Anesth Pain Med.
2023 Oct;18(4):406-413. 10.17085/apm.23064.
Comparison of pain relief of the cervical radiculopathy between high thoracic erector spinae plane block and cervical epidural injection
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Keimyung University Dongsan Hospital, Daegu, Korea
- KMID: 2550921
- DOI: http://doi.org/10.17085/apm.23064
Abstract
- Background
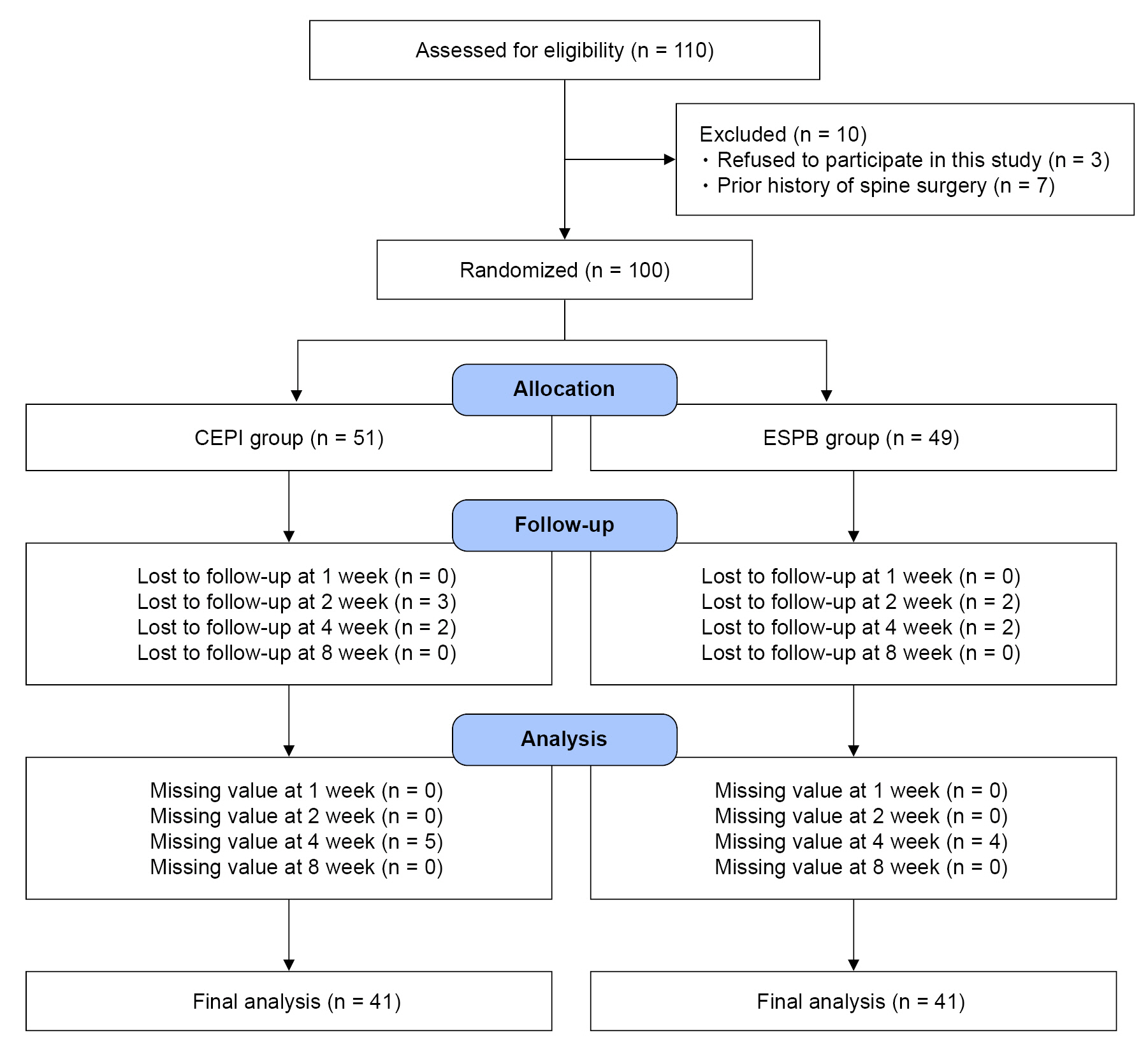
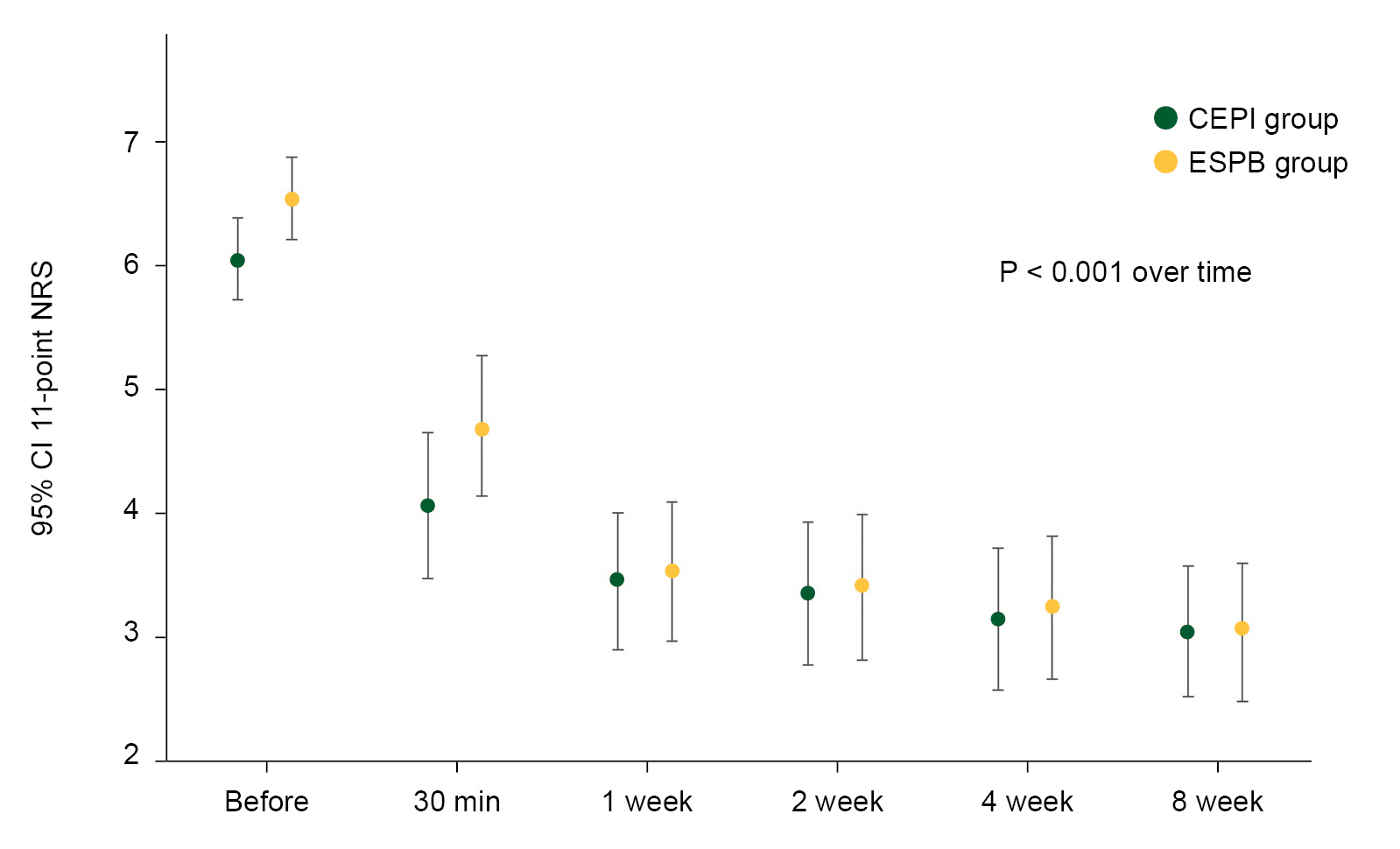
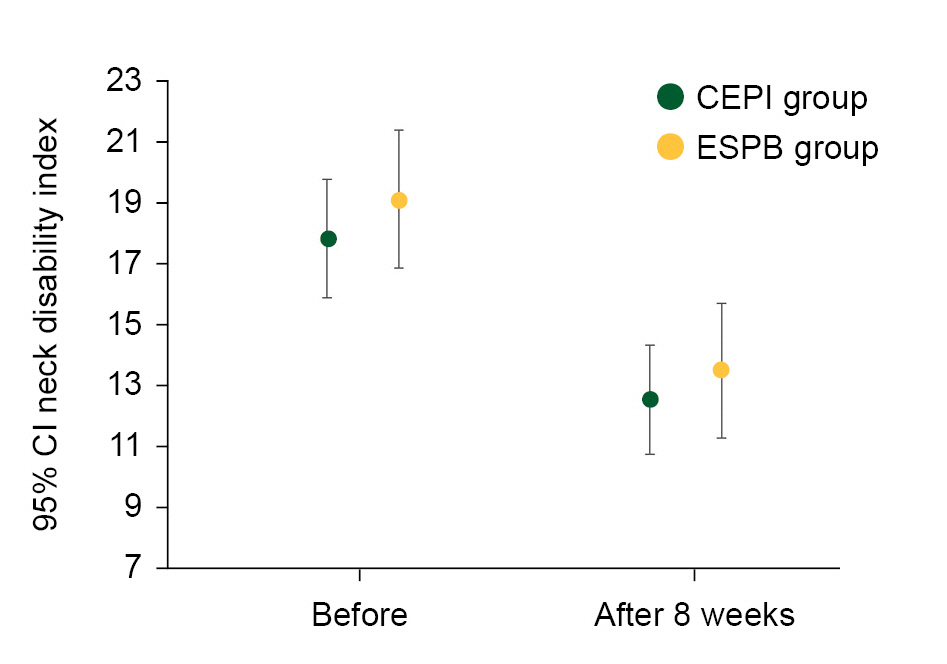
The high thoracic erector spinae plane block (ESPB) has been used for the management of chronic shoulder pain or arthroscopic shoulder surgery. No study has evaluated the analgesic efficacy of ESPB in patients with cervical radiculopathy although it is a favored and easy technique compared to neuraxial block. The purpose of this study was to compare the treatment outcome of cervical radiculopathy using high thoracic ESPB or cervical interlaminar epidural injection (CEPI). Methods: This study included 82 patients with neck and arm pain who received CEPI (CEPI group) using 4 ml of 0.1% ropivacaine or high thoracic ipsilateral ESPB (ESPB group) at the T2 or T3 level using 20 ml of 0.1% ropivacaine 20 ml. The degree of pain relief and disability were assessed using an 11-point numerical scale (NRS) and neck disability index (NDI), respectively. Results: The CEPI and ESPB groups demonstrated an equal number of patients with excellent pain relief (NRS reduction ≥ 50%). Significant reduction of NRS was found in both groups, and the effect of time was statistically significant in the groups (P < 0.001). The number of patients who showed an excellent improvement in NDI (NDI reduction ≥ 30%) was 20 (48.8%) and 22 (53.7%) in the CEPI and ESPB groups, respectively. Conclusions: Both the CEPI and ESPB demonstrated significant relief in neck and arm pain with improvement in disability.
Keyword
Figure
Reference
-
1. Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae plane block: a novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016; 41:621–7.2. Kot P, Rodriguez P, Granell M, Cano B, Rovira L, Morales J, et al. The erector spinae plane block: a narrative review. Korean J Anesthesiol. 2019; 72:209–20.
Article3. Altıparmak B, Korkmaz Toker M, Uysal AI, Kuşçu Y, Gümüş Demirbilek S. Ultrasound-guided erector spinae plane block versus oblique subcostal transversus abdominis plane block for postoperative analgesia of adult patients undergoing laparoscopic cholecystectomy: randomized, controlled trial. J Clin Anesth. 2019; 57:31–6.
Article4. Wang Q, Zhang G, Wei S, He Z, Sun L, Zheng H. Comparison of the Effects of Ultrasound-guided Erector Spinae Plane Block and Wound Infiltration on Perioperative Opioid Consumption and Postoperative Pain in Thoracotomy. J Coll Physicians Surg Pak. 2019; 29:1138–43.
Article5. Park S, Park J, Choi JW, Bang YJ, Oh EJ, Park J, et al. The efficacy of ultrasound-guided erector spinae plane block after mastectomy and immediate breast reconstruction with a tissue expander: a randomized clinical trial. Korean J Pain. 2021; 34:106–13.
Article6. Hong B, Bang S, Chung W, Yoo S, Chung J, Kim S. Multimodal analgesia with multiple intermittent doses of erector spinae plane block through a catheter after total mastectomy: a retrospective observational study. Korean J Pain. 2019; 32:206–14.
Article7. Liang X, Zhou W, Fan Y. Erector spinae plane block for spinal surgery: a systematic review and meta-analysis. Korean J Pain. 2021; 34:487–500.
Article8. Jeong H, Choi JW, Sim WS, Kim DK, Bang YJ, Park S, et al. Ultrasound-guided erector spinae plane block for pain management after gastrectomy: a randomized, single-blinded, controlled trial. Korean J Pain. 2022; 35:303–10.
Article9. Mahmoud AM, Ragab SG, Shawky MA, Masry DH, Botros JM. The efficacy of erector spinae plane block compared with intrathecal morphine in postoperative analgesia in patients undergoing lumbar spine surgery: a double-blind prospective comparative study. Pain Physician. 2023; 26:149–59.10. Ciftci B, Ekinci M, Gölboyu BE, Kapukaya F, Atalay YO, Kuyucu E, et al. High thoracic erector spinae plane block for arthroscopic shoulder surgery: a randomized prospective double-blind study. Pain Med. 2021; 22:776–83.
Article11. Abdelhaleem NF, Abdelatiff SE, Abdel Naby SM. Comparison of erector spinae plane block at the level of the second thoracic vertebra with suprascapular nerve block for postoperative analgesia in arthroscopic shoulder surgery. Pain Physician. 2022; 25:577–85.12. Dautzenberg KHW, Zegers MJ, Bleeker CP, Tan E, Vissers KCP, Van Geffen GJ, et al. Unpredictable injectate spread of the erector spinae plane block in human cadavers. Anesth Analg. 2019; 129:e163–6.
Article13. Restrepo-Garces CE, Urrego J, Mejia-Loaiza C, Giraldo L. The erector spinae plane block for radicular pain during pregnancy. Int J Obstet Anesth. 2019; 39:143–4.
Article14. Lee JH, Lee Y, Park HS, Lee JH. Comparison of clinical efficacy of transforaminal and interlaminar epidural steroid injection in radicular pain due to cervical diseases: a systematic review and meta-analysis. Pain Physician. 2022; 25:E1351–66.15. Chang A, Wang D. Complications of fluoroscopically guided cervical interlaminar epidural steroid injections. Curr Pain Headache Rep. 2020; 24:63.
Article16. Kim WJ, Park HG, Park YH, Shin MR, Koo GH, Shin HY. Pneumocephalus during cervical transforaminal epidural steroid injections: a case report. Am J Phys Med Rehabil. 2015; 94:63–9.17. Farrar JT Jr, Young JP, LaMoreaux L, Werth JL, Poole MR. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001; 94:149–58.
Article18. Song KJ, Choi BW, Choi BR, Seo GB. Cross-cultural adaptation and validation of the Korean version of the neck disability index. Spine (Phila Pa 1976). 2010; 35:E1045–9.
Article19. Vernon H. The neck disability index: state-of-the-art, 1991-2008. J Manipulative Physiol Ther. 2008; 31:491–502.
Article20. Abbed KM, Coumans JV. Cervical radiculopathy: pathophysiology, presentation, and clinical evaluation. Neurosurgery. 2007; 60(1 Suppl 1):S28–34.21. Rajmohan N, Thiruvathtra J, Lobo RP, Nair SG. Erector spinae plane block: a new modality of pain relief in a difficult situation. Korean J Anesthesiol. 2021; 74:82–3.
Article22. Kaushal B, Chauhan S, Magoon R, Krishna NS, Saini K, Bhoi D, et al. Efficacy of bilateral erector spinae plane block in management of acute postoperative surgical pain after pediatric cardiac surgeries through a midline sternotomy. J Cardiothorac Vasc Anesth. 2020; 34:981–6.
Article23. Taketa Y, Irisawa Y, Fujitani T. Comparison of ultrasound-guided erector spinae plane block and thoracic paravertebral block for postoperative analgesia after video-assisted thoracic surgery: a randomized controlled non-inferiority clinical trial. Reg Anesth Pain Med. 2019; rapm-2019-100827.
Article24. Forero M, Rajarathinam M, Adhikary SD, Chin KJ. Erector spinae plane block for the management of chronic shoulder pain: a case report. Can J Anaesth. 2018; 65:288–93.
Article25. Kim JY, Yang S, Kim D, Park Y, Kim YH. Correlation between the extent of injectate spread and clinical outcomes in cervical interlaminar epidural injection. Pain Physician. 2022; 25:E1229–38.26. Landers MH. Spinal cord injury during attempted cervical interlaminar epidural injection of steroids. Pain Med. 2018; 19:652–7.
Article27. Amrhein TJ, Parivash SN, Gray L, Kranz PG. Incidence of inadvertent dural puncture during CT fluoroscopy-guided interlaminar epidural corticosteroid injections in the cervical spine: an analysis of 974 cases. AJR Am J Roentgenol. 2017; 209:656–61.
Article28. Carette S, Leclaire R, Marcoux S, Morin F, Blaise GA, St-Pierre A, et al. Epidural corticosteroid injections for sciatica due to herniated nucleus pulposus. N Engl J Med. 1997; 336:1634–40.
Article29. Friedly JL, Comstock BA, Turner JA, Heagerty PJ, Deyo RA, Sullivan SD, et al. A randomized trial of epidural glucocorticoid injections for spinal stenosis. N Engl J Med. 2014; 371:11–21.
Article30. Yawata S, Imamachi N, Sakura S, Yamamoto H, Saito Y. Local anesthetic systemic toxicity of levobupivacaine in erector spinae plane block. Korean J Anesthesiol. 2021; 74:271–2.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Magnetic Resonance Imaging Images of the Local Anesthetic Spreading after Erector Spinae Plane Block at T2 Level
- Analgesic Effect of Erector Spinae Plane Block at T2 Level in Arm Surgery
- Comparison of Pain Relief and Spread Level Using Two Volumes of High Thoracic Erector Spinae Plane Block: A Prospective Randomized Study
- Erector Spinae Plane Block in Patients with Low Back Pain
- Anatomical classification and clinical application of thoracic paraspinal blocks