Ann Lab Med.
2023 Sep;43(5):485-492. 10.3343/alm.2023.43.5.485.
Performance Validation of Three Scoring Systems for the Prediction of Thrombotic Microangiopathy Due to Severe ADAMTS13 Deficiency and the Response to Therapeutic Plasma Exchange: First Study in Korea
- Affiliations
-
- 1Department of Laboratory Medicine, University of Ulsan College of Medicine, Ulsan University Hospital, Ulsan, Korea
- 2Department of Hematology and Cellular Therapy, University of Ulsan College of Medicine, Ulsan University Hospital, Ulsan, Korea
- KMID: 2551997
- DOI: http://doi.org/10.3343/alm.2023.43.5.485
Abstract
- Background
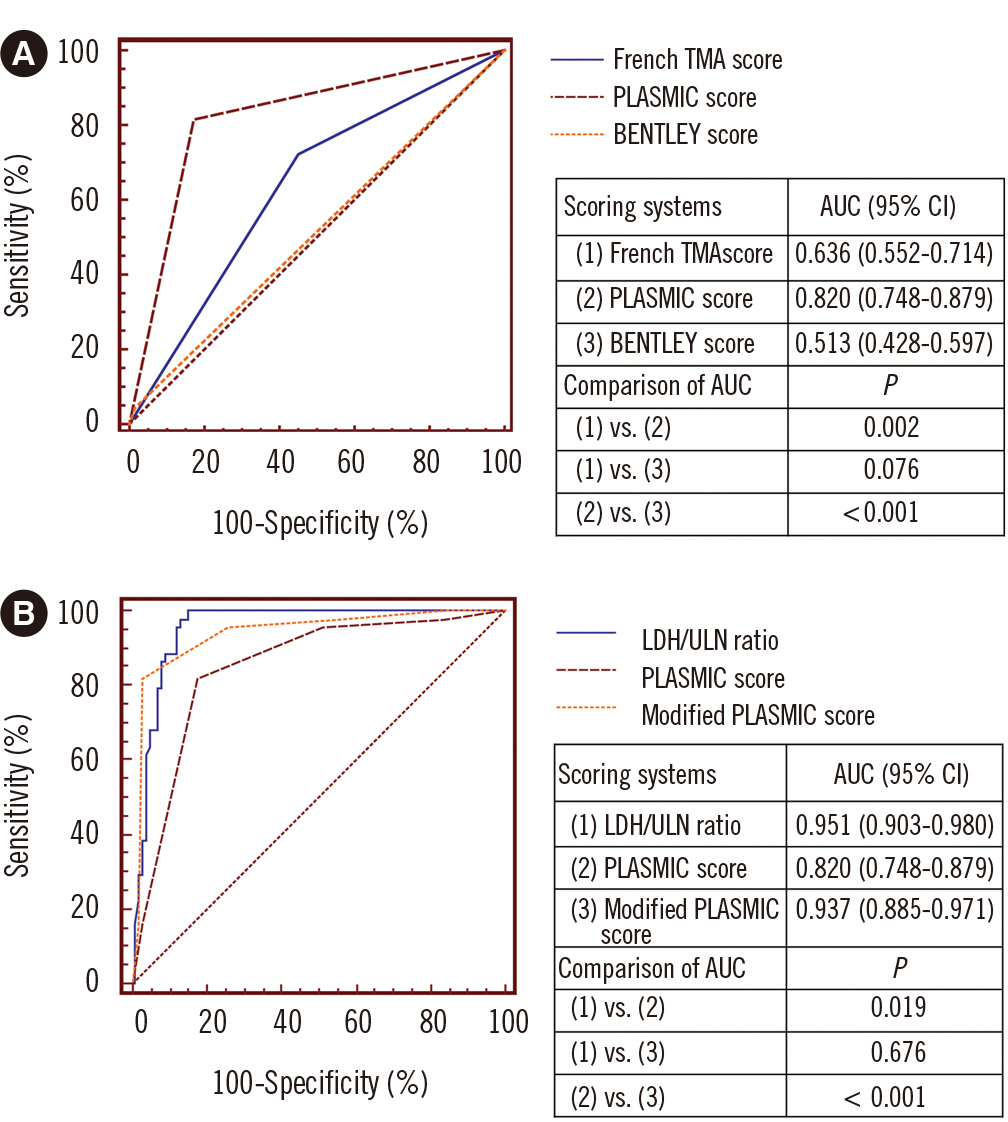
The BENTLEY score (B-S), French thrombotic microangiopathy (TMA) Reference Center score (FTMA-S), and PLASMIC score (PLASMIC-S) have been developed for TMA diagnostic prediction. We retrospectively validated their predictive performances in patients with severe (<10%) disintegrin and metalloprotease with thrombospondin type 1 motif, member 13 (ADAMTS13) deficiency in terms of the risk of TMA and response to therapeutic plasma exchange (TPE).
Methods
The predictive performances of the three scoring systems were compared in 145 patients with suspected TMA who underwent ADAMTS13 activity tests between January 2014 and September 2022. The response to TPE and mortality in TMA-positive patients were compared after risk stratification, using the Mann–Whitney U and Fisher’s exact tests.
Results
The PLASMIC-S, FTMA-S, and B-S showed area under the curve values of 0.820, 0.636, and 0.513, respectively, for predicting TMA positivity in high-risk patients. The PLASMIC-S showed higher sensitivity (81.8%), negative predictive value (91.2%), positive predictive value (PPV; 66.7%), and accuracy (82.1%) than the FTMA-S (72.7%, 82.1%, 41.0%, and 60.0%, respectively) and B-S (4.6%, 70.2%, 50.0%, and 69.7%, respectively). The PLASMIC-S also showed higher specificity than the FTMA-S (82.2% vs. 54.5%). The modified PLASMIC-S, including lactate dehydrogenase/upper limit of normal ratios, increased the specificity, PPV, and accuracy to 97.0%, 92.3%, and 92.4%, respectively. In TMA-positive patients, high risk assessed by the PLASMIC-S predicted higher platelet recovery rates and less TPE sessions required for recovery than for those assessed at low-to-intermediate risk.
Conclusions
PLASMIC-S is the preferred scoring system for detecting patients with TMA positivity and for prognosis before confirmation of ADAMTS13 activity.
Keyword
Figure
Reference
-
1. George JN, Nester CM. 2014; Syndromes of thrombotic microangiopathy. N Engl J Med. 371:654–66. DOI: 10.1056/NEJMra1312353. PMID: 25119611.
Article2. Bendapudi PK, Hurwitz S, Fry A, Marques MB, Waldo SW, Li A, et al. 2017; Derivation and external validation of the PLASMIC score for rapid assessment of adults with thrombotic microangiopathies: a cohort study. Lancet Haematol. 4:e157–64. DOI: 10.1016/S2352-3026(17)30026-1. PMID: 28259520.
Article3. Bendapudi PK, Li A, Hamdan A, Uhl L, Kaufman R, Stowell C, et al. 2015; Impact of severe ADAMTS13 deficiency on clinical presentation and outcomes in patients with thrombotic microangiopathies: the experience of the Harvard TMA Research Collaborative. Br J Haematol. 171:836–44. DOI: 10.1111/bjh.13658. PMID: 26314936.
Article4. Hassan S, Westwood JP, Ellis D, Laing C, Mc Guckin S, Benjamin S, et al. 2015; The utility of ADAMTS13 in differentiating TTP from other acute thrombotic microangiopathies: results from the UK TTP Registry. Br J Haematol. 171:830–5. DOI: 10.1111/bjh.13654. PMID: 26359646.
Article5. Moake JL, Rudy CK, Troll JH, Weinstein MJ, Colannino NM, Azocar J, et al. 1982; Unusually large plasma factor VIII:von Willebrand factor multimers in chronic relapsing thrombotic thrombocytopenic purpura. N Engl J Med. 307:1432–5. DOI: 10.1056/NEJM198212023072306. PMID: 6813740.
Article6. Fujikawa K, Suzuki H, McMullen B, Chung D. 2001; Purification of human von Willebrand factor-cleaving protease and its identification as a new member of the metalloproteinase family. Blood. 98:1662–6. DOI: 10.1182/blood.V98.6.1662. PMID: 11535495.
Article7. Gerritsen HE, Robles R, Lämmle B, Furlan M. 2001; Partial amino acid sequence of purified von Willebrand factor-cleaving protease. Blood. 98:1654–61. DOI: 10.1182/blood.V98.6.1654. PMID: 11535494.
Article8. Tsai HM, Lian EC. 1998; Antibodies to von Willebrand factor-cleaving protease in acute thrombotic thrombocytopenic purpura. N Engl J Med. 339:1585–94. DOI: 10.1056/NEJM199811263392203. PMID: 9828246. PMCID: PMC3159001.
Article9. Furlan M, Robles R, Galbusera M, Remuzzi G, Kyrle PA, Brenner B, et al. 1998; von Willebrand factor-cleaving protease in thrombotic thrombocytopenic purpura and the hemolytic-uremic syndrome. N Engl J Med. 339:1578–84. DOI: 10.1056/NEJM199811263392202. PMID: 9828245.
Article10. Amorosi EL, Ultmann JE. 1966; Thrombotic thrombocytopenic purpura: report of 16 cases and review of the literature. Medicine. 45:139–60. DOI: 10.1097/00005792-196603000-00003.11. Bell WR, Braine HG, Ness PM, Kickler TS. 1991; Improved survival in thrombotic thrombocytopenic purpura-hemolytic uremic syndrome. Clinical experience in 108 patients. N Engl J Med. 325:398–403. DOI: 10.1056/NEJM199108083250605. PMID: 2062331.
Article12. Rock GA, Shumak KH, Buskard NA, Blanchette VS, Kelton JG, Nair RC, et al. 1991; Comparison of plasma exchange with plasma infusion in the treatment of thrombotic thrombocytopenic purpura. Canadian apheresis study group. N Engl J Med. 325:393–7. DOI: 10.1056/NEJM199108083250604. PMID: 2062330.
Article13. Zheng XL. 2015; ADAMTS13 and von Willebrand factor in thrombotic thrombocytopenic purpura. Annu Rev Med. 66:211–25. DOI: 10.1146/annurev-med-061813-013241. PMID: 25587650. PMCID: PMC4599565.
Article14. Zheng XL, Kaufman RM, Goodnough LT, Sadler JE. 2004; Effect of plasma exchange on plasma ADAMTS13 metalloprotease activity, inhibitor level, and clinical outcome in patients with idiopathic and nonidiopathic thrombotic thrombocytopenic purpura. Blood. 103:4043–9. DOI: 10.1182/blood-2003-11-4035. PMID: 14982878. PMCID: PMC7816822.
Article15. Vesely SK, George JN, Lämmle B, Studt JD, Alberio L, El-Harake MA, et al. 2003; ADAMTS13 activity in thrombotic thrombocytopenic purpura-hemolytic uremic syndrome: relation to presenting features and clinical outcomes in a prospective cohort of 142 patients. Blood. 102:60–8. DOI: 10.1182/blood-2003-01-0193. PMID: 12637323.
Article16. Veyradier A, Obert B, Houllier A, Meyer D, Girma JP. 2001; Specific von Willebrand factor-cleaving protease in thrombotic microangiopathies: a study of 111 cases. Blood. 98:1765–72. DOI: 10.1182/blood.V98.6.1765. PMID: 11535510.
Article17. Coppo P, Bengoufa D, Veyradier A, Wolf M, Bussel A, Millot GA, et al. 2004; Severe ADAMTS13 deficiency in adult idiopathic thrombotic microangiopathies defines a subset of patients characterized by various autoimmune manifestations, lower platelet count, and mild renal involvement. Medicine. 83:233–44. DOI: 10.1097/01.md.0000133622.03370.07. PMID: 15232311.
Article18. Coppo P, Schwarzinger M, Buffet M, Wynckel A, Clabault K, Presne C, et al. 2010; Predictive features of severe acquired ADAMTS13 deficiency in idiopathic thrombotic microangiopathies: the French TMA reference center experience. PLoS One. 5:e10208. DOI: 10.1371/journal.pone.0010208. PMID: 20436664. PMCID: PMC2859048.
Article19. Shah N, Rutherford C, Matevosyan K, Shen YM, Sarode R. 2013; Role of ADAMTS13 in the management of thrombotic microangiopathies including thrombotic thrombocytopenic purpura (TTP). Br J Haematol. 163:514–9. DOI: 10.1111/bjh.12569. PMID: 24111495.
Article20. Scully M, Yarranton H, Liesner R, Cavenagh J, Hunt B, Benjamin S, et al. 2008; Regional UK TTP registry: correlation with laboratory ADAMTS 13 analysis and clinical features. Br J Haematol. 142:819–26. DOI: 10.1111/j.1365-2141.2008.07276.x. PMID: 18637802.
Article21. Mariotte E, Azoulay E, Galicier L, Rondeau E, Zouiti F, Boisseau P, et al. 2016; Epidemiology and pathophysiology of adulthood-onset thrombotic microangiopathy with severe ADAMTS13 deficiency (thrombotic thrombocytopenic purpura): a cross-sectional analysis of the French national registry for thrombotic microangiopathy. Lancet Haematol. 3:e237–45. DOI: 10.1016/S2352-3026(16)30018-7. PMID: 27132698.
Article22. Li A, Makar RS, Hurwitz S, Uhl L, Kaufman RM, Stowell CP, et al. 2016; Treatment with or without plasma exchange for patients with acquired thrombotic microangiopathy not associated with severe ADAMTS13 deficiency: a propensity score-matched study. Transfusion. 56:2069–77. DOI: 10.1111/trf.13654. PMID: 27232383.
Article23. Connell NT, Cheves T, Sweeney JD. 2016; Effect of ADAMTS13 activity turnaround time on plasma utilization for suspected thrombotic thrombocytopenic purpura. Transfusion. 56:354–9. DOI: 10.1111/trf.13359. PMID: 26456149.
Article24. Bentley MJ, Lehman CM, Blaylock RC, Wilson AR, Rodgers GM. 2010; The utility of patient characteristics in predicting severe ADAMTS13 deficiency and response to plasma exchange. Transfusion. 50:1654–64. DOI: 10.1111/j.1537-2995.2010.02653.x. PMID: 20412532.
Article25. Bentley MJ, Wilson AR, Rodgers GM. 2013; Performance of a clinical prediction score for thrombotic thrombocytopenic purpura in an independent cohort. Vox Sang. 105:313–8. DOI: 10.1111/vox.12050. PMID: 23662653.
Article26. Li A, Khalighi PR, Wu Q, Garcia DA. 2018; External validation of the PLASMIC score: a clinical prediction tool for thrombotic thrombocytopenic purpura diagnosis and treatment. J Thromb Haemost. 16:164–9. DOI: 10.1111/jth.13882. PMID: 29064619. PMCID: PMC5760324.
Article27. Bendapudi PK, Upadhyay V, Sun L, Marques MB, Makar RS. 2017; Clinical scoring systems in thrombotic microangiopathies. Semin Thromb Hemost. 43:540–8. DOI: 10.1055/s-0037-1603100. PMID: 28597458.
Article28. Liu A, Dhaliwal N, Upreti H, Kasmani J, Dane K, Moliterno A, et al. 2021; Reduced sensitivity of PLASMIC and French scores for the diagnosis of thrombotic thrombocytopenic purpura in older individuals. Transfusion. 61:266–73. DOI: 10.1111/trf.16188. PMID: 33179792. PMCID: PMC8859842.
Article29. Zhao N, Zhou L, Hu X, Sun G, Chen C, Fan X, et al. 2020; A modified PLASMIC score including the lactate dehydrogenase/the upper limit of normal ratio more accurately identifies Chinese thrombotic thrombocytopenic purpura patients than the original PLASMIC score. J Clin Apher. 35:79–85. DOI: 10.1002/jca.21760. PMID: 31724781.
Article30. Patriquin CJ, Pavenski K. 2020; Plasma exchange in TTP: to taper or not to taper. Transfusion. 60:1647–8. DOI: 10.1111/trf.15969. PMID: 33460108.31. Hanley JA, McNeil BJ. 1983; A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology. 148:839–43. DOI: 10.1148/radiology.148.3.6878708. PMID: 6878708.
Article32. Fage N, Orvain C, Henry N, Mellaza C, Beloncle F, Tuffigo M, et al. 2021; Proteinuria increases the PLASMIC and French scores performance to predict thrombotic thrombocytopenic purpura in patients with thrombotic microangiopathy syndrome. Kidney Int Rep. 7:221–31. DOI: 10.1016/j.ekir.2021.11.009. PMID: 35155861. PMCID: PMC8820983.
Article33. Kato S, Matsumoto M, Matsuyama T, Isonishi A, Hiura H, Fujimura Y. 2006; Novel monoclonal antibody-based enzyme immunoassay for determining plasma levels of ADAMTS13 activity. Transfusion. 46:1444–52. DOI: 10.1111/j.1537-2995.2006.00914.x. PMID: 16934083.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Thrombotic Thrombocytopenic Purpura with Exacerbation after Incomplete Remission of Therapeutic Plasma Exchange
- Differential Diagnosis and Treatment of Thrombotic Microangiopathy Syndrome
- Recent advances in the management of immune-mediated thrombotic thrombocytopenic purpura
- Therapeutic Plasma Exchange in a Patient with Hemophagocytic Lymphohistiocytosis
- A Case Report of Rituximab Therapy for Recurrent Thrombotic Thrombocytopenia Purpura