J Korean Neurosurg Soc.
2024 Jan;67(1):115-121. 10.3340/jkns.2022.0263.
De Novo Vertebral Artery Dissecting Aneurysm after Parent Artery Occlusion of the Contralateral Vertebral Artery
- Affiliations
-
- 1Department of Neurosurgery, Kano General Hospital, Osaka, Japan
- 2Department of Neurology, Kano General Hospital, Osaka, Japan
- 3Department of Neurosurgery, Osaka Medical and Pharmaceutical University, Takatsuki, Japan
- KMID: 2550465
- DOI: http://doi.org/10.3340/jkns.2022.0263
Abstract
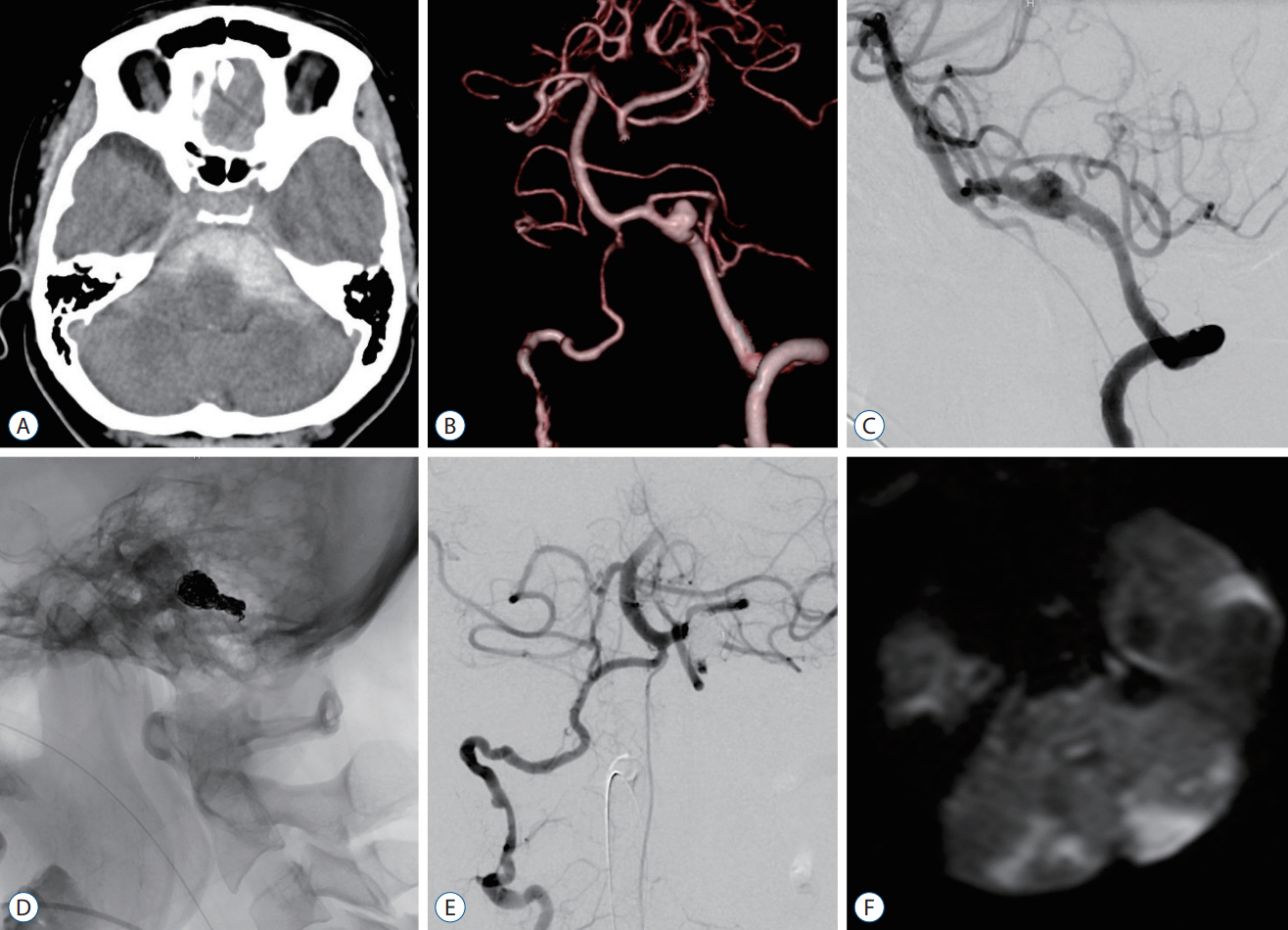
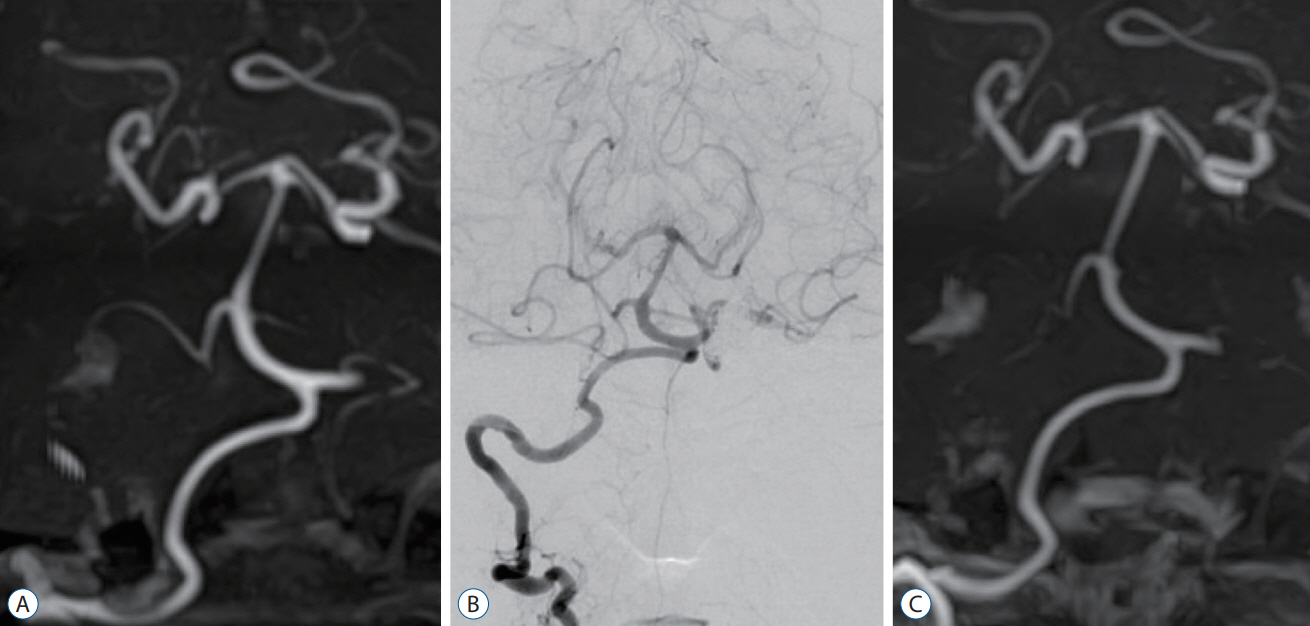
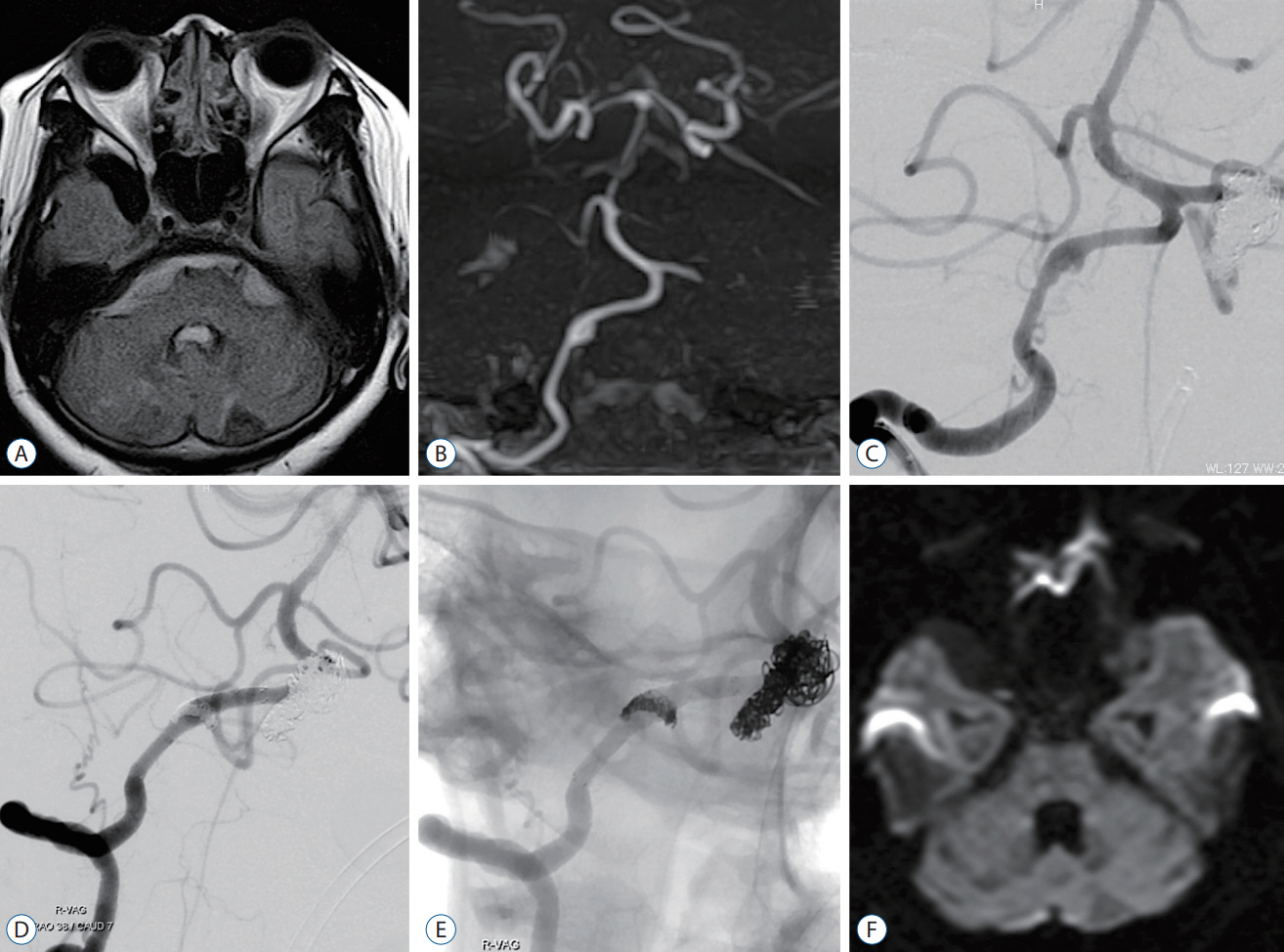
- After treatment of unilateral vertebral artery dissecting aneurysm (VADA), de novo VADA rarely occurs on the contralateral side. In this article, we report a case of subarachnoid hemorrhage (SAH) due to de novo VADA in the contralateral vertebral artery (VA) 3 years after parent artery occlusion of unilateral VADA, with a review of the literature. A 47-year-old woman was admitted to our hospital complaining of headache and impaired consciousness. Head computed tomography showed SAH, and three-dimensional computed tomography angiography showed a fusiform aneurysm in the left VA. We performed an emergency parent artery occlusion. Three years and 3 months after the initial treatment, the patient presented to our hospital with complaints of headache and neck pain. Magnetic resonance imaging revealed SAH, and magnetic resonance angiography revealed de novo VADA in the right VA. We performed a stent-assisted coil embolization. The patient had a good postoperative course and was discharged with a modified Rankin scale score of 0. Long-term follow-up is necessary in patients with VADA because contralateral de novo VADA can develop even several years after the initial treatment.
Figure
Reference
-
References
1. Cho DY, Choi JH, Kim BS, Shin YS. Comparison of clinical and radiologic outcomes of diverse endovascular treatments in vertebral artery dissecting aneurysm involving the origin of PICA. World Neurosurg. 121:e22–e31. 2019.
Article2. Chung J, Kim BS, Lee D, Kim TH, Shin YS. Vertebral artery occlusion with vertebral artery-to-posterior inferior cerebellar artery stenting for preservation of the PICA in treating ruptured vertebral artery dissection. Acta Neurochir (Wien). 152:1489–1492. 2010.
Article3. Endo H, Matsumoto Y, Kondo R, Sato K, Fujimura M, Inoue T, et al. Medullary infarction as a poor prognostic factor after internal coil trapping of a ruptured vertebral artery dissection. J Neurosurg. 118:131–139. 2013.
Article4. Fukunaga A, Tabuse M, Naritaka H, Nakamura T, Akiyama T. Spontaneous resolution of nontraumatic bilateral intracranial vertebral artery dissections. Neurol Med Chir (Tokyo). 42:491–495. 2002.
Article5. Guan J, Li G, Kong X, He C, Long J, Qin H, et al. Endovascular treatment for ruptured and unruptured vertebral artery dissecting aneurysms: a meta-analysis. J Neurointerv Surg. 9:558–563. 2017.
Article6. Inui Y, Oiwa Y, Terada T, Nakakita K, Kamei I, Hayashi S. De novo vertebral artery dissecting aneurysm after contralateral vertebral artery occlusion--two case reports. Neurol Med Chir (Tokyo). 46:32–36. 2006.
Article7. Katsuno M, Mizunari T, Kobayashi S, Takahashi H, Teramoto A. Rupture of a vertebral artery dissecting aneurysm developing immediately after trapping of a dissecting aneurysm on the contralateral vertebral artery: case report. Neurol Med Chir (Tokyo). 49:468–470. 2009.
Article8. Kidani N, Sugiu K, Hishikawa T, Hiramatsu M, Haruma J, Nishihiro S, et al. De novo vertebral artery dissecting aneurysm after internal trapping of the contralateral vertebral artery. Acta Neurochir (Wien). 159:1329–1333. 2017.
Article9. Kim MJ, Chung J, Kim SL, Roh HG, Kwon BJ, Kim BS, et al. Stenting from the vertebral artery to the posterior inferior cerebellar artery. AJNR Am J Neuroradiol. 33:348–352. 2012.
Article10. Kim YS, Kim TS, Yang IC, Joo SP. Staged, combined management of ruptured vertebral artery dissecting aneurysms involving the posterior inferior cerebellar artery: report of 4 cases and review of the literature. World Neurosurg. 128:444–447. 2019.
Article11. Komoribayashi N, Kubo Y, Koji T, Nishikawa Y, Ogawa A, Ogasawara K. Rupture of contralateral vertebral artery dissection two years after spontaneous occlusion of ipsilateral vertebral artery dissection: a case report. Jpn J Stroke. 35:291–294. 2013.
Article12. Kubo Y, Miura K, Suzuki M, Tsuiki K, Kuwata N, Kubo N, et al. Development of a dissecting aneurysm on the vertebral artery immediately after occlusion of the contralateral vertebral artery: a case report. Neurosurg Rev. 21:177–180. 1998.
Article13. Madaelil TP, Wallace AN, Chatterjee AN, Zipfel GJ, Dacey RG Jr, Cross DT 3rd, et al. Endovascular parent vessel sacrifice in ruptured dissecting vertebral and posterior inferior cerebellar artery aneurysms: clinical outcomes and review of the literature. J Neurointerv Surg. 8:796–801. 2016.
Article14. Mizutani T, Aruga T, Kirino T, Miki Y, Saito I, Tsuchida T. Recurrent subarachnoid hemorrhage from untreated ruptured vertebrobasilar dissecting aneurysms. Neurosurgery. 36:905–911. discussion 912-913. 1995.
Article15. Otawara Y, Ogasawara K, Ogawa A, Kogure T. Dissecting aneurysms of the bilateral vertebral arteries with subarachnoid hemorrhage: report of three cases. Neurosurgery. 50:1372–1374. discussion 1374-1375. 2002.
Article16. Ro A, Kageyama N, Abe N, Takatsu A, Fukunaga T. Intracranial vertebral artery dissection resulting in fatal subarachnoid hemorrhage: clinical and histopathological investigations from a medicolegal perspective. J Neurosurg. 110:948–954. 2009.
Article17. Robertson JJ, Koyfman A. Cervical artery dissections: a review. J Emerg Med. 51:508–518. 2016.
Article18. Ryu CW, Park S, Shin HS, Koh JS. Complications in stent-assisted endovascular therapy of ruptured intracranial aneurysms and relevance to antiplatelet administration: a systematic review. AJNR Am J Neuroradiol. 36:1682–1688. 2015.
Article19. Yasui T, Sakamoto H, Kishi H, Komiyama M, Iwai Y, Yamanaka K, et al. Bilateral dissecting aneurysms of the vertebral arteries resulting in subarachnoid hemorrhage: case report. Neurosurgery. 42:162–164. discussion 165. 1998.
Article20. You W, Feng J, Liu Q, Liu X, Lv J, Jiang Y, et al. Case report: de novo vertebral artery dissection after intravascular stenting of the contralateral unruptured vertebral artery aneurysm. Front Neurol. 12:59997. 2021.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Dissecting Aneurysm of the Intracranial Vertbral Artery: Case Report
- Antegrade Recanalization of Parent Artery after Internal Trapping of Ruptured Vertebral Artery Dissecting Aneurysm
- Stent Assisted Coil Embolization of a Dissecting Aneurysm of the Vertebral Artery: A Case Involving a Patient with Hypoplasia of the Contralateral Vertebral Artery
- Endovascular Coil Trapping of a Ruptured Dissecting Aneurysm of the Vertebral Artery Using Detachable Coils and Micro-Tornado(R) Coils
- Stent-Jack Technique for Ruptured Vertebral Artery Dissecting Aneurysm Involving the Origin of Posterior Inferior Cerebellar Artery