J Korean Neurosurg Soc.
2024 Jan;67(1):122-129. 10.3340/jkns.2022.0273.
Synchronous Carotid Body and Glomus Jugulare Tumors : A Case Report and Review of Literature
- Affiliations
-
- 1Department of Neurosurgery, Bangabandhu Sheikh Mujib Medical University, Shahbag, Bangladesh
- 2Department of Neurosurgery, Trauma Center, Gamma Knife Center, Cannizzaro Hospital, Catania, Italy
- 3Department of Neurosurgery, Enam Medical College, Savar, Bangladesh
- 4Department of Neurosurgery, Combined Military Hospital (CMH), Dhaka, Bangladesh
- 5Department of Neurosurgery, Dhaka Medical College Hospital, Dhaka, Bangladesh
- 6Department of Neurosurgery, Neurosurgery Clinic, Birgunj, Nepal
- KMID: 2550466
- DOI: http://doi.org/10.3340/jkns.2022.0273
Abstract
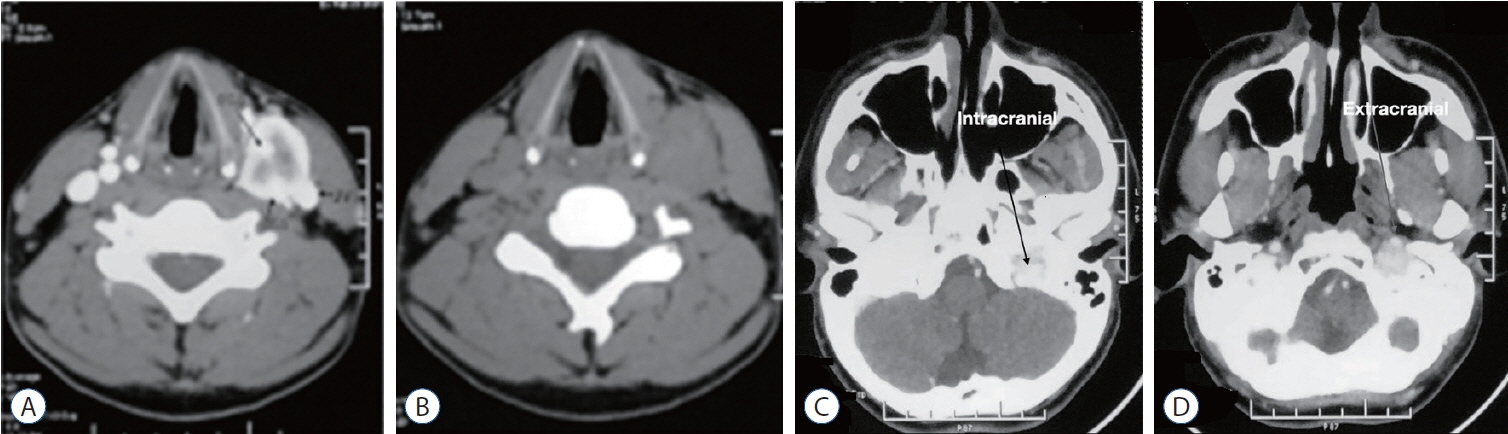
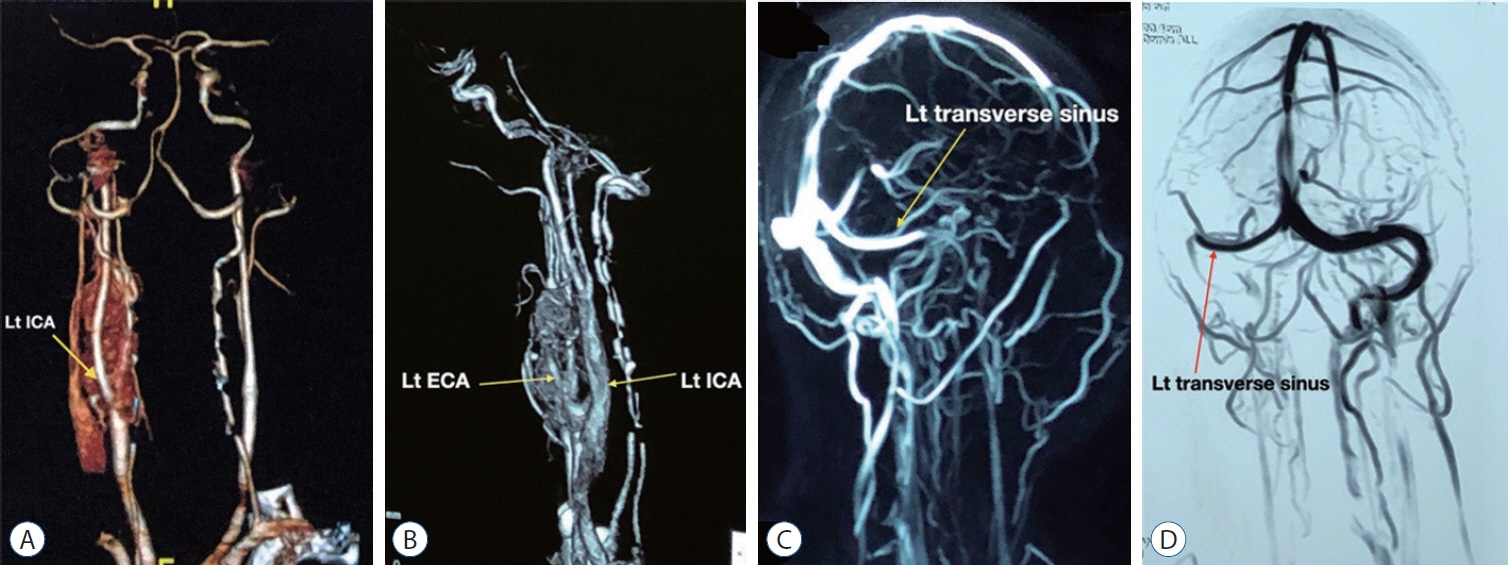
- Paragangliomas are rare neuroendocrine tumors that are usually benign in nature. They may be either familial or sporadic in their occurrence. Numerous neuroendocrine tumors are collectively included under the umbrella of paragangliomas. Among them, carotid body tumors and glomus jugulare tumors are extremely rare. Thus, we present a rare case of 29-year-old male who was admitted with hearing difficulties and tinnitus in the left ear, with swelling on the left side of the neck. Based on clinical and radiological findings, a diagnosis of left-sided glomus jugulare with carotid body tumor was made. The patient underwent a twostage surgery with an interval of approximately 2 months. Histopathology revealed a paraganglioma. Herein, we present the clinical features, imaging findings, management, and a brief review of literature on the classification, evaluation, and management of carotid body and glomus jugulare tumors. Paraganglioma is a slow-growing tumor. The synchronous occurrence of carotid body and glomus jugulare tumors is infrequent. Microsurgical resection remains the primary treatment modality. Therefore, our patient underwent two-stage surgery. The rarity of occurrence and the proximity and adherence to vital neurovascular structures have resulted in the treatment of paragangliomas remaining a challenge.
Figure
Reference
-
References
1. Alexander MJ, Moftakhar P. Nonatherosclerotic Carotid Lesions Emobolization in Winn HR (ed) : Youmans Neurological Surgery EBook. Philadelphia: Elsevier Health Sciences;2011. p. 3655–3664.2. Ammirati M, Zarzour H. Overview of Skull Base Tumors in Winn HR (ed) : Youmans Neurological Surgery E-Book. Philadelphia: Elsevier Health Sciences;2011. p. 1569–1586.3. Askenasy HM, Eppenstein SS, Herzberger EE. Tumor of the glomus jugulare co-existing possibly with carotid body tumor. Acta Neurochir (Wien). 3:170–179. 1953.
Article4. Ball JR, Hurlbert RJ. Endovascular Techniques for Tumor Emobolization in Winn HR (ed) : Youmans Neurological Surgery E-Book. Philadelphia: Elsevier Health Sciences;2011. p. 1226.5. Bogdasarian RS, Lotz PR. Multiple simultaneous paragangliomas of the head and neck in association with multiple retroperitoneal pheochromocytomas. Otolaryngol Head Neck Surg (1979). 87:648–652. 1979.
Article6. Casterline PF, Jaques DA. Simultaneous recurrent multiple chemodectomas. Arch Otolaryngol. 104:157–160. 1978.
Article7. Farrior JB 3rd, Hyams VJ, Benke RH, Farrior JB. Carcinoid apudoma arising in a glomus jugulare tumor: review of endocrine activity in glomus jugulare tumors. Laryngoscope. 90:110–119. 1980.
Article8. Gerosa M, Paolo R. Glomus Tumors in Winn HR (ed) : Youmans Neurological Surgery E-Book. Philadelphia: Elsevier Health Sciences;2011. p. 1594–1609.9. Green JD Jr, Brackmann DE, Nguyen CD, Arriaga MA, Telischi FF, De la Cruz A. Surgical management of previously untreated glomus jugulare tumors. Laryngoscope. 104(8 Pt 1):917–921. 1994.
Article10. Greenberg MS : Handbook of neurosurgery. Stuttgart : Thieme, 2019.11. Hoang VT, Trinh CT, Lai TAK, Doan DT, Tran TTT. Carotid body tumor: a case report and literature review. J Radiol Case Rep. 13:19–30. 2019.
Article12. Islam MR, Ansari A, Rahman A, Saklayen SMG, Muhammad N, Shah SK, et al. The perplexing postsurgical complication of carotid-jugular fistula: a bitter experience. Surg Neurol Int. 13:2. 2022.
Article13. Jackson CG, Harris PF, Glasscock ME 3rd, Fritsch M, Dimitrov E, Johnson GD, et al. Diagnosis and management of paragangliomas of the skull base. Am J Surg. 159:389–393. 1990.
Article14. Klingbeil JR. Multiplicity and familial incidence of carotid body and glomus jugulare tumors. Plas Reconst Surg. 38:489. 1966.
Article15. Liu JK, Sameshima T, Gottfried ON, Couldwell WT, Fukushima T. The combined transmastoid retro- and infralabyrinthine transjugular transcondylar transtubercular high cervical approach for resection of glomus jugulare tumors. Neurosurgery. 59(1 Suppl 1):ONS-115-25. discussion ONS115-25. 2006.
Article16. Luna-Ortiz K, Rascon-Ortiz M, Villavicencio-Valencia V, Granados-Garcia M, Herrera-Gomez A. Carotid body tumors: review of a 20-year experience. Oral Oncol. 41:56–61. 2005.
Article17. Mafee MF, Raofi B, Kumar A, Muscato C. Glomus faciale, glomus jugulare, glomus tympanicum, glomus vagale, carotid body tumors, and simulating lesions. Role of MR imaging. Radiol Clin North Am. 38:1059–1076. 2000.
Article18. Martins R, Bugalho MJ. Paragangliomas/pheochromocytomas: clinically oriented genetic testing. Int J Endocrinol. 2014:794187. 2014.
Article19. Moffat DA, Hardy DG. Surgical management of large glomus jugulare tumours: infra- and trans-temporal approach. J Laryngol Otol. 103:1167–1180. 1989.
Article20. Pareschi R, Righini S, Destito D, Raucci AF, Colombo S. Surgery of glomus jugulare tumors. Skull Base. 13:149–157. 2003.
Article21. Parkinson D. Intracranial pheochromocytomas (active glomus jugulare). Case report. J Neurosurg. 31:94–100. 1969.22. Sessions RT, McSwain B, Carlson RI, Scott HW Jr. Surgical experiences with tumors of the carotid body, glomus jugulare and retroperitoneal nonchromaffin paraganglia. Ann Surg. 150:808–823. 1959.
Article23. Thompson JW, Cohen SR. Management of bilateral carotid body tumors and a glomus jugulare tumor in a child. Int J Pediatr Otorhinolaryngol. 17:75–87. 1989.
Article24. Thompson JW, Cohen SR. Management of bilateral carotid body tumors and a glomus jugulare tumor in a child. Int J Pediatr Otorhinolaryngol. 17:75–87. 1989.
Article25. Watkins LD, Mendoza N, Cheesman AD, Symon L. Glomus jugulare tumours: a review of 61 cases. Acta Neurochir (Wien). 130:66–70. 1994.
Article26. Young WF Jr. Paragangliomas: clinical overview. Ann N Y Acad Sci. 1073:21–29. 2006.27. Zacks SI. Chemodectomas occurring concurrently in the neck (carotid body), temporal bone (glomus jugulare) and retroperitoneum; report of a case with histochemical observations. Am J Pathol. 34:293. 1958.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Metastatic Thy roid Carcinoma of Jugular Foramen Simulating Glomus Jugulare Tumor: A Case Report
- A Case of Extra-adrenal Paraganglioma of the Scrotum
- Surgical Resection of Glomus Jugulare Tumor via Infratemporal Approach after Preoperative Embolization
- Multiple Paragangliomas: Three Cases
- Intraosseous Glomus Tumor: A Case Report