J Stroke.
2024 Jan;26(1):87-94. 10.5853/jos.2023.01669.
Association Between Anemia and Clinical Outcome in Acute Ischemic Stroke Patients Treated With Endovascular Treatment
- Affiliations
-
- 1School for Cardiovascular Diseases (CARIM), Maastricht University, Maastricht, The Netherlands
- 2Department of Neurology, Maastricht University Medical Center+, Maastricht, The Netherlands
- 3Department of Radiology and Nuclear Medicine, Maastricht University Medical Center+, Maastricht, The Netherlands
- 4School for Mental Health and Neuroscience (MHeNs), Maastricht University, Maastricht, The Netherlands
- KMID: 2551350
- DOI: http://doi.org/10.5853/jos.2023.01669
Abstract
- Background and Purpose
Endovascular treatment (EVT) is the preferred treatment option in eligible acute ischemic stroke (AIS) patients with a large vessel occlusion of the anterior circulation. Several comorbidities have been identified that can affect clinical outcomes. Various studies have investigated the association between anemia and clinical outcome and found conflicting results. The aim is to investigate the association between pre-EVT anemia and clinical outcomes at different time points post-EVT, primarily focusing on the National Institutes of Health Stroke Scale (NIHSS) at 24–48 hours.
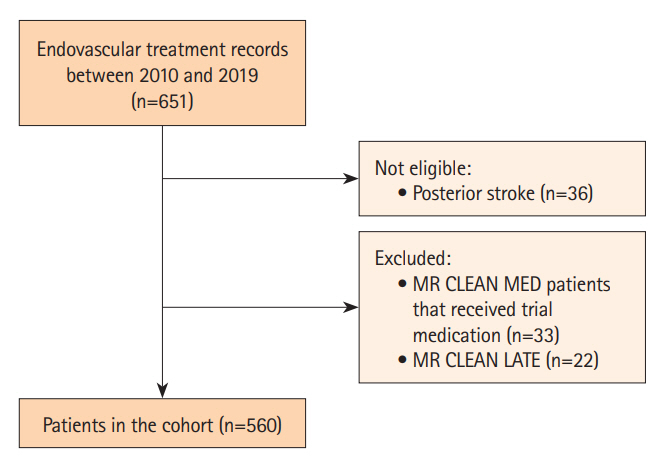
Methods
We prospectively included 560 AIS patients who received EVT in the Maastricht University Medical Center+. Hemoglobin levels (Hb; g/dL) were determined on admission. Hb levels were also categorized into two groups: anemia (male: Hb ≤12.9 g/dL; female: Hb ≤11.9 g/dL) and no anemia. Multiple imputation was used to handle missing data. Multivariable regression was used to investigate the association between anemia or Hb levels and clinical outcomes.
Results
Anemia was present in 26% of the patients. Multivariable regression did not show a significant association between anemia or Hb levels and NIHSS at 24–48 hours (adjusted β [aβ]anemia: 1.44, 95% confidence interval [CI]: -0.47 to 3.36; aβHb: -0.37, 95% CI: -0.88 to 0.13). However, multivariable regression showed significant associations with modified Rankin Scale (adjusted common odds ratio [acOR]anemia: 1.66, 95% CI: 1.12 to 2.48; acORHb: 0.83, 95% CI: 0.75 to 0.93) and poor functional outcome at 90 days (adjusted OR [aOR]anemia: 2.09, 95% CI: 1.21 to 3.63; aORHb: 0.80, 95% CI: 0.69 to 0.92).
Conclusion
Anemia was not independently associated with early neurological deficit (NIHSS) post-AIS, suggesting it is more suitable as a general frailty marker.
Figure
Reference
-
References
1. Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015; 372:11–20.2. Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016; 387:1723–1731.3. Olthuis SGH, Pirson FAV, Pinckaers FME, Hinsenveld WH, Nieboer D, Ceulemans A, et al. Endovascular treatment versus no endovascular treatment after 6-24 h in patients with ischaemic stroke and collateral flow on CT angiography (MR CLEANLATE) in the Netherlands: a multicentre, open-label, blinded-endpoint, randomised, controlled, phase 3 trial. Lancet. 2023; 401:1371–1380.4. Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, OrtegaGutierrez S, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018; 378:708–718.5. Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018; 378:11–21.6. Compagne KCJ, Kappelhof M, Hinsenveld WH, Brouwer J, Goldhoorn RB, Uyttenboogaart M, et al. Improvements in endovascular treatment for acute ischemic stroke: a longitudinal study in the MR CLEAN registry. Stroke. 2022; 53:1863–1872.7. Simic´-Panic´ D, Boškovic´ K, Milic´evic´ M, Rabi Žikic´ T, Cvjetkovic´ Bošnjak M, Tomaševic´-Todorovic´ S, et al. The impact of comorbidity on rehabilitation outcome after ischemic stroke. Acta Clin Croat. 2018; 57:5–15.8. Khan MF, Shamael I, Zaman Q, Mahmood A, Siddiqui M. Association of anemia with stroke severity in acute ischemic stroke patients. Cureus. 2018; 10:e2870.9. Desai A, Oh D, Rao EM, Sahoo S, Mahajan UV, Labak CM, et al. Impact of anemia on acute ischemic stroke outcomes: a systematic review of the literature. PLoS One. 2023; 18:e0280025.10. Akpinar CK, Gurkas E, Aytac E. Moderate to severe anemia is associated with poor functional outcome in acute stroke patients treated with mechanical thrombectomy. Interv Neurol. 2018; 7:12–18.11. Altersberger VL, Kellert L, Al Sultan AS, Martinez-Majander N, Hametner C, Eskandari A, et al. Effect of haemoglobin levels on outcome in intravenous thrombolysis-treated stroke patients. Eur Stroke J. 2020; 5:138–147.12. Barlas RS, Honney K, Loke YK, McCall SJ, Bettencourt-Silva JH, Clark AB, et al. Impact of hemoglobin levels and anemia on mortality in acute stroke: analysis of UK regional registry data, systematic review, and meta-analysis. J Am Heart Assoc. 2016; 5:e003019.13. Park YH, Kim BJ, Kim JS, Yang MH, Jang MS, Kim N, et al. Impact of both ends of the hemoglobin range on clinical outcomes in acute ischemic stroke. Stroke. 2013; 44:3220–3222.14. Nisar T, Shapouran S, Abu-Hadid O, Shaulov S, Tofade T, Patel J, et al. Association of anemia with functional outcomes in patients with mechanical thrombectomy. Clin Neurol Neurosurg. 2021; 211:107028.15. Pienimäki JP, Protto S, Hakomäki E, Jolma P, Sillanpää N. Anemia predicts poor clinical outcome in mechanical thrombectomy patients with fair or good collateral circulation. Cerebrovasc Dis Extra. 2020; 10:139–147.16. Bellwald S, Balasubramaniam R, Nagler M, Burri MS, Fischer SDA, Hakim A, et al. Association of anemia and hemoglobin decrease during acute stroke treatment with infarct growth and clinical outcome. PLoS One. 2018; 13:e0203535.17. Nisar T, Lebioda K, Shaulov S, Shapouran S, Abu-Hadid O, Tofade T, et al. Interplay between anemia parameters and collateral status in patients who undergo mechanical thrombectomy. J Clin Neurosci. 2022; 104:34–41.18. Li Z, Zhou T, Li Y, Chen P, Chen L. Anemia increases the mortality risk in patients with stroke: a meta-analysis of cohort studies. Sci Rep. 2016; 6:26636.19. Hao Z, Wu B, Wang D, Lin S, Tao W, Liu M. A cohort study of patients with anemia on admission and fatality after acute ischemic stroke. J Clin Neurosci. 2013; 20:37–42.20. Ganesh A, Ospel JM, Menon BK, Demchuk AM, McTaggart RA, Nogueira RG, et al. Assessment of discrepancies between follow-up infarct volume and 90-day outcomes among patients with ischemic stroke who received endovascular therapy. JAMA Netw Open. 2021; 4:e2132376.21. Furlan JC, Fang J, Silver FL. Acute ischemic stroke and abnormal blood hemoglobin concentration. Acta Neurol Scand. 2016; 134:123–130.22. Sharma K, Johnson DJ, Johnson B, Frank SM, Stevens RD. Hemoglobin concentration does not impact 3-month outcome following acute ischemic stroke. BMC Neurol. 2018; 18:78.23. Chang TR, Boehme AK, Aysenne A, Albright KC, Burns C, Beasley TM, et al. Nadir hemoglobin is associated with poor outcome from intracerebral hemorrhage. Springerplus. 2013; 2:379.24. Young FB, Weir CJ, Lees KR. Comparison of the National Institutes of Health Stroke Scale with disability outcome measures in acute stroke trials. Stroke. 2005; 36:2187–2192.25. Taylor-Rowan M, Wilson A, Dawson J, Quinn TJ. Functional assessment for acute stroke trials: properties, analysis, and application. Front Neurol. 2018; 9:191.26. Chalos V, van der Ende NAM, Lingsma HF, Mulder MJHL, Venema E, Dijkland SA, et al. National Institutes of Health Stroke Scale: an alternative primary outcome measure for trials of acute treatment for ischemic stroke. Stroke. 2020; 51:282–290.27. van der Steen W, van de Graaf RA, Chalos V, Lingsma HF, van Doormaal PJ, Coutinho JM, et al. Safety and efficacy of aspirin, unfractionated heparin, both, or neither during endovascular stroke treatment (MR CLEAN-MED): an open-label, multicentre, randomised controlled trial. Lancet. 2022; 399:1059–1069.28. Jansen IGH, Mulder MJHL, Goldhoorn RB; MR CLEAN Registry Investigators. Endovascular treatment for acute ischaemic stroke in routine clinical practice: prospective, observational cohort study (MR CLEAN registry). BMJ. 2018; 360:k949.29. LeCouffe NE, Kappelhof M, Treurniet KM, Rinkel LA, Bruggeman AE, Berkhemer OA, et al. A randomized trial of intravenous alteplase before endovascular treatment for stroke. N Engl J Med. 2021; 385:1833–1844.30. World Health Organization. Anaemia: how is it defined? Geneva: World Health Organization;2008. [cited Year Month Date]. Available from: https://www.who.int/data/nutrition/nlis/info/anaemia.31. Cappellini MD, Motta I. Anemia in clinical practice-definition and classification: does hemoglobin change with aging? Semin Hematol. 2015; 52:261–269.32. van Buuren S, Groothuis-Oudshoorn K. mice: Multivariate imputation by chained equations in R. J Stat Softw. 2011; 45:1–67.33. von Hippel PT. How many imputations do you need? A two-stage calculation using a quadratic rule. Sociol Methods Res. 2020; 49:699–718.34. Harrell FE Jr, Lee KL, Califf RM, Pryor DB, Rosati RA. Regression modelling strategies for improved prognostic prediction. Stat Med. 1984; 3:143–152.35. Gandhi SJ, Hagans I, Nathan K, Hunter K, Roy S. Prevalence, comorbidity and investigation of anemia in the primary care office. J Clin Med Res. 2017; 9:970–980.36. den Elzen WP, Willems JM, Westendorp RG, de Craen AJ, Assendelft WJ, Gussekloo J. Effect of anemia and comorbidity on functional status and mortality in old age: results from the Leiden 85-plus study. CMAJ. 2009; 181:151–157.37. Salive ME, Cornoni-Huntley J, Guralnik JM, Phillips CL, Wallace RB, Ostfeld AM, et al. Anemia and hemoglobin levels in older persons: relationship with age, gender, and health status. J Am Geriatr Soc. 1992; 40:489–496.38. Gaskell H, Derry S, Andrew Moore R, McQuay HJ. Prevalence of anaemia in older persons: systematic review. BMC Geriatr. 2008; 8:1.39. Stauder R, Valent P, Theurl I. Anemia at older age: etiologies, clinical implications, and management. Blood. 2018; 131:505–514.40. Gottesman RF, Sojkova J, Beason-Held LL, An Y, Longo DL, Ferrucci L, et al. Patterns of regional cerebral blood flow associated with low hemoglobin in the Baltimore Longitudinal Study of Aging. J Gerontol A Biol Sci Med Sci. 2012; 67:963–969.41. Leal-Noval SR, Múñoz-Gómez M, Murillo-Cabezas F. Optimal hemoglobin concentration in patients with subarachnoid hemorrhage, acute ischemic stroke and traumatic brain injury. Curr Opin Crit Care. 2008; 14:156–162.42. Ducrocq G, Gonzalez-Juanatey JR, Puymirat E, Lemesle G, Cachanado M, Durand-Zaleski I, et al. Effect of a restrictive vs liberal blood transfusion strategy on major cardiovascular events among patients with acute myocardial infarction and anemia: the REALITY randomized clinical trial. JAMA. 2021; 325:552–560.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Multiple Territory Ischemic Stroke Aggravated by Severe Anemia
- Endovascular Treatment of Acute Ischemic Stroke
- Intravenous Thrombolysis and Endovascular Thrombectomy in Acute Ischemic Stroke with Minor Symptom
- Reperfusion therapy in acute ischemic stroke
- Previous and Recent Evidence of Endovascular Therapy in Acute Ischemic Stroke