Acute Crit Care.
2023 Nov;38(4):425-434. 10.4266/acc.2023.00773.
Healthcare-associated infections in critical COVID-19 patients in Tunis: epidemiology, risk factors, and outcomes
- Affiliations
-
- 1Medical Intensive Care Unit, La Rabta Hospital, Tunis, Tunisia
- KMID: 2550898
- DOI: http://doi.org/10.4266/acc.2023.00773
Abstract
- Background
Coronavirus disease 2019 (COVID-19) pandemic disrupted adherences to healthcare-associated infection (HAI) prevention protocols. Herein, we studied the characteristics of all HAIs occurring in critically ill COVID-19 patients.
Methods
A retrospective, single-center cohort of critical COVID-19 patients during 2021. Microbiological samples were collected if HAI was suspected. We analyzed all factors that could potentially induce HAI, using septic shock and mortality as endpoints.
Results
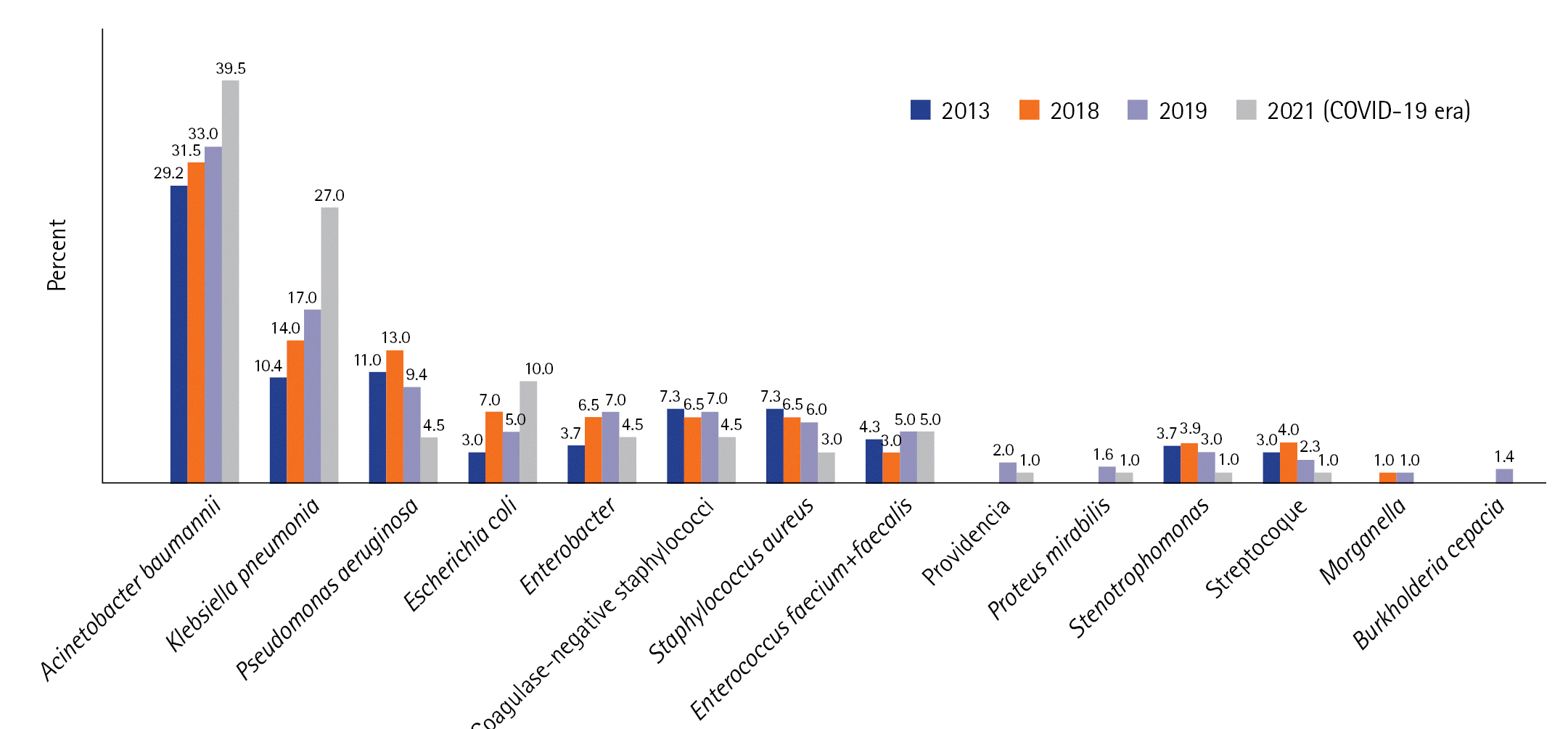
Sixty-four among 161 included patients (39.7%) presented a total of 117 HAIs with an incidence density of 69.2 per 1,000 hospitalization days. Compared to the prior COVID-19 period (2013–2019), the identification of HAI increased in 2021. HAIs were classified into ventilator-associated pneumonia (VAP; n=38), bloodstream infection (n=32), urinary tract infection (n=24), catheter-related infection (n=12), and fungal infection (n=11). All HAIs occurred significantly earlier in the post–COVID-19 period (VAP: 6 vs. 10 days, P=0.045, in 2017 and 2021). Acinetobacter baumannii (39.5%) and Klebsiella pneumoniae (27%) were the most commonly isolated pathogens that exhibited a multidrug-resistant (MDR) profile, observed in 89% and 64.5%, respectively. The HAI factors were laboratory abnormalities (odds ratio [OR], 6.4; 95% confidence interval [CI], 2.3–26.0), cumulative steroid dose (OR, 1.9; 95% CI, 1.3–4.0), and invasive procedures (OR, 20.7; 95% CI, 5.3–64.0). HAI was an independent factor of mortality (OR, 8.5; P=0.004).
Conclusions
During the COVID-19 era, the incidence of HAIs increased and MDR isolates remained frequent. A severe biological inflammatory syndrome, invasive devices, and elevated cumulative steroid dosages were related to HAIs. HAI was a significant death factor.
Figure
Reference
-
1. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020; 395:497–506.
Article2. Conway Morris A, Kohler K, De Corte T, Ercole A, De Grooth HJ, Elbers PW, et al. Co-infection and ICU-acquired infection in COIVD-19 ICU patients: a secondary analysis of the UNITE-COVID data set. Crit Care. 2022; 26:236.3. Despotovic A, Milosevic B, Milosevic I, Mitrovic N, Cirkovic A, Jovanovic S, et al. Hospital-acquired infections in the adult intensive care unit-Epidemiology, antimicrobial resistance patterns, and risk factors for acquisition and mortality. Am J Infect Control. 2020; 48:1211–5.
Article4. Barrasa H, Martín A, Maynar J, Rello J, Fernández-Torres M, Aguirre-Quiñonero A, et al. High rate of infections during ICU admission of patients with severe SARS-CoV-2 pneumonia: a matter of time? J Infect. 2021; 82:186–230.
Article5. Lansbury L, Lim B, Baskaran V, Lim WS. Co-infections in people with COVID-19: a systematic review and meta-analysis. J Infect. 2020; 81:266–75.
Article6. Contou D, Claudinon A, Pajot O, Micaëlo M, Longuet Flandre P, Dubert M, et al. Bacterial and viral co-infections in patients with severe SARS-CoV-2 pneumonia admitted to a French ICU. Ann Intensive Care. 2020; 10:119.
Article7. Hanson KE, Caliendo AM, Arias CA, Englund JA, Hayden MK, Lee MJ, et al. Infectious Diseases Society of America Guidelines on the Diagnosis of Coronavirus Disease 2019 (COVID-19): serologic testing. Clin Infect Dis. 2020; ciaa1343.
Article8. Trifi A, Abdellatif S, Oueslati M, Zribi M, Daly F, Nasri R, et al. Nosocomial infections: current situation in a resuscitation-unit. Tunis Med. 2017; 95:179–84.9. Schwendimann R, Blatter C, Dhaini S, Simon M, Ausserhofer D. The occurrence, types, consequences and preventability of in-hospital adverse events: a scoping review. BMC Health Serv Res. 2018; 18:521.10. World Health Organization. Patient safety fact file [Internet]. World Health Organization;2019. [cited 2023 Sep 1]. Available from: https://www.who.int/news-room/fact-sheets/detail/patient-safety.11. Haque M, Sartelli M, McKimm J, Abu Bakar M. Health care-associated infections: an overview. Infect Drug Resist. 2018; 11:2321–33.12. Peters A, Tartari E, Mai SH, Allegranzi B, Pittet D. 2019 WHO hand hygiene campaign and global survey: clean care for all-it's in your hands. Lancet Infect Dis. 2019; 19:463–4.
Article13. Saito H, Allegranzi B, Pittet D. 2018 WHO hand hygiene campaign: preventing sepsis in health care and the path to universal health coverage. Lancet Infect Dis. 2018; 18:490–2.
Article14. Roshan R, Feroz AS, Rafique Z, Virani N. Rigorous hand hygiene practices among health care workers reduce hospital-associated infections during the COVID-19 pandemic. J Prim Care Community Health. 2020; 11:2150132720943331.
Article15. Baccolini V, Migliara G, Isonne C, Dorelli B, Barone LC, Giannini D, et al. The impact of the COVID-19 pandemic on healthcare-associated infections in intensive care unit patients: a retrospective cohort study. Antimicrob Resist Infect Control. 2021; 10:87.
Article16. Petty LA, Flanders SA, Vaughn VM, Ratz D, O'Malley M, Malani AN, et al. Risk factors and outcomes associated with community-onset and hospital-acquired coinfection in patients hospitalized for coronavirus disease 2019 (COVID-19): a multihospital cohort study. Infect Control Hosp Epidemiol. 2022; 43:1184–93.
Article17. Somers EC, Eschenauer GA, Troost JP, Golob JL, Gandhi TN, Wang L, et al. Tocilizumab for treatment of mechanically ventilated patients with COVID-19. Clin Infect Dis. 2021; 73:e445–54.
Article18. He Y, Li W, Wang Z, Chen H, Tian L, Liu D. Nosocomial infection among patients with COVID-19: a retrospective data analysis of 918 cases from a single center in Wuhan, China. Infect Control Hosp Epidemiol. 2020; 41:982–3.
Article19. Soriano MC, Vaquero C, Ortiz-Fernández A, Caballero A, Blandino-Ortiz A, de Pablo R. Low incidence of co-infection, but high incidence of ICU-acquired infections in critically ill patients with COVID-19. J Infect. 2021; 82:e20–1.
Article20. Grasselli G, Scaravilli V, Mangioni D, Scudeller L, Alagna L, Bartoletti M, et al. Hospital-acquired infections in critically ill patients with COVID-19. Chest. 2021; 160:454–65.
Article21. Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review. JAMA. 2020; 324:782–93.
Article22. Luyt CE, Bouadma L, Morris AC, Dhanani JA, Kollef M, Lipman J, et al. Pulmonary infections complicating ARDS. Intensive Care Med. 2020; 46:2168–83.
Article23. Kokkoris S, Papachatzakis I, Gavrielatou E, Ntaidou T, Ischaki E, Malachias S, et al. ICU-acquired bloodstream infections in critically ill patients with COVID-19. J Hosp Infect. 2021; 107:95–7.
Article24. Falcone M, Tiseo G, Giordano C, Leonildi A, Menichini M, Vecchione A, et al. Predictors of hospital-acquired bacterial and fungal superinfections in COVID-19: a prospective observational study. J AntimicrobChemother. 2021; 76:1078–84.
Article25. Bardi T, Pintado V, Gomez-Rojo M, Escudero-Sanchez R, Azzam Lopez A, Diez-Remesal Y, et al. Nosocomial infections associated to COVID-19 in the intensive care unit: clinical characteristics and outcome. Eur J Clin Microbiol Infect Dis. 2021; 40:495–502.
Article26. Garcia-Vidal C, Sanjuan G, Moreno-García E, Puerta-Alcalde P, Garcia-Pouton N, Chumbita M, et al. Incidence of co-infections and superinfections in hospitalized patients with COVID-19: a retrospective cohort study. Clin Microbiol Infect. 2021; 27:83–8.
Article27. Cheng K, He M, Shu Q, Wu M, Chen C, Xue Y. Analysis of the risk factors for nosocomial bacterial infection in patients with COVID-19 in a tertiary hospital. Risk Manag Healthc Policy. 2020; 13:2593–9.28. Kyi M, Colman PG, Wraight PR, Reid J, Gorelik A, Galligan A, et al. Early intervention for diabetes in medical and surgical inpatients decreases hyperglycemia and hospital-acquired infections: a cluster randomized trial. Diabetes Care. 2019; 42:832–40.
Article29. Khaodhiar L, McCowen K, Bistrian B. Perioperative hyperglycemia, infection or risk? Curr Opin Clin Nutr Metab Care. 1999; 2:79–82.
Article30. Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020; 46:846–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Factors Affecting Fear of COVID-19 Infection in Healthcare Workers in COVID-19 Dedicated Teams: Focus on Professional Quality of Life
- The Pathologic Mechanisms and Epidemiology of Dysphagia Associated with COVID-19
- Clinical Effect of Hepatitis B Virus on COVID-19 Infected Patients: A Nationwide Population-Based Study Using the Health Insurance Review & Assessment Service Database
- Burnout among Healthcare Workers during COVID-19 Pandemic
- Risk factors for progressing to critical illness in patients with hospital-acquired COVID-19