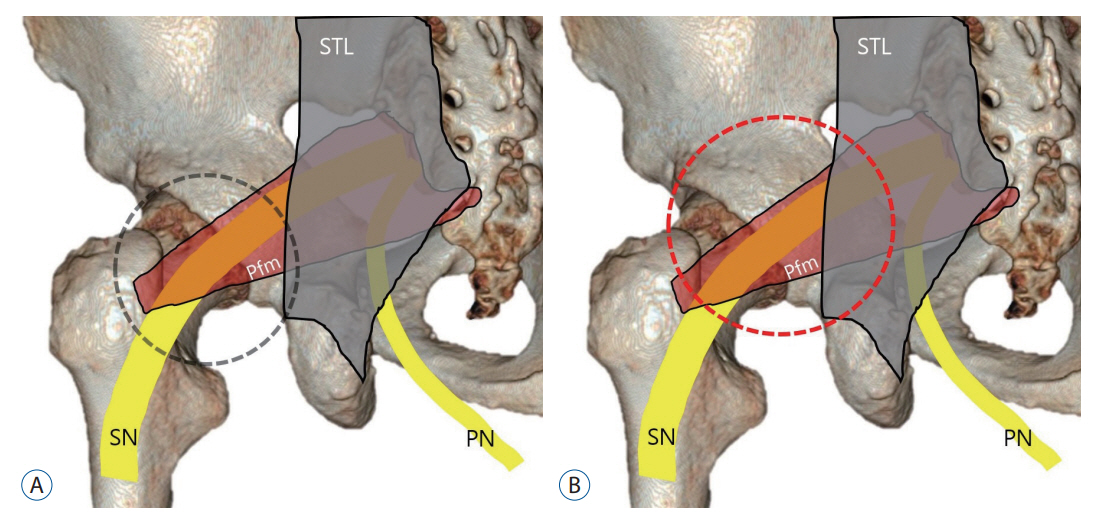
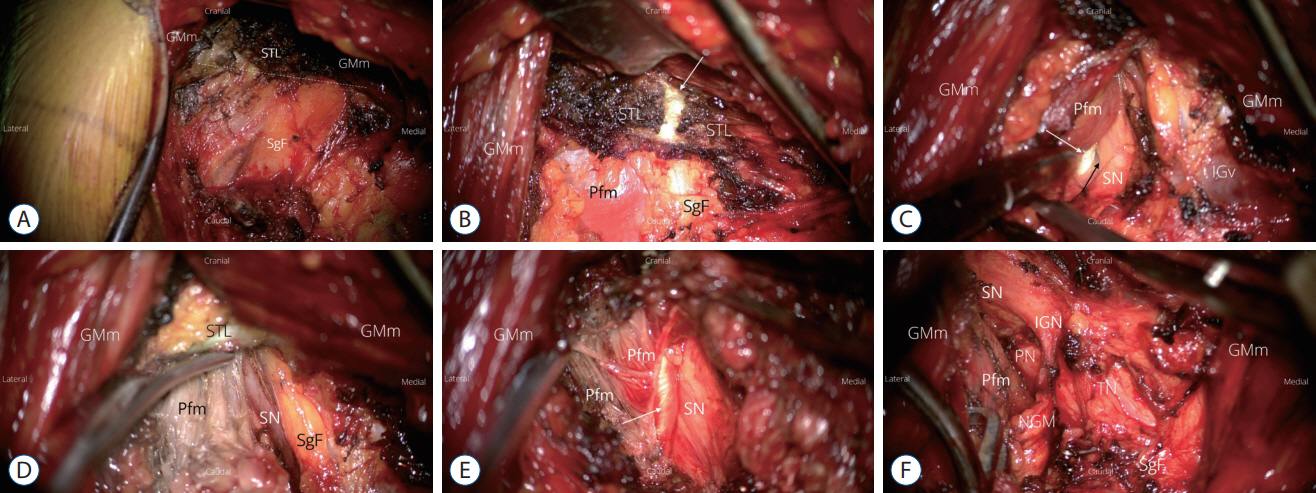
Importance of Sacrotuberous Ligament in Transgluteal Approach for Sciatic Nerve Entrapment in the Greater Sciatic Notch (Piriformis Syndrome)
- Affiliations
-
- 1Department of Neurosurgery, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Catholic Neuroscience Institute, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2553128
- DOI: http://doi.org/10.3340/jkns.2023.0166
Abstract
Objective
: The efficacy of sciatic nerve decompression via transgluteal approach for entrapment of the sciatic nerve at the greater sciatic notch, called piriformis syndrome, and factors affecting the surgical outcome were analyzed.
Methods
: The outcome of pain reduction was analyzed in 81 patients with sciatic nerve entrapment who underwent decompression through a transgluteal approach. The patients were followed up for at least 6 months. The degree of pain reduction was analyzed using a numerical rating scale-11 (NRS-11) score and percent pain relief before and after last follow-up following surgery. Success was defined by at least 50% reduction in pain measured via NRS-11. To assess the degree of subjective satisfaction, a 10-point Likert scale was used. In addition, demographic characteristics, anatomical variations, and variations in surgical technique involving sacrotuberous ligamentectomy were analyzed as factors that affect the surgical outcome.
Results
: At a follow-up of 17.5±12.5 months, sciatic nerve decompression was successful in 50 of 81 patients (61.7%), and the pain relief rate was 43.9±34.17. Subjective improvement based on a 10-point Likert scale was 4.90±3.43. Among the factors that affect the surgical outcome, only additional division of the sacrotuberous ligament during piriformis muscle resection played a significant role. The success rate was higher in the scarotuberous ligementectomy group (79.4%) than in the non-resection group (42.6%), resulting in statistically significant difference based on average NRS-11 score, percent pain relief, and subjective improvement (p<0.05, independent t-test).
Conclusion
: Sciatic nerve decompression is effective in pain relief in chronic sciatica due to sciatic nerve entrapment at the greater sciatic notch. Its effect was further enhanced by circumferential dissection of the sciatic nerve based on the compartment formed by the piriformis muscle and the sacrotuberous ligament in the greater sciatic notch.
Figure
Reference
-
References
1. Aldabe D, Hammer N, Flack NAMS, Woodley SJ. A systematic review of the morphology and function of the sacrotuberous ligament. Clin Anat. 32:396–407. 2019.2. Bartret AL, Beaulieu CF, Lutz AM. Is it painful to be different? Sciatic nerve anatomical variants on MRI and their relationship to piriformis syndrome. Eur Radiol. 28:4681–4686. 2018.3. Beaton LE, Anson BJ. The relation of the sciatic nerve and of its subdivisions to the piriformis muscle. Anat Rec. 70:1–5. 1937.4. Benzon HT, Katz JA, Benzon HA, Iqbal MS. Piriformis syndrome: anatomic considerations, a new injection technique, and a review of the literature. Anesthesiology. 98:1442–1448. 2003.5. Cass SP. Piriformis syndrome: a cause of nondiscogenic sciatica. Curr Sports Med Rep. 14:41–44. 2015.6. Chan CW, Peng P. Failed back surgery syndrome. Pain Med. 12:577–606. 2011.7. Durrani Z, Winnie AP. Piriformis muscle syndrome: an underdiagnosed cause of sciatica. J Pain Symptom Manage. 6:384–379. 1991.8. England JD. Entrapment neuropathies. Curr Opin Neurol. 12:597–602. 1999.9. Filler AG, Haynes J, Jordan SE, Prager J, Villablanca JP, Farahani K, et al. Sciatica of nondisc origin and piriformis syndrome: diagnosis by magnetic resonance neurography and interventional magnetic resonance imaging with outcome study of resulting treatment. J Neurosurg Spine. 2:99–115. 2005.10. Fishman LM, Schaefer MP. The piriformis syndrome is underdiagnosed. Muscle Nerve. 28:646–649. 2003.11. Fritz J, Fritz B, Dellon AL. Sacrotuberous ligament healing following surgical division during transgluteal pudendal nerve decompression: a 3-tesla MR neurography study. PLoS One. 11:e0165239. 2016.12. Furtmüller GJ, McKenna CA, Ebmer J, Dellon AL. Pudendal nerve 3-dimensional illustration gives insight into surgical approaches. Ann Plast Surg. 73:670–678. 2014.13. Hallin RP. Sciatic pain and the piriformis muscle. Postgrad Med. 74:69–72. 1983.14. Hernando MF, Cerezal L, Pérez-Carro L, Abascal F, Canga A. Deep gluteal syndrome: anatomy, imaging, and management of sciatic nerve entrapments in the subgluteal space. Skeletal Radiol. 44:919–934. 2015.15. Hwang Y, Son BC. Sciatic nerve entrapment (deep gluteal syndrome) as a cause of failed back surgery syndrome: a case report. The Nerve. 6:114–119. 2020.16. Kay J, de Sa D, Morrison L, Fejtek E, Simunovic N, Martin HD, et al. Surgical management of deep gluteal syndrome causing sciatic nerve entrapment: a systematic review. Arthroscopy. 33:2263–2278.e1. 2017.17. Knudsen JS, Mei-Dan O, Brick MJ. Piriformis syndrome and endoscopic sciatic neurolysis. Sports Med Arthrosc Rev. 24:e1–e7. 2016.18. Kobbe P, Zelle BA, Gruen GS. Case report : recurrent piriformis syndrome after surgical release. Clin Orthop Relat Res. 466:1745–1748. 2008.19. Martin HD, Shears SA, Johnson JC, Smathers AM, Palmer IJ. The endoscopic treatment of sciatic nerve entrapment/deep gluteal syndrome. Arthroscopy. 27:172–181. 2011.20. Moretti VM, Post ZD. Surgical approaches for total hip arthroplasty. Indian J Orthop. 51:368–370. 2017.21. Natsis K, Totlis T, Konstantinidis GA, Paraskevas G, Piagkou M, Koebke J. Anatomical variations between the sciatic nerve and the piriformis muscle: a contribution to surgical anatomy in piriformis syndrome. Surg Radiol Anat. 36:273–280. 2014.22. Papadopoulos EC, Khan SN. Piriformis syndrome and low back pain: a new classification and review of the literature. Orthop Clin North Am. 35:64–71. 2004.23. Park JW, Lee YK, Lee YJ, Shin S, Kang Y, Koo KH. Deep gluteal syndrome as a cause of posterior hip pain and sciatica-like pain. Bone Joint J. 102-B:556–567. 2020.24. Pećina M. Contribution to the etiological explanation of the piriformis syndrome. Acta Anat (Basel). 105:181–187. 1979.25. Probst D, Stout A, Hunt D. Piriformis syndrome: a narrative review of the anatomy, diagnosis, and treatment. PM R. 11 Suppl 1:S54–S63. 2019.26. Robert R, Labat JJ, Riant T, Khalfallah M, Hamel O. Neurosurgical treatment of perineal neuralgias. Adv Tech Stand Neurosurg. 32:41–59. 2007.27. Robinson DR. Pyriformis syndrome in relation to sciatic pain. Am J Surg. 73:355–358. 1947.28. Smoll NR. Variations of the piriformis and sciatic nerve with clinical consequence: a review. Clin Anat. 23:8–17. 2010.29. Spinner RJ, Thomas NM, Kline DG. Failure of surgical decompression for a presumed case of piriformis syndrome. Case report. J Neurosurg. 94:652–654. 2001.30. Son BC. Sciatic nerve entrapment in deep gluteal space (piriformis syndrome) as a cause of failed back surgery syndrome: a case report. Int J Pain. 13:90–98. 2022.31. Son BC. Decompression of pudendal nerve in chronic pudendal neuralgia: a case report. Int J Pain. 11:61–68. 2020.32. Son BC, Lee C. Decompression of inferior rectal nerve in refractory perianal pain caused by pudendal nerve entrapment: a case report. Int J Pain. 12:24–30. 2021.33. Son BC, Lee C. Piriformis syndrome (sciatic nerve entrapment) associated with type C sciatic nerve variation: a report of two cases and literature review. Korean J Neurotrauma. 18:434–443. 2022.34. Son BC, Lee C. The transgluteal approach for decompression of sciatic nerve entrapment (piriformis syndrome) with intraoperative neurophysiology: a technical note. The Nerve. 8:59–69. 2022.35. Standring S. Gray’s anatomy the anatomical basis of clinical practice. 41st ed. Edinburg: Elsevier;2016. p. 1354–1359.36. Voos JE, Rudzki JR, Shindle MK, Martin H, Kelly BT. Arthroscopic anatomy and surgical techniques for peritrochanteric space disorders in the hip. Arthroscopy. 23:1246.e1–e5. 2007.37. Yeoman W. The relation of arthritis of the sacro-iliac joint to sciatica, with an analysis of 100 cases. Lancet. 2:1119–1122. 1928.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Transgluteal Approach for Decompression of Sciatic Nerve Entrapment (Piriformis Syndrome) with Intraoperative Neurophysiology: A Technical Note
- Piriformis Syndrome (Sciatic Nerve Entrapment) Associated With Type C Sciatic Nerve Variation: A Report of Two Cases and Literature Review
- Piriformis Syndrome: A Case Report
- Piriformis syndrome: a case report
- A Case Report of the Piriformis Syndrome Treated by Caudal Steroid and Local Anesthetic