Anesth Pain Med.
2023 Oct;18(4):431-438. 10.17085/apm.23079.
The sniffing position facilitated easier light wand guided endotracheal intubation compared with the neutral position with chin-lift
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, National Medical Center, Seoul, Korea
- KMID: 2550924
- DOI: http://doi.org/10.17085/apm.23079
Abstract
- Background
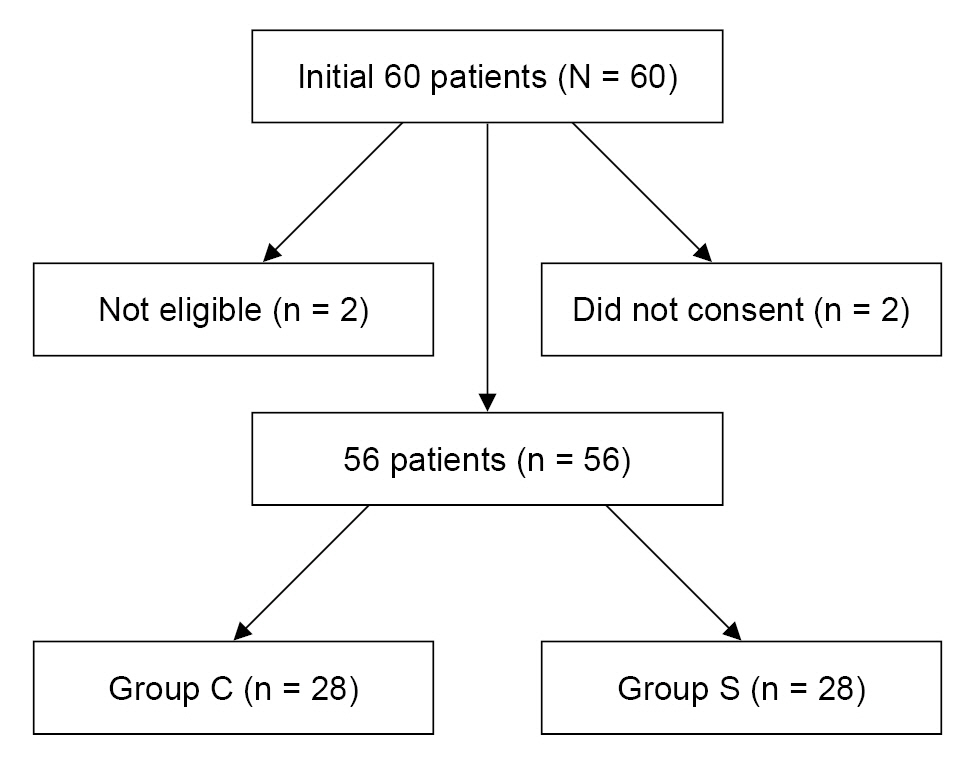
Traditionally, the patient's head is placed in a neutral position with a chin-lift to facilitate light wand guided endotracheal intubation. However, our study found that the sniffing position was more effective. In this study, we aimed to compare the two positions of light wand guided endotracheal intubation. Methods: Sixty adult patients were included in the study, after obtaining informed consent, and were randomly assigned to one of two groups: a control group in a neutral position with a chin-lift (group C, n = 30) and a sniffing position group (group S, n = 30). In group C, the anesthesiologist inserted a light wand after lifting the patient's mandible using the thumb of their non-dominant hand inside the patient's mouth. In group S, a light wand was inserted after the patient's head was flexed with the neck extended. We assessed variables such as light-search time, number of intubation attempts, time to achieve intubation, and side effects including blood tinge on the endotracheal tube, hoarseness, sore throat, and anesthesiologist satisfaction. Results: The light-search and intubation times were shorter in group S than in group C. The incidence of blood tinge on the endotracheal tube was higher in group C than in group S. Anesthesiologist satisfaction was higher in group S than in group C. Conclusions: The sniffing position was more effective in facilitating light wand guided endotracheal intubation than the neutral position with a chin-lift.
Keyword
Figure
Reference
-
1. Lin CP, Su CF, Lin WY, Jan JY, Jeng CS, Lin FS, et al. Modified lightwand intubation in a child with spondyloepiphyseal dysplasia congenita. Acta Anesthesiol Taiwan. 2011; 49:66–8.
Article2. Xue FS, Yang QY, Lio X, He N, Liu HP. Lightwand guided intubation in paediatric patients with a known difficult airway: a report of four cases. Anaesthesia. 2008; 63:520–5.
Article3. Davis L, Cook-Sather SD, Schreiner MS. Lighted stylet tracheal intubation: a review. Anesth Analg. 2000; 90:745–56.
Article4. Yon JH, Jo JK, Kwon YS, Park HG, Lee SS. Effect-site concentration of remifentanil for blunting hemodynamic responses to tracheal intubation using lightwand during target controlled infusion-total intravenous anesthesia. Korean J Anesthesiol. 2011; 60:398–402.
Article5. Kim JM, Im KS, Lee JM, Ro JH, Yoo KY, Kim JB. Relevance of radiological and clinical measurements in predicting difficult intubation using light wand (Surch-lite™) in adult patients. J Int Med Res. 2016; 44:136–46.
Article6. Han JU, Cho SY, Jeon WJ, Yeom JH, Shin WJ, Shim JH, et al. The optimal effect-site concentration of remifentanil for lightwand tracheal intubation during propofol induction without muscle relaxation. J Clin Anesth. 2011; 23:379–83.
Article7. Graham DH. Lightwand intubation using the Trachlight: a brief review of current knowledge. Can J Anaesth. 2001; 48:1169–70.
Article8. Byun SJ, Lee JH, Kim EJ, Lee SG, Ban JS, Min BW. The comparison of success rates of lightwand faciliated tracheal intubation in different head positions (neutral position versus sniffing position). Korean J Anesthesiol. 2006; 51:308–11.
Article9. Suh JK, Kim NW, Jeon WJ, Yeom JH, Shin WJ, Kim KH, et al. Randomized study comparing the sniffing position with the neutral position for lightwand intubation. Korean J Anesthesiol. 2008; 54:25–9.
Article10. Agrò F, Hung OR, Cataldo R, Carassiti M, Gherardi S. Lightwand intubation using the Trachlight: a brief review of current knowledge. Can J Anaesth. 2001; 48:592–9.
Article11. Kim JS, Seo DK, Lee CJ, Jung HS, Kim SS. Difficult intubation using intubating laryngeal mask airway in conjunction with a fiber optic bronchoscope. J Dent Anesth Pain Med. 2015; 15:167–71.
Article12. Jeon YT, Lim YJ, Na HS, Park SH, Oh AY, Hwang JW, et al. A double bending lightwand can provide more successful endotracheal intubation in patients with a short thyromental distance: a prospective randomised study. Eur J Anesthesiol. 2011; 28:651–4.13. Asai T, Shingu K. Blind intubation using the Endotrol tube and a light wand. Can J Anaesth. 2000; 47:478–9.
Article14. Lee HC, Yun MJ, Hwang JW, Na HS, Kim DH, Park JY. Higher operating tables provide better laryngeal views for tracheal intubation. Br J Anaesth. 2014; 112:749–55.
Article15. Akihisa Y, Hoshijima H, Maruyama K, Koyama Y, Andoh T. Effects of sniffing position for tracheal intubation: a meta-analysis of randomized controlled trials. Am J Emerg Med. 2015; 33:1606–11.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Comparison of Suceess Rates of Lightwand Facilitated Tracheal Intubation in Different Head Positions (Neutral Position versus Sniffing Position)
- Randomized Study Comparing the Sniffing Position with the Neutral Position for Lightwand Intubation
- Comparison of the rate of successful endotracheal intubation between the "sniffing" and "ramped" positions in patients with an expected difficult intubation: a prospective randomized study
- Ramped versus sniffing position in the videolaryngoscopy-guided tracheal intubation of morbidly obese patients: a prospective randomized study
- The Effect of Head Position on Tracheal Intubation using a Lightwand