J Korean Med Sci.
2024 Jan;39(3):e24. 10.3346/jkms.2024.39.e24.
Differences in Clinical Outcomes Between Hydroxyurea-Resistant and -Intolerant Polycythemia Vera Patients
- Affiliations
-
- 1Department of Hematology, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Divison of Hematology and Medical Oncology, Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea
- 3Department of Internal Medicine, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea
- 4Divison of Hematology, Department of Internal Medicine, Gachon University Gil Medical Center, Incheon, Korea
- 5Divison of Hematology-Oncology, Department of Internal Medicine, Korea University Guro Hospital, Seoul, Korea
- 6Department of Internal Medicine, Daegu Catholic University School of Medicine, Daegu, Korea
- 7Department of Internal Medicine, Yeungnam University College of Medicine, Daegu, Korea
- 8Division of Hematology-Oncology, Department of Internal Medicine, Soonchunhyang University College of Medicine, Seoul, Korea
- 9Divison of Hematology, Department of Internal Medicine, Konkuk University Medical Center, Konkuk University, Seoul, Korea
- KMID: 2551176
- DOI: http://doi.org/10.3346/jkms.2024.39.e24
Abstract
- Background
Previous studies have suggested that patients with polycythemia vera (PV) who exhibit hydroxyurea-resistance (HU-R) and -intolerance (HU-I) may have distinct characteristics and clinical outcomes. However, to date, no studies have reported a comparison between these two groups or assessed prognostic factors in these patients.
Methods
The objective of this study was to evaluate clinical outcomes and identify prognostic factors among PV patients with HU-R or HU-I. We conducted a review of PV patients who received frontline treatment with HU from nine centers and identified 90 patients with HU-R or HU-I.
Results
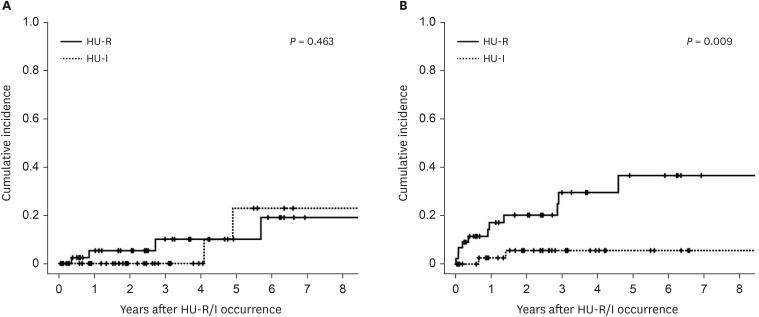
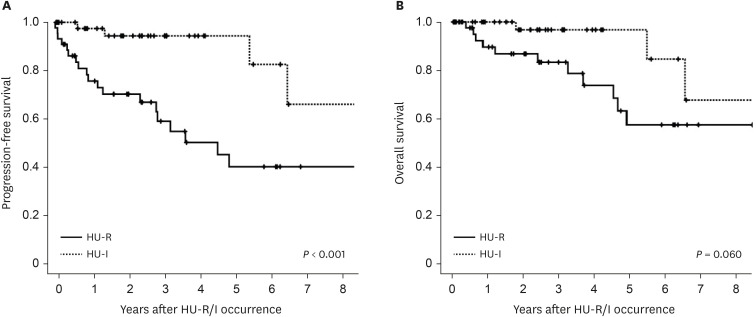
The cumulative incidence of thrombosis after 7 years of HU-R/I was 21.4%, and the incidence of disease progression was 22.5%. Comparing the HU-R and HU-I groups, the HU-R group had a significantly higher rate of disease progression (36.7% vs. 0.56%, P = 0.009), while there was no significant difference in thrombosis incidence (19.0% vs. 22.9%, P = 0.463). Multivariate analysis revealed that HU-R was an independent prognostic factor for progression-free survival (hazard ratio, 6.27, 95% confidence interval, 1.83–21.47, P = 0.003). Additionally, higher lactate dehydrogenase levels, multiple cardiovascular risk factors, and prior thrombosis were identified as unfavorable predictors of overall survival.
Conclusion
These findings suggest that patients with HU-R face a higher risk of hematological transformation, but have a comparable risk of thrombosis to patients with HU intolerance. These distinctions should guide decisions on second-line treatment options and clinical trials involving these patients.
Keyword
Figure
Reference
-
1. Vannucchi AM. Insights into the pathogenesis and management of thrombosis in polycythemia vera and essential thrombocythemia. Intern Emerg Med. 2010; 5(3):177–184. PMID: 19789961.2. Arber DA, Orazi A, Hasserjian R, Thiele J, Borowitz MJ, Le Beau MM, et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016; 127(20):2391–2405. PMID: 27069254.3. Moulard O, Mehta J, Fryzek J, Olivares R, Iqbal U, Mesa RA. Epidemiology of myelofibrosis, essential thrombocythemia, and polycythemia vera in the European Union. Eur J Haematol. 2014; 92(4):289–297. PMID: 24372927.4. Tefferi A. Novel mutations and their functional and clinical relevance in myeloproliferative neoplasms: JAK2, MPL, TET2, ASXL1, CBL, IDH and IKZF1. Leukemia. 2010; 24(6):1128–1138. PMID: 20428194.5. Tefferi A, Rumi E, Finazzi G, Gisslinger H, Vannucchi AM, Rodeghiero F, et al. Survival and prognosis among 1545 patients with contemporary polycythemia vera: an international study. Leukemia. 2013; 27(9):1874–1881. PMID: 23739289.6. Marchioli R, Finazzi G, Landolfi R, Kutti J, Gisslinger H, Patrono C, et al. Vascular and neoplastic risk in a large cohort of patients with polycythemia vera. J Clin Oncol. 2005; 23(10):2224–2232. PMID: 15710945.7. Cerquozzi S, Tefferi A. Blast transformation and fibrotic progression in polycythemia vera and essential thrombocythemia: a literature review of incidence and risk factors. Blood Cancer J. 2015; 5(11):e366. PMID: 26565403.8. Finazzi G, Barbui T. Evidence and expertise in the management of polycythemia vera and essential thrombocythemia. Leukemia. 2008; 22(8):1494–1502. PMID: 18596737.9. Marchetti M, Vannucchi AM, Griesshammer M, Harrison C, Koschmieder S, Gisslinger H, et al. Appropriate management of polycythaemia vera with cytoreductive drug therapy: European LeukemiaNet 2021 recommendations. Lancet Haematol. 2022; 9(4):e301–e311. PMID: 35358444.10. Tefferi A, Vannucchi AM, Barbui T. Polycythemia vera: historical oversights, diagnostic details, and therapeutic views. Leukemia. 2021; 35(12):3339–3351. PMID: 34480106.11. Antonioli E, Guglielmelli P, Pieri L, Finazzi M, Rumi E, Martinelli V, et al. Hydroxyurea-related toxicity in 3,411 patients with Ph’-negative MPN. Am J Hematol. 2012; 87(5):552–554. PMID: 22473827.12. Alvarez-Larrán A, Pereira A, Cervantes F, Arellano-Rodrigo E, Hernández-Boluda JC, Ferrer-Marín F, et al. Assessment and prognostic value of the European LeukemiaNet criteria for clinicohematologic response, resistance, and intolerance to hydroxyurea in polycythemia vera. Blood. 2012; 119(6):1363–1369. PMID: 22160617.13. Alvarez-Larrán A, Kerguelen A, Hernández-Boluda JC, Pérez-Encinas M, Ferrer-Marín F, Bárez A, et al. Frequency and prognostic value of resistance/intolerance to hydroxycarbamide in 890 patients with polycythaemia vera. Br J Haematol. 2016; 172(5):786–793. PMID: 26898196.14. Parasuraman S, DiBonaventura M, Reith K, Naim A, Concialdi K, Sarlis NJ. Patterns of hydroxyurea use and clinical outcomes among patients with polycythemia vera in real-world clinical practice: a chart review. Exp Hematol Oncol. 2016; 5(1):3. PMID: 26839736.15. Vannucchi AM, Kiladjian JJ, Griesshammer M, Masszi T, Durrant S, Passamonti F, et al. Ruxolitinib versus standard therapy for the treatment of polycythemia vera. N Engl J Med. 2015; 372(5):426–435. PMID: 25629741.16. Barosi G, Birgegard G, Finazzi G, Griesshammer M, Harrison C, Hasselbalch H, et al. A unified definition of clinical resistance and intolerance to hydroxycarbamide in polycythaemia vera and primary myelofibrosis: results of a European LeukemiaNet (ELN) consensus process. Br J Haematol. 2010; 148(6):961–963. PMID: 19930182.17. Schulman S, Kearon C. Subcommittee on Control of Anticoagulation of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost. 2005; 3(4):692–694. PMID: 15842354.18. Barbui T, Barosi G, Birgegard G, Cervantes F, Finazzi G, Griesshammer M, et al. Philadelphia-negative classical myeloproliferative neoplasms: critical concepts and management recommendations from European LeukemiaNet. J Clin Oncol. 2011; 29(6):761–770. PMID: 21205761.19. Marchioli R, Finazzi G, Specchia G, Cacciola R, Cavazzina R, Cilloni D, et al. Cardiovascular events and intensity of treatment in polycythemia vera. N Engl J Med. 2013; 368(1):22–33. PMID: 23216616.20. Alvarez-Larrán A, Díaz-González A, Such E, Mora E, Andrade-Campos M, García-Hernández C, et al. Genomic characterization of patients with polycythemia vera developing resistance to hydroxyurea. Leukemia. 2021; 35(2):623–627. PMID: 32372025.21. Tefferi A, Barraco D, Cerquozzi S, Lasho TL, Hanson CA, Ketterling RP, et al. Identification of serum lactate dehydrogenase (LDH) as an independent prognostic biomarker in polycythemia vera. Blood. 2016; 128(22):3111.22. Passamonti F, Griesshammer M, Palandri F, Egyed M, Benevolo G, Devos T, et al. Ruxolitinib for the treatment of inadequately controlled polycythaemia vera without splenomegaly (RESPONSE-2): a randomised, open-label, phase 3b study. Lancet Oncol. 2017; 18(1):88–99. PMID: 27916398.23. Demuynck T, Verhoef G, Delforge M, Vandenberghe P, Devos T. Polycythemia vera and hydroxyurea resistance/intolerance: a monocentric retrospective analysis. Ann Hematol. 2019; 98(6):1421–1426. PMID: 30919072.24. McMullin MF, Wilkins BS, Harrison CN. Management of polycythaemia vera: a critical review of current data. Br J Haematol. 2016; 172(3):337–349. PMID: 26492433.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Squamous Cell Carcinoma Associated With Hydroxyurea Therapy
- A Case of Secondary Erythromelalgia Associated with Polycythemia Vera
- Rapidly Growing and Aggressive Cutaneous Squamous Cell Carcinomas in a Patient Treated with Ruxolitinib
- Advances in Treatment for Polycythemia Vera and Essential Thrombocythemia
- Concurrent IgA Nephropathy and Minimal Change Disease in a Patient with Polycythemia Vera: A Case Report