Ann Surg Treat Res.
2024 Feb;106(2):68-77. 10.4174/astr.2024.106.2.68.
Safety of nighttime elective hepatectomy for hepatocellular carcinoma patients: a retrospective study
- Affiliations
-
- 1Division of Liver Surgery, Department of General Surgery, West China Hospital, Sichuan University, Chengdu, China
- KMID: 2552387
- DOI: http://doi.org/10.4174/astr.2024.106.2.68
Abstract
- Purpose
This study aimed to investigate whether nighttime elective surgery influenced the short-term outcomes and prognosis of hepatocellular carcinoma (HCC) patients.
Methods
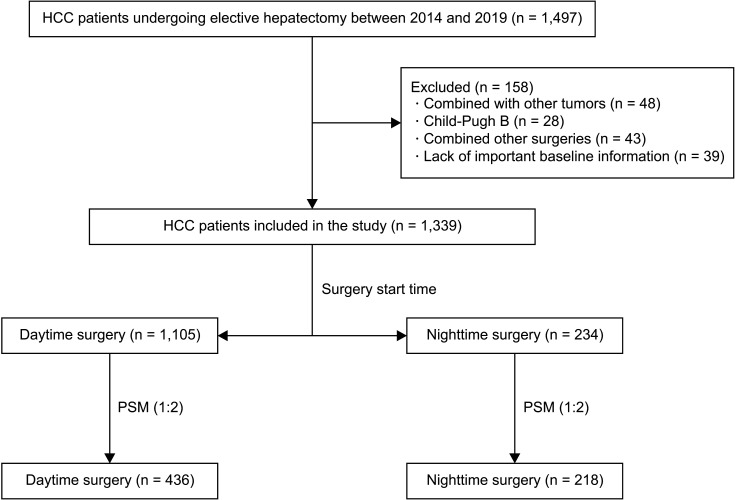
The 1,339 HCC patients who underwent hepatectomy were divided into the daytime surgery group (8 a.m.–6 p.m., n = 1,105) and the nighttime surgery group (after 6 p.m., n = 234) based on the start time of surgery. The 1:2 propensity score matching (PSM) analysis was used to control confounding factors. The short-term outcomes of HCC patients in the 2 groups were compared before and after PSM. Factors associated with major complications (Clavien-Dindo grade, ≥III) and textbook oncologic outcomes (TOO) were separately identified by multivariable logistic regression based on variables screened via least absolute shrinkage and selection operator (LASSO). The Kaplan-Meier method was used to analyze overall survival (OS) and recurrence-free survival (RFS).
Results
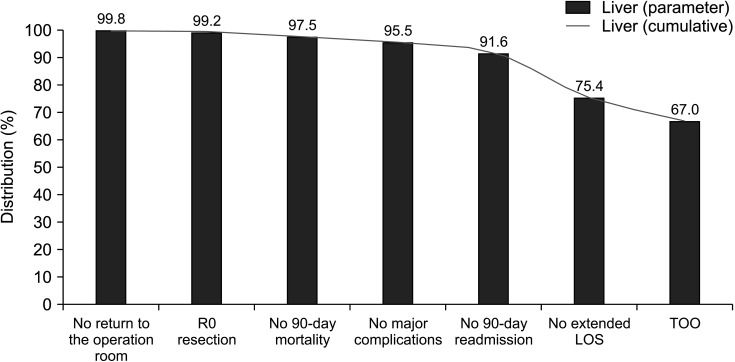
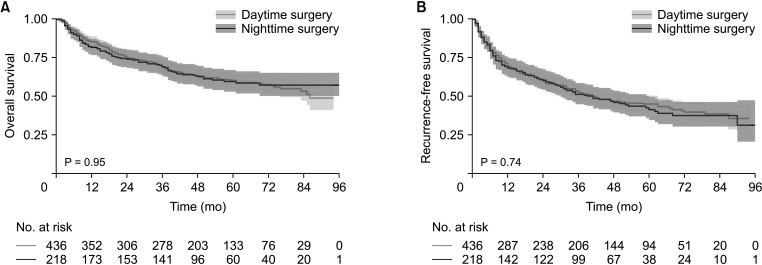
TOO was achieved after surgery in 897 HCC patients. HCC patients in the nighttime surgery group had a higher body mass index (P = 0.010). After 1:2 PSM, the baseline characteristics of patients between the 2 groups were similar. Short-term outcomes in HCC patients were comparable both before and after PSM (all Ps > 0.05), as were TOO in the 2 groups before (P = 0.673) and after PSM (P = 0.333). In our LASSO-logistic regression, nighttime surgery was not an independent factor associated with major complications or TOO. Both groups also had similar OS (P = 0.950) and RFS (P = 0.740) after PSM.
Conclusion
Our study revealed the safety of nighttime elective hepatectomy for HCC patients.
Keyword
Figure
Reference
-
1. Cortegiani A, Ippolito M, Misseri G, Helviz Y, Ingoglia G, Bonanno G, et al. Association between night/after-hours surgery and mortality: a systematic review and meta-analysis. Br J Anaesth. 2020; 124:623–637. PMID: 32147102.2. Cortegiani A, Gregoretti C, Neto AS, Hemmes SN, Ball L, Canet J, et al. Association between night-time surgery and occurrence of intraoperative adverse events and postoperative pulmonary complications. Br J Anaesth. 2019; 122:361–369. PMID: 30770054.3. Janhofer DE, Lakhiani C, Song DH. Addressing surgeon fatigue: current understanding and strategies for mitigation. Plast Reconstr Surg. 2019; 144:693e–699e. PMID: 31461028.4. Kelz RR, Freeman KM, Hosokawa PW, Asch DA, Spitz FR, Moskowitz M, et al. Time of day is associated with postoperative morbidity: an analysis of the national surgical quality improvement program data. Ann Surg. 2008; 247:544–552. PMID: 18376202.5. Lu Q, Li QS, Zhang W, Liu K, Li T, Yu JW, et al. Operation start time and long-term outcome of hepatocellular carcinoma after curative hepatic resection. Ann Surg Treat Res. 2020; 99:1–7. PMID: 32676476.6. Sessler DI, Kurz A, Saager L, Dalton JE. Operation timing and 30-day mortality after elective general surgery. Anesth Analg. 2011; 113:1423–1428. PMID: 21965365.7. Institute of Medicine (US) Committee on Quality of Health Care in America. Kohn LT, Corrigan JM, Donaldson MS, editors. To err is human: building a safer health system. National Academies Press (US);2000.8. Gawande AA, Zinner MJ, Studdert DM, Brennan TA. Analysis of errors reported by surgeons at three teaching hospitals. Surgery. 2003; 133:614–621. PMID: 12796727.9. Turrentine FE, Wang H, Young JS, Calland JF. What is the safety of nonemergent operative procedures performed at night? A study of 10,426 operations at an academic tertiary care hospital using the American College of Surgeons national surgical quality program improvement database. J Trauma. 2010; 69:313–319. PMID: 20699739.10. Althoff FC, Wachtendorf LJ, Rostin P, Santer P, Schaefer MS, Xu X, et al. Effects of night surgery on postoperative mortality and morbidity: a multicentre cohort study. BMJ Qual Saf. 2021; 30:678–688.11. Koltka AK, İlhan M, Ali A, Gök AF, Sivrikoz N, Yanar TH, et al. Is nighttime laparoscopic general surgery under general anesthesia safe? Ulus Travma Acil Cerrahi Derg. 2018; 24:20–24. PMID: 29350363.12. Qiu Z, Qi W, Wu Y, Li L, Li C. Insurance status impacts survival of hepatocellular carcinoma patients after liver resection. Cancer Med. 2023; 12:17037–17046. PMID: 37455560.13. Zhou J, Sun H, Wang Z, Cong W, Wang J, Zeng M, et al. Guidelines for the diagnosis and treatment of hepatocellular carcinoma (2019 edition). Liver Cancer. 2020; 9:682–720. PMID: 33442540.14. Sugawara Y, Hibi T. Surgical treatment of hepatocellular carcinoma. Biosci Trends. 2021; 15:138–141. PMID: 33746184.15. Görgec B, Benedetti Cacciaguerra A, Lanari J, Russolillo N, Cipriani F, Aghayan D, et al. Assessment of textbook outcome in laparoscopic and open liver surgery. JAMA Surg. 2021; 156:e212064. PMID: 34076671.16. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213. PMID: 15273542.17. Moazzam Z, Alaimo L, Endo Y, Lima HA, Shaikh CF, Ratti F, et al. Variations in textbook oncologic outcomes after curative-intent resection: early versus intermediate hepatocellular carcinoma based on barcelona clinic liver cancer criteria and child-pugh classification. Ann Surg Oncol. 2023; 30:750–759. PMID: 36404380.18. Balzan S, Belghiti J, Farges O, Ogata S, Sauvanet A, Delefosse D, et al. The "50-50 criteria" on postoperative day 5: an accurate predictor of liver failure and death after hepatectomy. Ann Surg. 2005; 242:824–828. PMID: 16327492.19. Koch M, Garden OJ, Padbury R, Rahbari NN, Adam R, Capussotti L, et al. Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International Study Group of Liver Surgery. Surgery. 2011; 149:680–688. PMID: 21316725.20. Guidry CA, Davies SW, Willis RN, Dietch ZC, Shah PM, Sawyer RG. Operative start time does not affect post-operative infection risk. Surg Infect (Larchmt). 2016; 17:547–551. PMID: 27227370.21. George TJ, Arnaoutakis GJ, Merlo CA, Kemp CD, Baumgartner WA, Conte JV, et al. Association of operative time of day with outcomes after thoracic organ transplant. JAMA. 2011; 305:2193–2199. PMID: 21632483.22. McCormick F, Kadzielski J, Landrigan CP, Evans B, Herndon JH, Rubash HE. Surgeon fatigue: a prospective analysis of the incidence, risk, and intervals of predicted fatigue-related impairment in residents. Arch Surg. 2012; 147:430–435. PMID: 22785637.23. Goel N, Basner M, Rao H, Dinges DF. Circadian rhythms, sleep deprivation, and human performance. Prog Mol Biol Transl Sci. 2013; 119:155–190. PMID: 23899598.24. Bukoh MX, Siah CR. A systematic review on the structured handover interventions between nurses in improving patient safety outcomes. J Nurs Manag. 2020; 28:744–755. PMID: 31859377.25. Chen C, Zhang X, Gu C, Wang Y, Liu K, Pan X, et al. Surgery performed at night by continuously working surgeons contributes to a higher incidence of intraoperative complications in video-assisted thoracoscopic pulmonary resection: a large monocentric retrospective study. Eur J Cardiothorac Surg. 2020; 57:447–454. PMID: 31539044.26. Ishiyama Y, Ishida F, Ooae S, Takano Y, Seki J, Shimada S, et al. Surgical starting time in the morning versus the afternoon: propensity score matched analysis of operative outcomes following laparoscopic colectomy for colorectal cancer. Surg Endosc. 2019; 33:1769–1776. PMID: 30291444.27. Slaughter KN, Frumovitz M, Schmeler KM, Nick AM, Fleming ND, dos Reis R, et al. Minimally invasive surgery for endometrial cancer: does operative start time impact surgical and oncologic outcomes? Gynecol Oncol. 2014; 134:248–252. PMID: 24945591.28. Tsilimigras DI, Mehta R, Merath K, Bagante F, Paredes AZ, Farooq A, et al. Hospital variation in textbook outcomes following curative-intent resection of hepatocellular carcinoma: an international multi-institutional analysis. HPB (Oxford). 2020; 22:1305–1313. PMID: 31889626.29. Dal Cero M, Román M, Grande L, Yarnoz C, Estremiana F, Gantxegi A, et al. Textbook outcome and survival after gastric cancer resection with curative intent: a population-based analysis. Eur J Surg Oncol. 2022; 48:768–775. PMID: 34753620.30. A-Lai GH, Hu JR, Xu ZJ, Yao P, Zhong X, Wang YC, et al. Whether the start time of elective lung surgery impacts perioperative outcomes and cost? Front Surg. 2022; 9:922198. PMID: 36090328.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prognostic Factors and Clinicopathologic Features after Resection of Small Hepatocellular Carcinoma (< or =2 cm)
- The risk factors of early recurrence after hepatectomy in hepatocellular carcinoma
- Associating microwave ablation and portal vein ligation for staged hepatectomy for the treatment of huge hepatocellular carcinoma with cirrhosis
- Two-Stage Hepatectomy for Bilateral Hepatocellular Carcinoma with Bile Duct Tumor Thrombi
- Surgical Treatment of Ruptured Hepatocellular Carcinoma