Obstet Gynecol Sci.
2024 Jan;67(1):67-75. 10.5468/ogs.23048.
Clinical outcome after high dose rate intracavitary brachytherapy with traditional point ‘A’ dose prescription in locally advanced carcinoma of uterine cervix: dosimetric analysis from the perspective of computed tomography imaging-based 3-dimensional treatment planning
- Affiliations
-
- 1Department of Radiation Oncology, Burdwan Medical College, Purba Bardhaman, West Bengal, India
- 2Department of Cardiology, Burdwan Medical College, Purba Bardhaman, West Bengal, India
- 3Department of Radiation Oncology, Agartala Government Medical College, Agartala, India
- KMID: 2550487
- DOI: http://doi.org/10.5468/ogs.23048
Abstract
Objective
To analyze tumour response and toxicity with respect to cumulative radiotherapy dose to target and organs at risk (OARs) with computed tomography (CT)-based image guided adaptive brachytherapy planning for locally advanced carcinoma cervix.
Methods
Patients were treated with two-dimensional concurrent chemoradiotherapy to whole pelvis followed by intracavitary brachytherapy (ICBT) with dose prescription to point ‘A’. CT image-based delineation of high-risk clinical target volume (HR-CTV), urinary bladder, rectum and sigmoid colon was done with generation of dose-volume histogram (DVH) data and optimization of doses to target and OARs. Follow up assessments were done for response of disease and toxicity with generation of data for statistical analysis.
Results
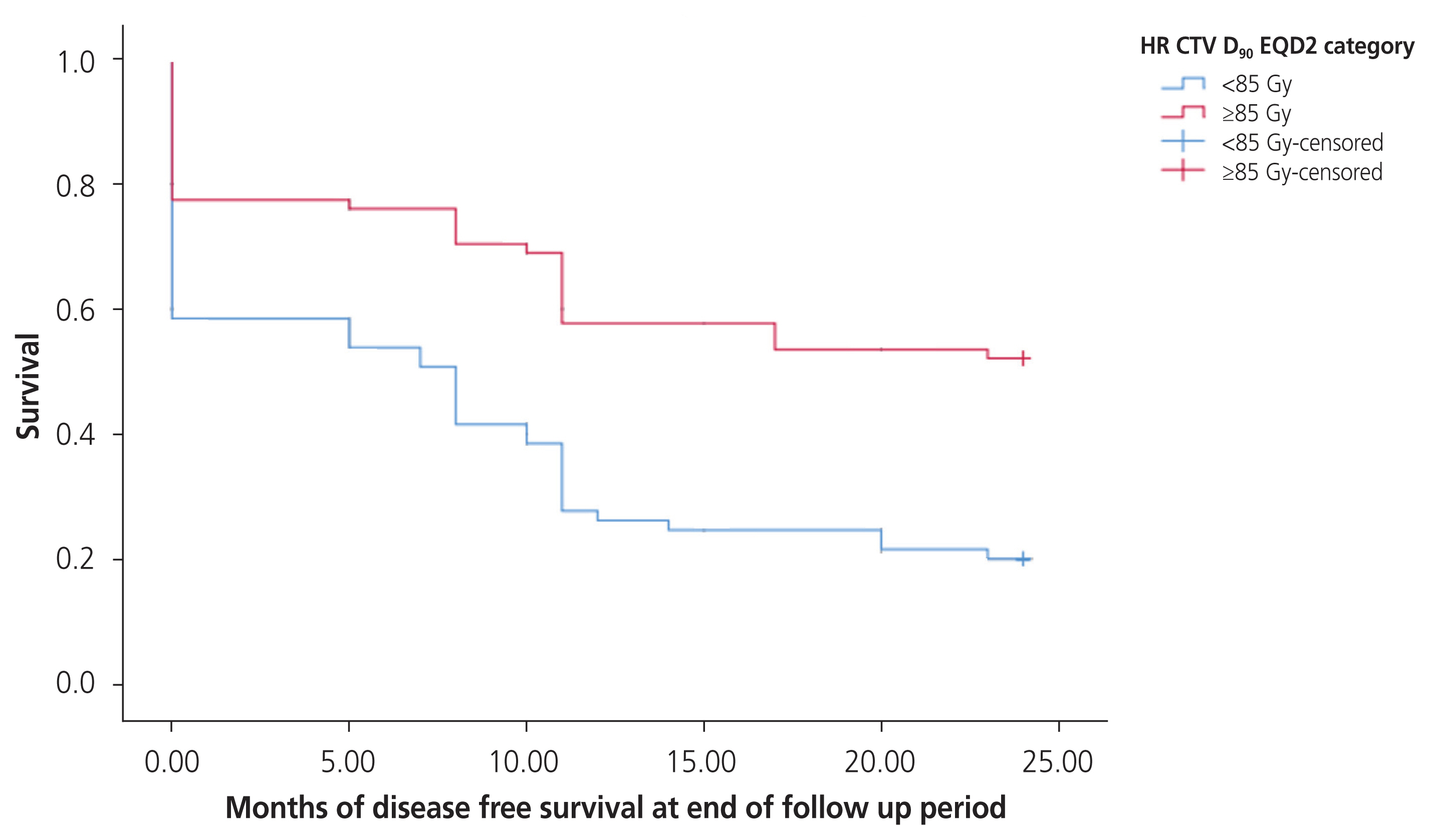
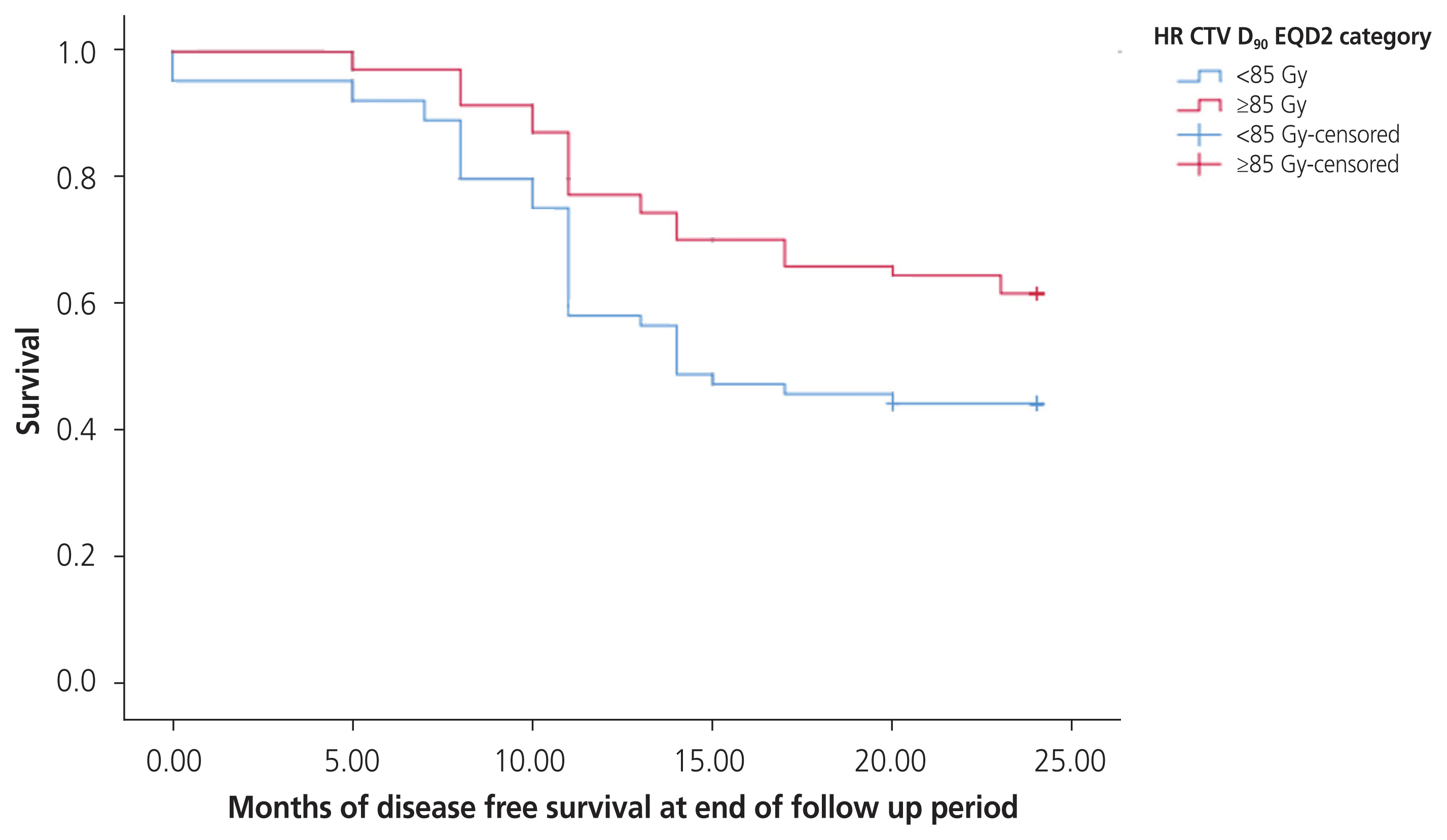
One hundred thirty-six patients were enrolled in the study. Delineated volume of HR-CTV ranged from 20.9 to 37.1 mL, with median value of 30.2 mL. The equivalent dose in 2 Gy per fraction (EQD2) for point ‘A’ ranged from 71.31 to 79.75 Gy with median value of 75.1 Gy and EQD2 HR-CTV D90 ranged from 71.9 to 89.7 Gy with median value of 85.1 Gy. 69.2% of patients showed complete response and after median follow-up of 25 months, 50 patients remained disease free, of whom, 74.0% had received ≥85 Gy to HR-CTV D90 versus 26.0% receiving <85 Gy to HR-CTV D90.
Conclusions
Amidst the unavailability of magnetic resonance imaging facilities in low middle income countries, incorporation of CT-image based treatment planning into routine practice for ICBT provides the scope to delineate volumes of target and OARs and to generate DVH data, which can prove to be a better surrogate for disease response and toxicity.
Keyword
Figure
Reference
-
References
1. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021; 71:209–49.2. International Commission on Radiation Units and Measurements. ICRU report 38 [Internet]. Bethesda (MD): International Commission on Radiation Units and Measurements;c1985. [cited 2023 Nov 13]. Available from: https://www.icru.org/report/dose-and-volume-specification-for-reporting-intracavitary-therapy-in-gynecology-report-38/ .3. Viswanathan AN, Erickson BA. Three-dimensional imaging in gynecologic brachytherapy: a survey of the American Brachytherapy Society. Int J Radiat Oncol Biol Phys. 2010; 76:104–9.4. Haie-Meder C, Pötter R, Van Limbergen E, Briot E, De Brabandere M, Dimopoulos J, et al. Recommendations from gynaecological (GYN) GEC-ESTRO Working Group (I): concepts and terms in 3D image based 3D treatment planning in cervix cancer brachytherapy with emphasis on MRI assessment of GTV and CTV. Radiother Oncol. 2005; 74:235–45.5. Pötter R, Haie-Meder C, Van Limbergen E, Barillot I, De Brabandere M, Dimopoulos J, et al. Recommendations from gynaecological (GYN) GEC ESTRO Working Group (II): concepts and terms in 3D image-based treatment planning in cervix cancer brachytherapy-3D dose volume parameters and aspects of 3D image-based anatomy, radiation physics, radiobiology. Radiother Oncol. 2006; 78:67–77.6. Prescribing, recording, and reporting brachytherapy for cancer of the cervix. J ICRU. 2013; 13:NP.7. Nag S, Erickson B, Thomadsen B, Orton C, Demanes JD, Petereit D. The American Brachytherapy Society recommendations for high-dose-rate brachytherapy for carcinoma of the cervix. Int J Radiat Oncol Biol Phys. 2000; 48:201–11.8. Viswanathan AN, Thomadsen B. American Brachytherapy Society consensus guidelines for locally advanced carcinoma of the cervix. Part I: general principles. Brachytherapy. 2012; 11:33–46.9. Viswanathan AN, Erickson B, Gaffney DK, Beriwal S, Bhatia SK, Lee Burnett O 3rd, et al. Comparison and consensus guidelines for delineation of clinical target volume for CT- and MR-based brachytherapy in locally advanced cervical cancer. Int J Radiat Oncol Biol Phys. 2014; 90:320–8.10. Viswanathan AN, Dimopoulos J, Kirisits C, Berger D, Pötter R. Computed tomography versus magnetic resonance imaging-based contouring in cervical cancer brachytherapy: results of a prospective trial and preliminary guidelines for standardized contours. Int J Radiat Oncol Biol Phys. 2007; 68:491–8.11. Viswanathan AN, Beriwal S, De Los Santos JF, Demanes DJ, Gaffney D, Hansen J, et al. American Brachytherapy Society consensus guidelines for locally advanced carcinoma of the cervix. Part II: high-dose-rate brachytherapy. Brachytherapy. 2012; 11:47–52.12. Anderson J, Huang Y, Kim Y. Dosimetric impact of point A definition on high-dose-rate brachytherapy for cervical cancer: evaluations on conventional point A and MRI-guided, conformal plans. J Contemp Brachytherapy. 2012; 4:241–6.13. Kirisits C, Pötter R, Lang S, Dimopoulos J, Wachter-Gerstner N, Georg D. Dose and volume parameters for MRI-based treatment planning in intracavitary brachytherapy for cervical cancer. Int J Radiat Oncol Biol Phys. 2005; 62:901–11.14. Kim H, Beriwal S, Houser C, Huq MS. Dosimetric analysis of 3D image-guided HDR brachytherapy planning for the treatment of cervical cancer: is point A-based dose prescription still valid in image-guided brachytherapy? Med Dosim. 2011; 36:166–70.15. Shi F, Yoder AK, Mach C, Dalwadi S, Anderson ML, Hall TR, et al. Impact of hematologic toxicities during concurrent chemoradiation for cervical cancer. Obstet Gynecol Sci. 2022; 65:176–87.16. Pötter R, Dimopoulos J, Georg P, Lang S, Waldhäusl C, Wachter-Gerstner N, et al. Clinical impact of MRI assisted dose volume adaptation and dose escalation in brachytherapy of locally advanced cervix cancer. Radiother Oncol. 2007; 83:148–55.17. Pötter R, Georg P, Dimopoulos JC, Grimm M, Berger D, Nesvacil N, et al. Clinical outcome of protocol based image (MRI) guided adaptive brachytherapy combined with 3D conformal radiotherapy with or without chemotherapy in patients with locally advanced cervical cancer. Radiother Oncol. 2011; 100:116–23.18. Georg P, Lang S, Dimopoulos JC, Dörr W, Sturdza AE, Berger D, et al. Dose-volume histogram parameters and late side effects in magnetic resonance image-guided adaptive cervical cancer brachytherapy. Int J Radiat Oncol Biol Phys. 2011; 79:356–62.19. Bandyopadhyay A, Mukherjee U, Ghosh S, Ghosh S, Sarkar SK. Pattern of failure with locally advanced cervical cancer- a retrospective audit and analysis of contributory factors. Asian Pac J Cancer Prev. 2018; 19:73–9.20. Onal C, Arslan G, Topkan E, Pehlivan B, Yavuz M, Oymak E, et al. Comparison of conventional and CT-based planning for intracavitary brachytherapy for cervical cancer: target volume coverage and organs at risk doses. J Exp Clin Cancer Res. 2009; 28:95.21. Goyal MK, Kehwar TS, Manjhi J, Barker JL, Heintz BH, Shide KL, et al. Dosimetric evaluation of tandem-based cervical high-dose-rate brachytherapy treatment planning using American Brachytherapy Society 2011 recommendations. J Radiother Pract. 2016; 15:283–9.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Accuracy of Dose Estimation in High Dose Rate Intracavitary Radiotherapy of Carcinoma of the Uterine Cervix
- Radiation sigmoiditis mimicking sigmoid colon cancer after radiation therapy for cervical cancer: the implications of three-dimensional image-based brachytherapy planning
- Clinical Evaluation of Dose Distribution in High Dose Rate Intracavitary Irradiation in the Treatment of Cervical Cancer
- Pelvic MRI Application to the Dosimetric Analysis in Brachytherapy of Uterine Cervix Carcinoma
- Intracavitary Dosimetry: A Comparison of Doses at Point A and B to Curie-minutes in Cervical Cancer