Cancer Res Treat.
2024 Jan;56(1):238-246. 10.4143/crt.2023.539.
Association between Metabolically Healthy Status and Risk of Gastrointestinal Cancer
- Affiliations
-
- 1School of Medicine, Nankai University, Tianjin, China
- 2Department of Hepatobiliary Surgery, Kailuan General Hospital, Tangshan, China
- 3Department of Radiation Oncology, North China University of Science and Technology Affiliated Hospital, Tangshan, China
- 4The Faculty of Hepatopancreatobiliary Surgery, The First Medical Center, Chinese People’s Liberation Army General Hospital, Beijing, China
- KMID: 2550339
- DOI: http://doi.org/10.4143/crt.2023.539
Abstract
- Purpose
Although obesity is associated with numerous diseases, the risks of disease may depend on metabolically healthy status. Nevertheless, it is unclear to whether metabolically healthy status affects risk of gastrointestinal (GI) cancer in general Chinese population.
Materials and Methods
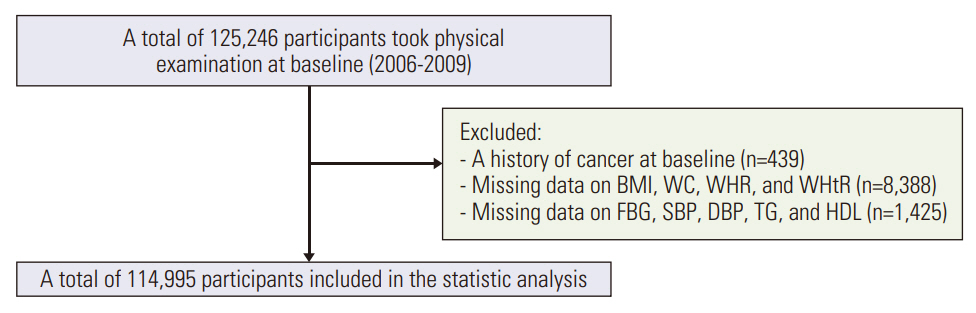
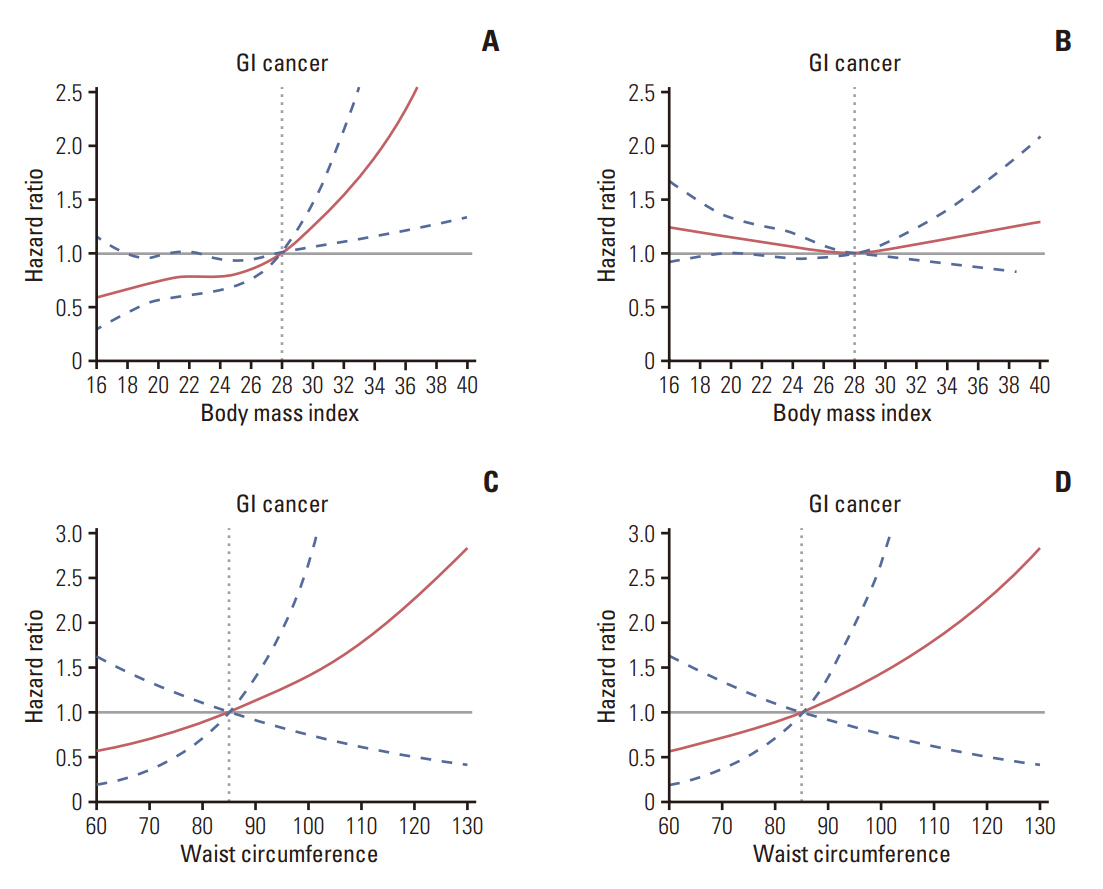
A total of 114,995 participants who met the criteria were included from the Kailuan Study. The study participants were divided into four groups according to body mass index (BMI)/waist circumference (WC) and metabolic status. Incident of GI cancer (esophageal cancer, gastric cancer, liver cancer, biliary cancer, pancreatic cancer, and colorectal cancer) during 2006-2020 were confirmed by review of medical records. The Cox proportional hazard regression models were used to assess the association metabolically healthy status with the risk of GI cancer by calculating the hazard ratios (HR) and 95% confidence interval (CI).
Results
During a mean 13.76 years of follow-up, we documented 2,311 GI cancers. Multivariate Cox regression analysis showed that compared with the metabolically healthy normal-weight group, metabolically healthy obese (MHO) participants demonstrated an increased risk of developing GI cancer (HR, 1.54; 95% CI, 1.11 to 2.13) by BMI categories. However, such associations were not found for WC category. These associations were moderated by age, sex, and anatomical site of the tumor. Individuals with metabolic unhealthy normal-weight or metabolic unhealthy obesity phenotype also have an increased risk of GI cancer.
Conclusion
MHO phenotype was associated with increased risk of GI cancer. Moreover, individuals who complicated by metabolic unhealthy status have an increased risk of developing GI cancer. Hence, clinicians should consider the risk of incident GI cancer in people with abnormal metabolically healthy status and counsel them about metabolic fitness and weight control.
Figure
Reference
-
References
1. Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022; 72:7–33.2. Xia C, Dong X, Li H, Cao M, Sun D, He S, et al. Cancer statistics in China and United States, 2022: profiles, trends, and determinants. Chin Med J (Engl). 2022; 135:584–90.3. Wild CP, Weiderpass E, Stewart BW. World cancer report 2020: cancer research for cancer prevention [Internet. Lyon: International Agency for Research on Cancer;2020. [cited 2021 Feb 22]. Available from: http://publications.iarc.fr/586.4. GBD 2019 Cancer Risk Factors Collaborators. The global burden of cancer attributable to risk factors, 2010-19: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2022; 400:563–91.5. Wu Y, Li Y, Giovannucci E. Potential impact of time trend of lifestyle risk factors on burden of major gastrointestinal cancers in China. Gastroenterology. 2021; 161:1830–41.6. Murphy N, Jenab M, Gunter MJ. Adiposity and gastrointestinal cancers: epidemiology, mechanisms and future directions. Nat Rev Gastroenterol Hepatol. 2018; 15:659–70.7. Bluher M. Metabolically healthy obesity. Endocr Rev. 2020; 41:bnaa004.8. Morkedal B, Vatten LJ, Romundstad PR, Laugsand LE, Janszky I. Risk of myocardial infarction and heart failure among metabolically healthy but obese individuals: HUNT (NordTrondelag Health Study), Norway. J Am Coll Cardiol. 2014; 63:1071–8.9. Lin CJ, Chang YC, Cheng TY, Lo K, Liu SJ, Yeh TL. The association between metabolically healthy obesity and risk of cancer: a systematic review and meta-analysis of prospective cohort studies. Obes Rev. 2020; 21:e13049.10. Sedlmeier AM, Viallon V, Ferrari P, Peruchet-Noray L, Fontvieille E, Amadou A, et al. Body shape phenotypes of multiple anthropometric traits and cancer risk: a multi-national cohort study. Br J Cancer. 2023; 128:594–605.11. Cui H, Liu Q, Wu Y, Cao L. Cumulative triglyceride-glucose index is a risk for CVD: a prospective cohort study. Cardiovasc Diabetol. 2022; 21:22.12. Ma X, Cui H, Sun M, Liu Q, Liu X, Li G, et al. Fasting blood glucose, cholesterol, and risk of primary liver cancer: the Kailuan study. Cancer Res Treat. 2021; 53:1113–22.13. Chen C, Lu FC. The guidelines for prevention and control of overweight and obesity in Chinese adults. Biomed Environ Sci. 2004; 17 Suppl:1–36.14. Zhou BF; Coorperative Meta-Analysis Group Of China Obesity Task Force. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults: study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed Environ Sci. 2002; 15:83–96.15. Lavie CJ, Laddu D, Arena R, Ortega FB, Alpert MA, Kushner RF. Healthy weight and obesity prevention: JACC health promotion series. J Am Coll Cardiol. 2018; 72:1506–31.16. Stefan N, Kantartzis K, Machann J, Schick F, Thamer C, Rittig K, et al. Identification and characterization of metabolically benign obesity in humans. Arch Intern Med. 2008; 168:1609–16.17. Stefan N, Schick F, Haring HU. Causes, characteristics, and consequences of metabolically unhealthy normal weight in humans. Cell Metab. 2017; 26:292–300.18. Pang Q, Zhang JY, Song SD, Qu K, Xu XS, Liu SS, et al. Central obesity and nonalcoholic fatty liver disease risk after adjusting for body mass index. World J Gastroenterol. 2015; 21:1650–62.19. Huang T, Tworoger SS, Willett WC, Stampfer MJ, Rosner BA. Associations of early life and adulthood adiposity with risk of epithelial ovarian cancer. Ann Oncol. 2019; 30:303–9.20. Kabat GC, Kim MY, Stefanick M, Ho GYF, Lane DS, Odegaard AO, et al. Metabolic obesity phenotypes and risk of colorectal cancer in postmenopausal women. Int J Cancer. 2018; 143:543–51.21. Hashimoto Y, Hamaguchi M, Obora A, Kojima T, Fukui M. Impact of metabolically healthy obesity on the risk of incident gastric cancer: a population-based cohort study. BMC Endocr Disord. 2020; 20:11.22. Park YM, White AJ, Nichols HB, O’Brien KM, Weinberg CR, Sandler DP. The association between metabolic health, obesity phenotype and the risk of breast cancer. Int J Cancer. 2017; 140:2657–66.23. Murphy N, Cross AJ, Abubakar M, Jenab M, Aleksandrova K, Boutron-Ruault MC, et al. A nested case-control study of metabolically defined body size phenotypes and risk of colorectal cancer in the European Prospective Investigation into Cancer and Nutrition (EPIC). PLoS Med. 2016; 13:e1001988.24. Cao Z, Zheng X, Yang H, Li S, Xu F, Yang X, et al. Association of obesity status and metabolic syndrome with site-specific cancers: a population-based cohort study. Br J Cancer. 2020; 123:1336–44.25. Braun S, Bitton-Worms K, LeRoith D. The link between the metabolic syndrome and cancer. Int J Biol Sci. 2011; 7:1003–15.26. Aguilar-Salinas CA, Garcia EG, Robles L, Riano D, Ruiz-Gomez DG, Garcia-Ulloa AC, et al. High adiponectin concentrations are associated with the metabolically healthy obese phenotype. J Clin Endocrinol Metab. 2008; 93:4075–9.27. Stolzenberg-Solomon RZ, Graubard BI, Chari S, Limburg P, Taylor PR, Virtamo J, et al. Insulin, glucose, insulin resistance, and pancreatic cancer in male smokers. JAMA. 2005; 294:2872–8.28. Liu T, Zhang Q, Wang Y, Ma X, Zhang Q, Song M, et al. Association between the TyG index and TG/HDL-C ratio as insulin resistance markers and the risk of colorectal cancer. BMC Cancer. 2022; 22:1007.29. Eckel N, Li Y, Kuxhaus O, Stefan N, Hu FB, Schulze MB. Transition from metabolic healthy to unhealthy phenotypes and association with cardiovascular disease risk across BMI categories in 90 257 women (the Nurses’ Health Study): 30 year follow-up from a prospective cohort study. Lancet Diabetes Endocrinol. 2018; 6:714–24.30. Gao M, Lv J, Yu C, Guo Y, Bian Z, Yang R, et al. Metabolically healthy obesity, transition to unhealthy metabolic status, and vascular disease in Chinese adults: a cohort study. PLoS Med. 2020; 17:e1003351.31. Nam KH, Yun HR, Joo YS, Kim J, Lee S, Lee C, et al. Changes in obese metabolic phenotypes over time and risk of incident chronic kidney disease. Diabetes Obes Metab. 2018; 20:2778–91.32. Cho YK, Lee J, Kim HS, Park JY, Lee WJ, Kim YJ, et al. Impact of transition in metabolic health and obesity on the incident chronic kidney disease: a nationwide cohort study. J Clin Endocrinol Metab. 2020; 105:dgaa033.33. Soriguer F, Gutierrez-Repiso C, Rubio-Martin E, Garcia-Fuentes E, Almaraz MC, Colomo N, et al. Metabolically healthy but obese, a matter of time? Findings from the prospective Pizarra study. J Clin Endocrinol Metab. 2013; 98:2318–25.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Metabolically Healthy Obesity Is Associated with an Increased Risk of Colorectal Adenoma Occurrence Diagnosed by Surveillance Colonoscopy
- Incidence of Prostate Cancer according to Metabolic Health Status: a Nationwide Cohort Study
- Gender Difference in Health-Related Behaviors associated with Metabolic Status-Obesity Phenotypes among Korean Adults
- Characteristics of Young Korean Metabolically Healthy Obese Patient: Based on Retrospective Analysis of Republic of Korea Navy Soldiers' Medical Examination
- Metabolically Healthy Obesity: Epidemiology, Criteria, and Implications in Chronic Kidney Disease