Ann Clin Microbiol.
2023 Dec;26(4):103-115. 10.5145/ACM.2023.26.4.103.
Clinical usefulness of procalcitonin/albumin and blood urea nitrogen/albumin ratios for the early detection of bacteremia
- Affiliations
-
- 1Department of Biomedical Laboratory Science, Jungwon University, Goesan- gun, Chungbuk, Korea
- 2Department of Sleep Medicine Institute, Jungwon University, Goesan- gun, Chungbuk,
- 3Departments of Laboratory Medicine, Uijeongbu St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Uijeongbu, Korea
- 4Departments of Internal Medicine, Uijeongbu St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Uijeongbu, Korea
- KMID: 2550662
- DOI: http://doi.org/10.5145/ACM.2023.26.4.103
Abstract
- Background
Early prediction of bacteremia is important because sepsis may develop if bacteremia is not treated in time. We aimed to determine whether blood tests are clinically useful in predicting gram-negative versus gram-positive bacteremia.
Methods
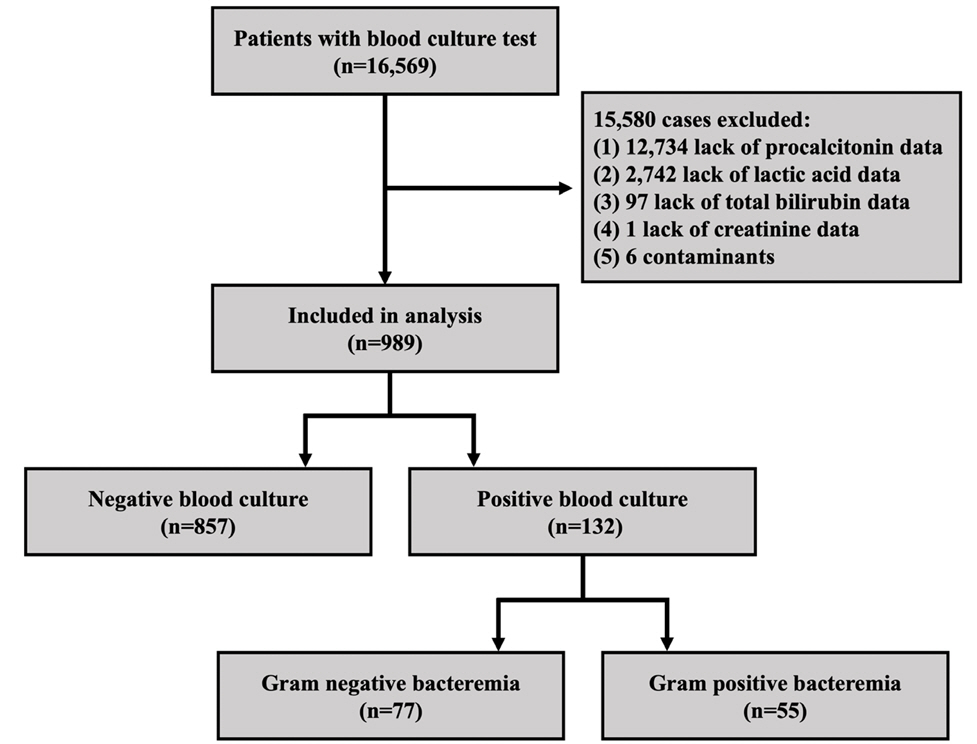
We retrospectively analyzed the medical records of 16,569 patients who underwent blood culture testing among those who visited St. Mary’s Hospital of Uijeongbu, Catholic University from January 1, 2018 to December 31, 2018. After excluding 15,580 patients with insufficient data for analysis, the total study population was 989.
Results
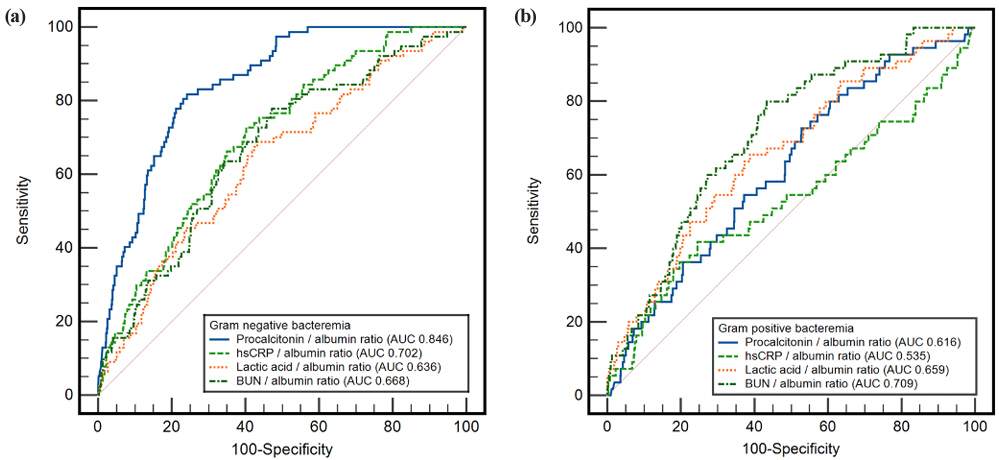
In the multivariable logistic regression analysis for gram-negative bacteremia, after adjusting for major variables, procalcitonin (odds ratio [OR] 1.02, P < 0.001), high-sensitivity C-reactive protein (OR 1.03, P = 0.010), and albumin (OR 0.55, P = 0.010) were significant. In the same model, lactic acid (OR 1.08, P = 0.010), blood urea nitrogen (BUN) (OR 1.02, P = 0.010), and albumin (OR 0.50, P = 0.005) were significant for gram-positive bacteremia. We constructed blood indicators by combining blood tests that were significant in multivariable logistic regression analysis. Comparing the area under the curve (AUC) of the receiver operating characteristic curve, the AUC of the procalcitonin/albumin ratio in gramnegative bacteremia was significantly higher than that of procalcitonin (0.846 vs. 0.837, P = 0.005), and the AUC of the BUN/albumin ratio in gram-positive bacteremia was significantly higher than that of BUN (0.709 vs. 0.679, P = 0.007).
Conclusion
The procalcitonin/albumin ratio is expected to be helpful in the early prediction of gram-negative bacteremia, whereas the BUN/albumin ratio in the early prediction of grampositive bacteremia.
Keyword
Figure
Reference
-
1. Smith DA and Nehring SM. Bacteremia. StatPearls. https://www.ncbi.nlm.nih.gov/books/ NBK441979/ [Online] (last visited on 6 November 2023).2. Fernández-Sarmiento J, Schlapbach LJ, Acevedo L, Santana CR, Acosta Y, Diana A, et al. Endothelial damage in sepsis: the importance of systems biology. Front Pediatr 2022;10:828968.3. Dugar S, Choudhary C, Duggal A. Sepsis and septic shock: guideline-based management. Cleve Clin J Med 2020;87:53-64.4. Uslan DZ, Crane SJ, Steckelberg JM, Cockerill FR, III, St. Sauver JL, Wilson WR, et al. Age- and sex-associated trends in bloodstream infection: a population-based study in olmsted county, minnesota. Arch Intern Med 2007;167:834-9.5. Søgaard M, Nørgaard M, Dethlefsen C, Schønheyder HC. Temporal changes in the incidence and 30-day mortality associated with bacteremia in hospitalized patients from 1992 through 2006: a population-based cohort study. Clin Infect Dis 2011;52:61-9.6. Doern GV, Carroll KC, Diekema DJ, Garey KW, Rupp ME, Weinstein MP, et al. Practical guidance for clinical microbiology laboratories: a comprehensive update on the problem of blood culture contamination and a discussion of methods for addressing the problem. Clin Microbiol Rev 2019;33:e00009-19.7. Lien F, Lin HS, Wu YT, Chiueh TS. Bacteremia detection from complete blood count and differential leukocyte count with machine learning: complementary and competitive with c-reactive protein and procalcitonin tests. BMC Infect Dis 2022;22:287.8. Colak A, Aksit MZ, Toprak B, Yılmaz N. Diagnostic values of neutrophil/lymphocyte ratio, platelet/lymphocyte ratio and procalcitonin in early diagnosis of bacteremia. Turk J Biochem 2020;45:57-64.9. Ljungström L, Pernestig AK, Jacobsson G, Andersson R, Usener B, Tilevik D. Diagnostic accuracy of procalcitonin, neutrophil-lymphocyte count ratio, C-reactive protein, and lactate in patients with suspected bacterial sepsis. PLoS One 2017;12:e0181704.10. Hoeboer SH, van der Geest PJ, Nieboer D, Groeneveld ABJ. The diagnostic accuracy of procalcitonin for bacteraemia: a systematic review and meta-analysis. Clin Microbiol Infect 2015;21:474-81.11. Markanday A. Acute phase reactants in infections: evidence-based review and a guide for clinicians. Open Forum Infect Dis 2015;2:ofv098.12. Wang H, Ran J, et al. Urea. In: Yang B and Sands J, eds. Urea transporters. Subcellular biochemistry. Dordrecht; Springer, 2014:7-29.13. Washio Y, Ito A, Kumagai S, Ishida T, Yamazaki A. A model for predicting bacteremia in patients with community-acquired pneumococcal pneumonia: a retrospective observational study. BMC Pulm Med 2018;18:24.14. Wiedermann CJ. Hypoalbuminemia as surrogate and culprit of infections. Int J Mol Sci 2021;22:4496.15. Gatta A, Verardo A, Bolognesi M. Hypoalbuminemia. Intern Emerg Med 2012;7:S193-9.16. Zou XL, Feng DY, Wu WB, Yang HL, Zhang TT. Blood urea nitrogen to serum albumin ratio independently predicts 30-day mortality and severity in patients with escherichia coli bacteraemia. Med Clin 2021;157:219-25.17. Güneş H, Yurttutan S, Çobanuşağı M, Doğaner A. CRP/albumin ratio: a promising marker of gram-negative bacteremia in late-onset neonatal sepsis. Turk Arch Pediatr 2021;56:32-6.18. DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 1988;44:837-45.19. Diekema DJ, Hsueh PR, Mendes RE, Pfaller MA, Rolston KV, Sader HS, et al. The microbiology of bloodstream infection: 20-year trends from the sentry antimicrobial surveillance program. Antimicrob Agents Chemother 2019;63:00355-19.20. Timsit JF, Ruppé E, Barbier F, Tabah A, Bassetti M. Bloodstream infections in critically ill patients: an expert statement. Intensive Care Med 2020;46:266-84.21. Huang TD, Melnik E, Bogaerts P, Evrard S, Glupczynski Y. Evaluation of the eplex blood culture identification panels for detection of pathogens in bloodstream infections. J Clin Microbiol 2019;57:01597-18.22. Berinson B, Both A, Berneking L, Christner M, Lütgehetmann M, Aepfelbacher M, et al. Usefulness of biofire filmarray bcid2 for blood culture processing in clinical practice. J Clin Microbiol 2021;59:e0054321.23. Scerbo MH, Kaplan HB, Dua A, Litwin DB, Ambrose CG, Moore LJ, et al. Beyond blood culture and gram stain analysis: a review of molecular techniques for the early detection of bacteremia in surgical patients. Surg Infect 2016;17:294-302.24. Blauwkamp TA, Thair S, Rosen MJ, Blair L, Lindner MS, Vilfan ID, et al. Analytical and clinical validation of a microbial cell-free DNA sequencing test for infectious disease. Nat Microbiol 2019;4:663-74.25. Jones AE, Fiechtl JF, Brown MD, Ballew JJ, Kline JA. Procalcitonin test in the diagnosis of bacteremia: a meta-analysis. Ann Emerg Med 2007;50:34-41.26. Li S, Rong H, Guo Q, Chen Y, Zhang G, Yang J. Serum procalcitonin levels distinguish gram-negative bacterial sepsis from gram-positive bacterial and fungal sepsis. J Res Med Sci 2016;21:39.27. Leli C, Ferranti M, Moretti A, Al Dhahab ZS, Cenci E, Mencacci A. Procalcitonin levels in gram-positive, gram-negative, and fungal bloodstream infections. Dis Markers 2015;2015:701480.28. Brodská H, Malíčková K, Adámková V, Benáková H, Šťastná MM, Zima T. Significantly higher procalcitonin levels could differentiate gram-negative sepsis from gram-positive and fungal sepsis. Clin Exp Med 2013;13:165-70.29. Wang D, Tao X, Guo W, Liu H, Cheng S, Wang J. The diagnostic ability of procalcitonin to differentiate gram-negative bacteria from gram-positive bacteria and fungal bloodstream infections in critically ill patients. Eur J Inflamm 2019;17:2058739219841469.30. Li T, Li X, Zhu Z, Liu X, Dong G, Xu Z, et al. Clinical value of procalcitonin-to-albumin ratio for identifying sepsis in neonates with pneumonia. Ann Med 2023;55:920-5.31. Higashikawa T, Okuro M, Ishigami K, Mae K, Sangen R, Mizuno T, et al. Procalcitonin and albumin as prognostic biomarkers in elderly patients with a risk of bacterial infection. J Int Med Res 2018;46:2606-14.32. Luo X, Yang X, Li J, Zou G, Lin Y, Qing G, et al. The procalcitonin/albumin ratio as an early diagnostic predictor in discriminating urosepsis from patients with febrile urinary tract infection. Medicine 2018;97:e11078.33. Çakırca TD, Çakırca G, Torun A, Bindal A, Üstünel M, Kaya A. Comparing the predictive values of procalcitonin/albumin ratio and other inflammatory markers in determining COVID-19 severity. Pak J Med Sci 2023;39:450-5.34. Küçükceran K, Ayrancı MK, Girişgin AS, Koçak S, Dündar ZD. The role of the bun/albumin ratio in predicting mortality in COVID-19 patients in the emergency department. Am J Emerg Med 2021;48:33-7.35. Milas GP, Issaris V, Papavasileiou V. Blood urea nitrogen to albumin ratio as a predictive factor for pneumonia: a meta-analysis. Respir Med Res 2022;81:100886.36. Dundar ZD, Kucukceran K, Ayranci MK. Blood urea nitrogen to albumin ratio is a predictor of in-hospital mortality in older emergency department patients. Am J Emerg Med 2021;46:34954.37. Peng X, Huang Y, Fu H, Zhang Z, He A, Luo R. Prognostic value of blood urea nitrogen to serum albumin ratio in intensive care unit patients with lung cancer. Int J Gen Med 2021;14:7349-59.38. Jeon JH and Park DW. Controversies regarding the new definition of sepsis. Korean J Med 2017;92:342-8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical relevance of blood urea nitrogen to serum albumin ratio for predicting bacteremia in very young children with febrile urinary tract infection
- Difference of Pertoneal Solute Transport in CAPD Patients with and without Diabetes Mellitus: Measurement by Personal Dialysis Capacity(PDC) Test
- Serum Levels of Protein, Urea Nitrogen, Uric Acid, Creatinine and Serum Amylase Activity in Normal School Children
- Predictive value of procalcitonin for bacteremia in patients with pneumonia in the emergency department
- Clinical Characteristics and Survival of Elderly Patient with Klebsiella pneumoniae Bacteremia in Emergency Room