Korean Circ J.
2024 Feb;54(2):63-75. 10.4070/kcj.2023.0195.
Comparison of Intracardiac Echocardiography Versus Transesophageal Echocardiography for Guidance During Transcatheter Aortic Valve Replacement
- Affiliations
-
- 1Division of Cardiology, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea
- 2Department of Cardiology, Myongji Hospital, Hanyang University College of Medicine, Goyang, Korea
- KMID: 2552231
- DOI: http://doi.org/10.4070/kcj.2023.0195
Abstract
- Background and Objectives
Evidence regarding the efficacy and safety of intracardiac echocardiography (ICE) for guidance during transcatheter aortic valve replacement (TAVR) is limited. This study aimed to compare the clinical efficacy and safety of ICE versus transesophageal echocardiography (TEE) for guiding TAVR.
Methods
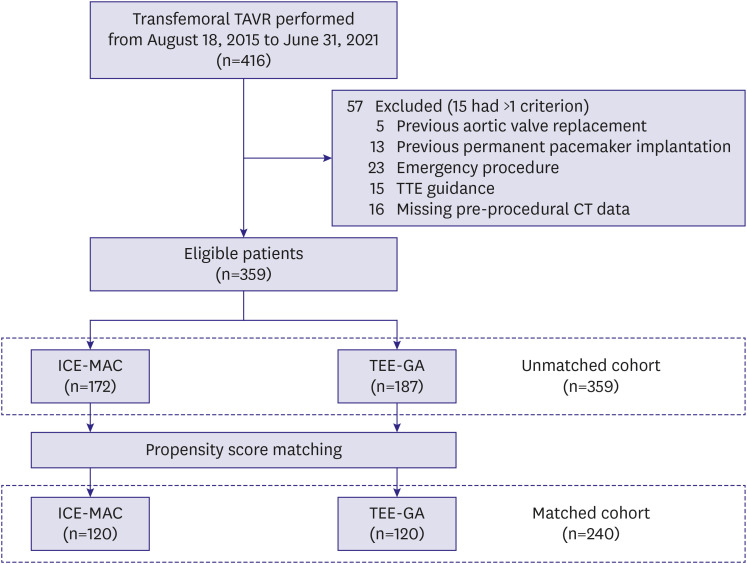
This prospective cohort study included patients who underwent TAVR from August 18, 2015, to June 31, 2021. Eligible patients were stratified by echocardiographic modality (ICE or TEE) and anesthesia mode (monitored anesthesia care [MAC] or general anesthesia [GA]). Primary outcome was the 1-year composite of all-cause mortality, rehospitalization for cardiovascular cause, or stroke, according to the Valve Academic Research Consortium-3 (VARC-3) definition. Propensity score matching was performed, and study outcomes were analyzed for the matched cohorts.
Results
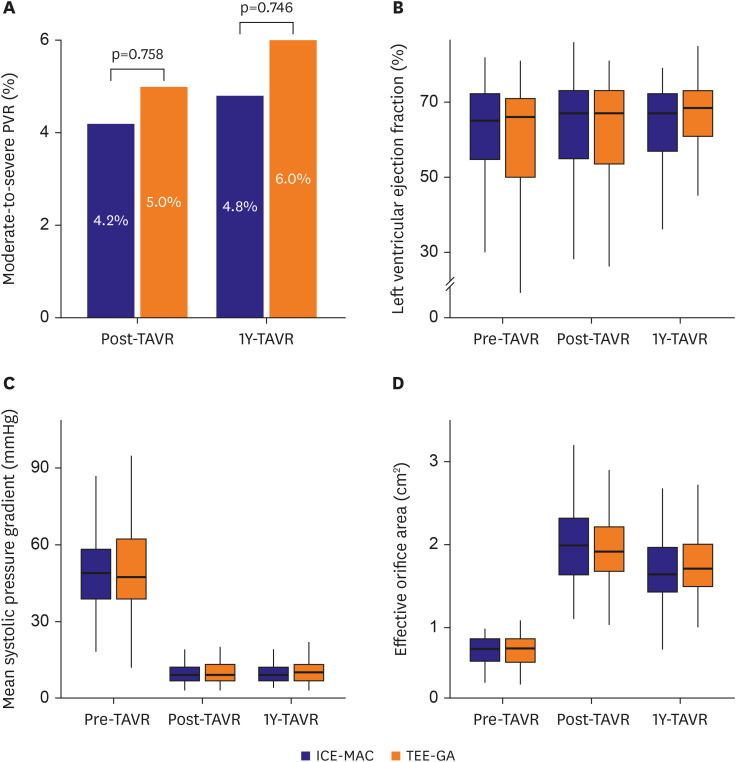
Of the 359 eligible patients, 120 patients were matched for the ICE-MAC and TEEGA groups, respectively. The incidence of primary outcome was similar between matched groups (18.3% vs. 20.0%; adjusted hazard ratio, 0.94; 95% confidence interval [CI], 0.53– 1.68; p=0.843). ICE-MAC and TEE-GA also had similar incidences of moderate-to-severe paravalvular regurgitation (PVR) (4.2% vs. 5.0%; adjusted odds ratio, 0.83; 95% CI, 0.23– 2.82; p=0.758), new permanent pacemaker implantation, and VARC-3 types 2–4 bleeding.
Conclusions
ICE was comparable to TEE for guidance during TAVR for the composite clinical efficacy outcome, with similar incidences of moderate-to-severe PVR, new permanent pacemaker implantation, and major bleeding. These results suggest that ICE could be a safe and effective alternative echocardiographic modality to TEE for guiding TAVR.
Keyword
Figure
Reference
-
1. Leon MB, Smith CR, Mack M, et al. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med. 2010; 363:1597–1607. PMID: 20961243.2. Smith CR, Leon MB, Mack MJ, et al. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med. 2011; 364:2187–2198. PMID: 21639811.3. Adams DH, Popma JJ, Reardon MJ, et al. Transcatheter aortic-valve replacement with a self-expanding prosthesis. N Engl J Med. 2014; 370:1790–1798. PMID: 24678937.4. Leon MB, Smith CR, Mack MJ, et al. Transcatheter or surgical aortic-valve replacement in intermediate-risk patients. N Engl J Med. 2016; 374:1609–1620. PMID: 27040324.5. Reardon MJ, Van Mieghem NM, Popma JJ, et al. Surgical or transcatheter aortic-valve replacement in intermediate-risk patients. N Engl J Med. 2017; 376:1321–1331. PMID: 28304219.6. Mack MJ, Leon MB, Thourani VH, et al. Transcatheter aortic-valve replacement with a balloon-expandable valve in low-risk patients. N Engl J Med. 2019; 380:1695–1705. PMID: 30883058.7. Popma JJ, Deeb GM, Yakubov SJ, et al. Transcatheter aortic-valve replacement with a self-expanding valve in low-risk patients. N Engl J Med. 2019; 380:1706–1715. PMID: 30883053.8. Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA Guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021; 143:e72–227. PMID: 33332150.9. Vahanian A, Beyersdorf F, Praz F, et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J. 2022; 43:561–632. PMID: 34453165.10. Rahhab Z, El Faquir N, Tchetche D, et al. Expanding the indications for transcatheter aortic valve implantation. Nat Rev Cardiol. 2020; 17:75–84. PMID: 31527743.11. Vahanian A, Alfieri O, Al-Attar N, et al. Transcatheter valve implantation for patients with aortic stenosis: a position statement from the European association of cardio-thoracic surgery (EACTS) and the European Society of Cardiology (ESC), in collaboration with the European Association of Percutaneous Cardiovascular Interventions (EAPCI). EuroIntervention. 2008; 4:193–199. PMID: 19110783.12. Zamorano JL, Badano LP, Bruce C, et al. EAE/ASE recommendations for the use of echocardiography in new transcatheter interventions for valvular heart disease. Eur Heart J. 2011; 32:2189–2214. PMID: 21885465.13. Hahn RT, Nicoara A, Kapadia S, Svensson L, Martin R. Echocardiographic imaging for transcatheter aortic valve replacement. J Am Soc Echocardiogr. 2018; 31:405–433. PMID: 29275985.14. Villablanca PA, Mohananey D, Ramakrishna H. Comparison of local versus general anesthesia in patients undergoing transcatheter aortic valve replacement: an updated meta-analysis. Catheter Cardiovasc Interv. 2018; 92:1018–1019. PMID: 29659154.15. Bartel T, Bonaros N, Müller L, et al. Intracardiac echocardiography: a new guiding tool for transcatheter aortic valve replacement. J Am Soc Echocardiogr. 2011; 24:966–975. PMID: 21641183.16. Alkhouli M, Hijazi ZM, Holmes DR Jr, Rihal CS, Wiegers SE. Intracardiac echocardiography in structural heart disease interventions. JACC Cardiovasc Interv. 2018; 11:2133–2147. PMID: 30409271.17. Enriquez A, Saenz LC, Rosso R, et al. Use of intracardiac echocardiography in interventional cardiology: working with the anatomy rather than fighting it. Circulation. 2018; 137:2278–2294. PMID: 29784681.18. Généreux P, Piazza N, Alu MC, et al. Valve academic research consortium 3: updated endpoint definitions for aortic valve clinical research. J Am Coll Cardiol. 2021; 77:2717–2746. PMID: 33888385.19. Zaid S, Haniyeh AA, Rosenzveig A, et al. Minimalist transcatheter aortic valve replacement misses paravalvular regurgitation: incidence and echocardiographic distribution of missed paravalvular regurgitation. Catheter Cardiovasc Interv. 2023; 101:180–186. PMID: 36478154.20. Hayek SS, Corrigan FE 3rd, Condado JF, et al. Paravalvular regurgitation after transcatheter aortic valve replacement: comparing transthoracic versus transesophageal echocardiographic guidance. J Am Soc Echocardiogr. 2017; 30:533–540. PMID: 28391002.21. Lerakis S, Hayek SS, Douglas PS. Paravalvular aortic leak after transcatheter aortic valve replacement: current knowledge. Circulation. 2013; 127:397–407. PMID: 23339094.22. Jilaihawi H, Makkar RR, Kashif M, et al. A revised methodology for aortic-valvar complex calcium quantification for transcatheter aortic valve implantation. Eur Heart J Cardiovasc Imaging. 2014; 15:1324–1332. PMID: 25187618.23. Vincent F, Ternacle J, Denimal T, et al. Transcatheter aortic valve replacement in bicuspid aortic valve stenosis. Circulation. 2021; 143:1043–1061. PMID: 33683945.24. Freitas-Ferraz AB, Bernier M, Vaillancourt R, et al. Safety of transesophageal echocardiography to guide structural cardiac interventions. J Am Coll Cardiol. 2020; 75:3164–3173. PMID: 32586591.25. Zahid S, Gowda S, Hashem A, et al. Feasibility and safety of intracardiac echocardiography use in transcatheter left atrial appendage closure procedures. J Soc Cardiovasc Angiogr Interv. 2022; 1:100510.26. Babaliaros V, Devireddy C, Lerakis S, et al. Comparison of transfemoral transcatheter aortic valve replacement performed in the catheterization laboratory (minimalist approach) versus hybrid operating room (standard approach): outcomes and cost analysis. JACC Cardiovasc Interv. 2014; 7:898–904. PMID: 25086843.27. Hosoba S, Yamamoto M, Shioda K, et al. Safety and efficacy of minimalist approach in transfemoral transcatheter aortic valve replacement: insights from the Optimized transCathEter vAlvular interventioN-Transcatheter Aortic Valve Implantation (OCEAN-TAVI) registry. Interact Cardiovasc Thorac Surg. 2018; 26:420–424. PMID: 29096029.28. Thiele H, Kurz T, Feistritzer HJ, et al. General versus local anesthesia with conscious sedation in transcatheter aortic valve implantation: the randomized SOLVE-TAVI trial. Circulation. 2020; 142:1437–1447. PMID: 32819145.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Echocardiography in Transcatheter Aortic Valve Implantation and Mitral Valve Clip
- Contrast-free (Zero-contrast) TAVR for Severe Aortic Stenosis in Patient with Chronic Kidney Disease
- Left Atrial Dissection by Aorto-Left Atrial Fistula after Aortic Valve Replacement: A case report
- A Case of 51 Year Old Woman with Quadricuspid Aortic Valve Associated with Regurgitation
- Expanding transcatheter aortic valve replacement into uncharted indications