Anesth Pain Med.
2023 Oct;18(4):349-356. 10.17085/apm.23031.
Spinal anesthesia in elective lumbar spinal surgery
- Affiliations
-
- 1Department of Neurosurgery, Tufts Medical Center, Boston, MA, USA
- 2Department of Anesthesiology, Tufts Medical Center, Boston, MA, USA
- KMID: 2550914
- DOI: http://doi.org/10.17085/apm.23031
Abstract
- Spinal anesthesia (SA) is gaining recognition as a safe and efficacious regional alternative to general anesthesia for elective lumbar surgery. However, unfamiliarity with management issues related to its use has limited the adoption of awake spine surgery, despite its benefits. Few centers in the United States routinely offer SA for elective lumbar surgery, and a comprehensive workflow to standardize SA for lumbar surgery is lacking. In this article, we examine recent literature on the use of SA in lumbar surgery, review the experience of our institution with SA in lumbar surgery, and provide a cohesive outline to streamline the implementation of SA from the perspective of the anesthesiologist. We review the critical features of SA in contemporary lumbar surgery, including selection of patients, methods of SA, intraoperative sedation, and management of several important technical considerations. We aimed to flatten the learning curve to improve the availability and accessibility of the technique for eligible patients.
Keyword
Figure
Reference
-
1. Deyo RA, Mirza SK, Martin BI, Kreuter W, Goodman DC, Jarvik JG. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA. 2010; 303:1259–65.2. Dietz N, Sharma M, Adams S, Alhourani A, Ugiliweneza B, Wang D, et al. Enhanced recovery after surgery (ERAS) for spine surgery: a systematic review. World Neurosurg. 2019; 130:415–26.3. Hernandez NS, Rogers JL, Pham MH. Brachioradial pruritus caused by cervical disc herniation precipitated by trauma treated with anterior cervical discectomy and fusion: report of two cases and review of the literature. Asian J Neurosurg 2003. doi: 10.1055/s-0043-1772760. [Epub ahead of print].4. De Biase G, Gruenbaum SE, West JL, Chen S, Bojaxhi E, Kryzanski J, et al. Spinal versus general anesthesia for minimally invasive transforaminal lumbar interbody fusion: implications on operating room time, pain, and ambulation. Neurosurg Focus. 2021; 51:E3.
Article5. Olmos M, Hernandez NS, Kanter M, Liu P, Riesenburger RI, Kryzanski J. Periprocedural polypharmacy in lumbar fusions performed under spinal anesthesia compared with general anesthesia. Neurosurgery. 2023; 92:632–8.
Article6. Hernandez NS, Wang AY, Kanter M, Olmos M, Ahsan T, Liu P, et al. Assessing the impact of spinal versus general anesthesia on postoperative urinary retention in elective spinal surgery patients. Clin Neurol Neurosurg. 2022; 222:107454.
Article7. Brouwer TA, Van Roon EN, Rosier P, Kalkman CJ, Veeger N. Postoperative urinary retention: risk factors, bladder filling rate and time to catheterization: an observational study as part of a randomized controlled trial. Perioper Med (Lond). 2021; 10:2.
Article8. Monk TG, Weldon BC, Garvan CW, Dede DE, Van der Aa MT, Heilman KM, et al. Predictors of cognitive dysfunction after major noncardiac surgery. Anesthesiology. 2008; 108:18–30.
Article9. Weinstein SM, Poultsides L, Baaklini LR, Mörwald EE, Cozowicz C, Saleh JN, et al. Postoperative delirium in total knee and hip arthroplasty patients: a study of perioperative modifiable risk factors. Br J Anaesth. 2018; 120:999–1008.
Article10. West JL, De Biase G, Bydon M, Bojaxhi E, Mendhi M, Quiñones-Hinojosa A, et al. What is the learning curve for lumbar spine surgery under spinal anesthesia? World Neurosurg. 2022; 158:e310–e6.
Article11. Stewart J, Gasanova I, Joshi GP. Spinal anesthesia for ambulatory surgery: current controversies and concerns. Curr Opin Anaesthesiol. 2020; 33:746–52.
Article12. Rattenberry W, Hertling A, Erskine R. Spinal anaesthesia for ambulatory surgery. BJA Educ. 2019; 19:321–8.
Article13. Nolte H, Schikor K, Gergs P, Meyer J, Stark P. [On spinal anaesthesia with isobaric bupivacaine 0,5% (author's transl)]. Anaesthesist. 1977; 26:33–7. German.14. Uppal V, Retter S, Shanthanna H, Prabhakar C, McKeen DM. Hyperbaric versus isobaric bupivacaine for spinal anesthesia: systematic review and meta-analysis for adult patients undergoing noncesarean delivery surgery. Anesth Analg. 2017; 125:1627–37.
Article15. Schnider TW, Minto CF, Bruckert H, Mandema JW. Population pharmacodynamic modeling and covariate detection for central neural blockade. Anesthesiology. 1996; 85:502–12.
Article16. De Cassai A, Geraldini F, Boscolo A, Pasin L, Pettenuzzo T, Persona P, et al. General Anesthesia Compared to Spinal Anesthesia for Patients Undergoing Lumbar Vertebral Surgery: A Meta-Analysis of Randomized Controlled Trials. J Clin Med. 2020; 10:102.
Article17. Perez-Roman RJ, Govindarajan V, Bryant JP, Wang MY. Spinal anesthesia in awake surgical procedures of the lumbar spine: a systematic review and meta-analysis of 3709 patients. Neurosurg Focus. 2021; 51:E7.
Article18. Waguia R, Touko EK, Sykes DAW, Kelly-Hedrick M, Hijji FY, Sharan AD, et al. How to start an awake spine program: Protocol and illustrative cases. IBRO Neurosci Rep. 2022; 13:69–77.
Article19. Zhang N, He L, Ni JX. Level of sensory block after spinal anesthesia as a predictor of hypotension in parturient. Medicine (Baltimore). 2017; 96:e7184.
Article20. Białowolska K, Horosz B, Sękowska A, Malec-Milewska M. Fixed dose versus height-adjusted conventional dose of intrathecal hyperbaric bupivacaine for caesarean delivery: a prospective, double-blinded randomised trial. J Clin Med. 2020; 9:3600.
Article21. Sng BL, Han NLR, Leong WL, Sultana R, Siddiqui FJ, Assam PN, et al. Hyperbaric vs. isobaric bupivacaine for spinal anaesthesia for elective caesarean section: a Cochrane systematic review. Anaesthesia. 2018; 73:499–511.
Article22. Helmi M, Uyun Y, Suwondo BS, Widodo U. Comparison of intrathecal use of isobaric and hyperbaric bupivacaine during lower abdomen surgery. Journal of Anesthesiology. 2014; 2014:141324.
Article23. Tecklenburg-Weier E, Quest F, Nolte H, Meyer J. [The effect of patient positioning on the spread of sensory blockade in hyperbaric and isobaric spinal anesthesia using bupivacaine]. Reg Anaesth. 1990; 13:163–7. German.24. Russell IF. Posture and isobaric subarachnoid anaesthesia. The influence on spread of spinal anaesthesia with 'isobaric' 0.5% bupivacaine plain. Anaesthesia. 1984; 39:865–7.25. Hocking G, Wildsmith JA. Intrathecal drug spread. Br J Anaesth. 2004; 93:568–78.
Article26. Stienstra R, Van Poorten F. Speed of injection does not affect subarachnoid distribution of plain bupivacaine 0.5%. Reg Anesth. 1990; 15:208–10.27. Mancuso CA, Duculan R, Cammisa FP, Sama AA, Hughes AP, Lebl DR, et al. Concordance Between Patients' and Surgeons' Expectations of Lumbar Surgery. Spine (Phila Pa 1976). 2021; 46:249–58.
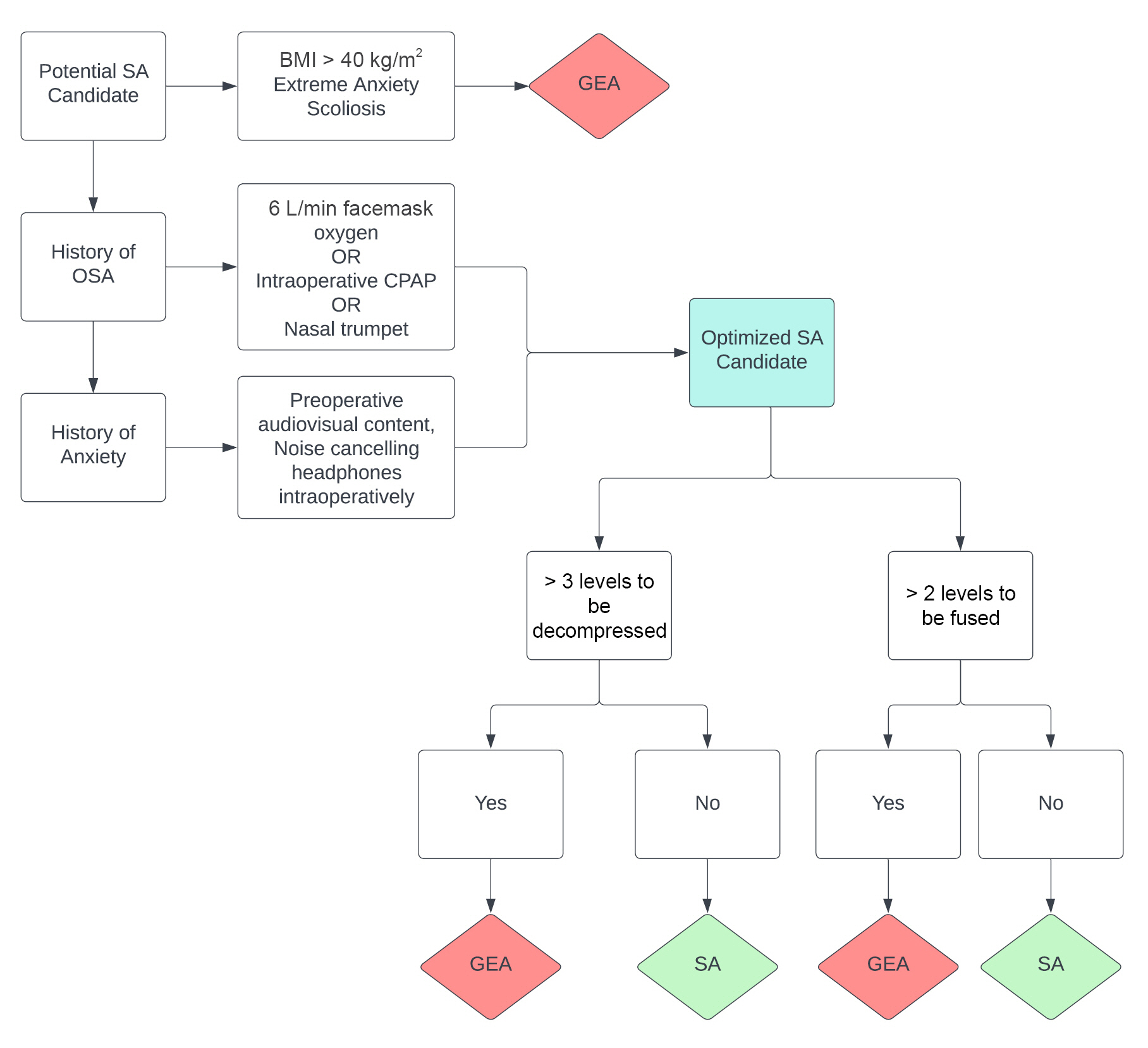
Article28. Letchuman V, Agarwal N, Mummaneni VP, Wang MY, Shabani S, Patel A, et al. Awake spinal surgery: simplifying the learning curve with a patient selection algorithm. Neurosurg Focus. 2021; 51:E2.
Article29. Ko JY, Leffert LR. Clinical implications of neuraxial anesthesia in the parturient with scoliosis. Anesth Analg. 2009; 109:1930–4.
Article30. Tharion JG, Kale S. Patient satisfaction through an immersive experience using a Mobile Phone-Based Head-Mounted Display During Arthroscopic Knee Surgery Under spinal anesthesia: a randomized clinical trial. Anesth Analg. 2021; 133:940–8.
Article31. Lamon AM, Einhorn LM, Cooter M, Habib AS. The impact of body mass index on the risk of high spinal block in parturients undergoing cesarean delivery: a retrospective cohort study. J Anesth. 2017; 31:552–8.
Article32. Lim H, Oh M, Chung YH, Ki H, Lee JJ. Effects of continuous positive airway pressure in patients at high risk of obstructive sleep apnea during propofol sedation after spinal anesthesia. J Clin Monit Comput. 2019; 33:657–63.
Article33. Practice guidelines for moderate procedural sedation and analgesia 2018: a report by the American Society of Anesthesiologists Task Force on Moderate Procedural Sedation and Analgesia, the American Association of Oral and Maxillofacial Surgeons, American College of Radiology, American Dental Association, American Society of Dentist Anesthesiologists, and Society of Interventional Radiology. Anesthesiology. 2018; 28:437–79.34. Arain SR, Ebert TJ. The Efficacy, Side effects, and recovery characteristics of dexmedetomidine versus propofol when used for intraoperative sedation. Anesth Analg. 2002; 95:461–6.
Article35. Candiotti KA, Bergese SD, Bokesch PM, Feldman MA, Wisemandle W, Bekker AY, et al. Monitored anesthesia care with dexmedetomidine: a prospective, randomized, double-blind, multicenter trial. Anesth Analg. 2010; 110:47–56.
Article36. Shin HJ, Woo Nam S, Kim H, Yim S, Han SH, Hwang JW, et al. Postoperative delirium after dexmedetomidine versus propofol sedation in healthy older adults undergoing orthopedic lower limb surgery with spinal anesthesia: a randomized controlled trial. Anesthesiology. 2023; 138:164–71.37. Park JW, Kim EK, Lee HT, Park S, Do SH. The effects of propofol or dexmedetomidine sedation on postoperative recovery in elderly patients receiving lower limb surgery under spinal anesthesia: a retrospective propensity score-matched analysis. J Clin Med. 2021; 10:135.
Article38. Abdallah FW, Abrishami A, Brull R. The facilitatory effects of intravenous dexmedetomidine on the duration of spinal anesthesia: a systematic review and meta-analysis. Anesth Analg. 2013; 117:271–8.39. Jeong J, Jin SH, Kim DY, Cho S, Lee H, Han JI. Effects of various methods of dexmedetomidine administration for sedation in elderly patients undergoing spinal anesthesia: a randomized controlled study. Anesth Pain Med (Seoul). 2020; 15:297–304.
Article40. Zhao TY, Chen D, Sun H, Xu ZX, Lyu S, Wang T, et al. Moderate sedation with single-dose remimazolam tosilate in elderly male patients undergoing transurethral resection of the prostate with spinal anesthesia: a prospective, single-arm, single-centre clinical trial. BMC Anesthesiol. 2022; 22:247.
Article41. Kilpatrick GJ. Remimazolam: non-clinical and clinical profile of a new sedative/anesthetic agent. Front Pharmacol. 2021; 12:690875.
Article42. Kumar AR, Guilleminault C, Certal V, Li D, Capasso R, Camacho M. Nasopharyngeal airway stenting devices for obstructive sleep apnoea: a systematic review and meta-analysis. J Laryngol Otol. 2015; 129:2–10.
Article43. Apfelbaum JL, Hagberg CA, Connis RT, Abdelmalak BB, Agarkar M, Dutton RP, et al. 2022 American Society of Anesthesiologists Practice Guidelines for management of the fifficult airway. Anesthesiology. 2022; 136:31–81.
Article44. Olsen KS, Petersen JT, Pedersen NA, Rovsing L. Self-positioning followed by induction of anaesthesia and insertion of a laryngeal mask airway versus endotracheal intubation and subsequent positioning for spinal surgery in the prone position: a randomised clinical trial. Eur J Anaesthesiol. 2014; 31:259–65.45. Abrishami A, Zilberman P, Chung F. Brief review: airway rescue with insertion of laryngeal mask airway devices with patients in the prone position. Can J Anaesth. 2010; 57:1014–20.
Article46. Hung MH, Fan SZ, Lin CP, Hsu YC, Shih PY, Lee TS. Emergency airway management with fiberoptic intubation in the prone position with a fixed flexed neck. Anesth Analg. 2008; 107:1704–6.
Article47. Kramer DC, Lo JC, Gilad R, Jenkins A. Fiberoptic scope as a rescue device in an anesthetized patient in the prone position. Anesth Analg. 2007; 105:890.
Article48. Southerland WA, Tollinche LE, Shapiro FE. Decision aids: the role of the patient in perioperative safety. Int Anesthesiol Clin. 2019; 57:4–11.
Article49. Marcantonio ER, Juarez G, Goldman L, Mangione CM, Ludwig LE, Lind L, et al. The relationship of postoperative delirium with psychoactive medications. JAMA. 1994; 272:1518–22.
Article50. Breton JM, Ludwig CG, Yang MJ, Nail TJ, Riesenburger RI, Liu P, et al. Spinal anesthesia in contemporary and complex lumbar spine surgery: experience with 343 cases. J Neurosurg Spine. 2022; 36:534–41.
Article51. Kanter M, Hernandez NS, Olmos M, Karimi H, Riesenburger RI, Kryzanski JT. Intraoperative triggered electromyography for pedicle screw placement under spinal anesthesia: a preliminary report. Oper Neurosurg (Hagerstown). 2023; 24:651–5.
Article52. Yang MJ, Riesenburger RI, Kryzanski JT. The use of intra-operative navigation during complex lumbar spine surgery under spinal anesthesia. Clin Neurol Neurosurg. 2022; 215:107186.
Article53. Kathirvel S, Sadhasivam S, Saxena A, Kannan TR, Ganjoo P. Effects of intrathecal ketamine added to bupivacaine for spinal anaesthesia. Anaesthesia. 2000; 55:899–904.
Article54. Adhikari P, Subedi A, Sah BP, Pokharel K. Analgesic effects of intravenous ketamine after spinal anaesthesia for non-elective caesarean delivery: a randomised controlled trial. BMJ Open. 2021; 11:e044168.
Article55. Wang AY, Olmos M, Ahsan T, Kanter M, Liu P, Balonov K, et al. A second prone dose algorithm for patients undergoing spinal anesthesia during thoracolumbar surgeries. Oper Neurosurg (Hagerstown). 2023; 24:283–90.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Definition of lumbar spinal pain
- Efficiency of Spinal Anesthesia versus General Anesthesia for Minimal Invasive Single Level Transforaminal Lumbar Interbody Fusion: A Retrospective Analysis of 178 Patients
- Physiology of Total Spinal Anesthesia
- Nerve injury in an undiagnosed adult tethered cord syndrome patients following spinal anesthesia: A case report
- A Case of Coexisting Cervical and Lumbar Spinal Stenosis