Cancer Res Treat.
2024 Jan;56(1):125-133. 10.4143/crt.2023.673.
Impact of Social Support during Diagnosis and Treatment on Disease Progression in Young Patients with Breast Cancer: A Prospective Cohort Study
- Affiliations
-
- 1Department of Clinical Research Design and Evaluation, SAIHST, Sungkyunkwan University, Seoul, Korea
- 2Center for Clinical Epidemiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 3Department of Health Sciences and Technology, SAIHST, Sungkyunkwan University, Seoul, Korea
- 4Department of Digital Health, SAIHST, Sungkyunkwan University, Seoul, Korea
- 5Research Institution for Future Medicine, Samsung Medical Center, Seoul, Korea
- 6Division of Breast Surgery, Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 7Division of Hematology-Oncology, Department of Internal Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2550329
- DOI: http://doi.org/10.4143/crt.2023.673
Abstract
- Purpose
We evaluated the association between changes in social support after cancer treatment and recurrence-free survival (RFS) in such patients using a prospective cohort study.
Materials and Methods
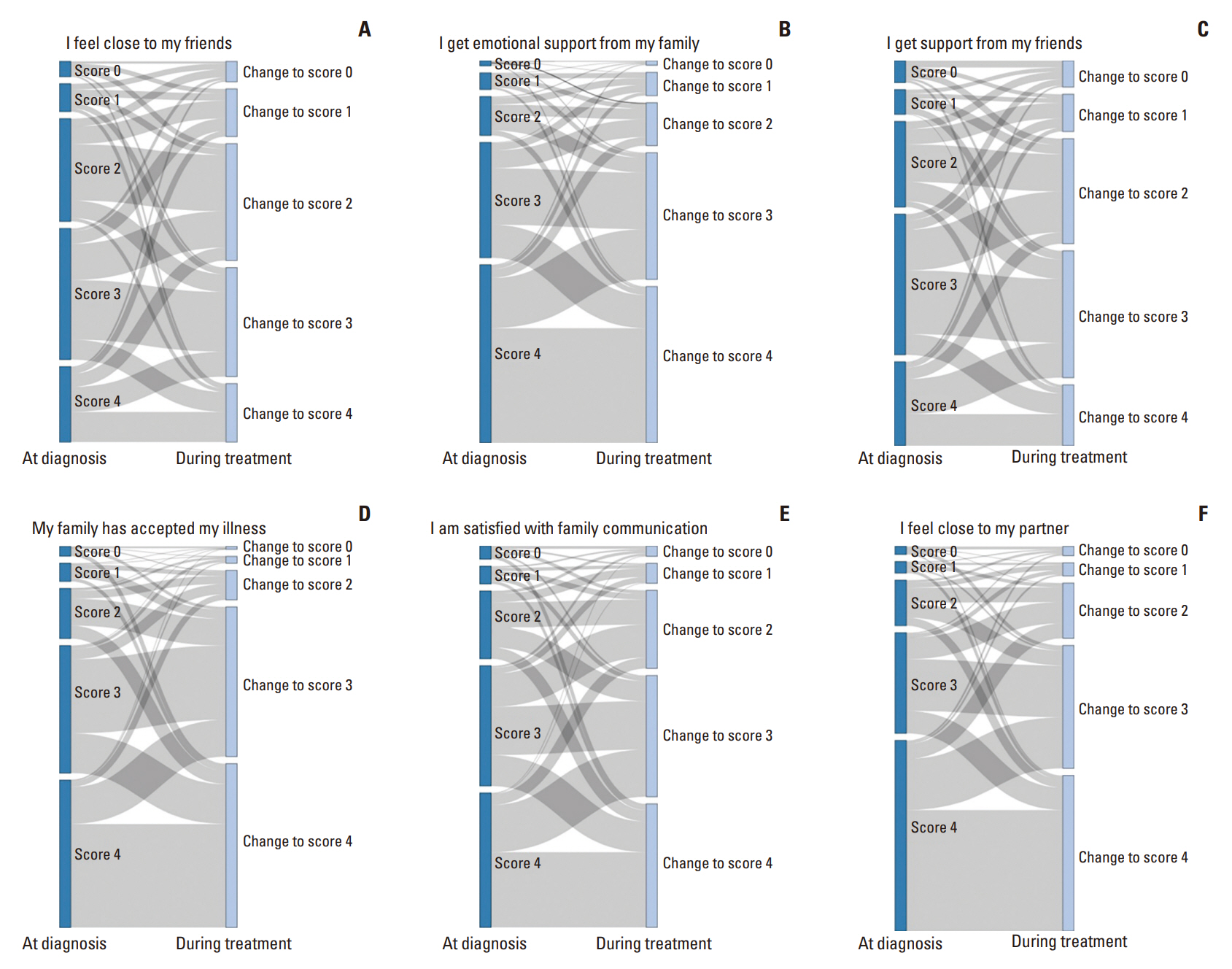
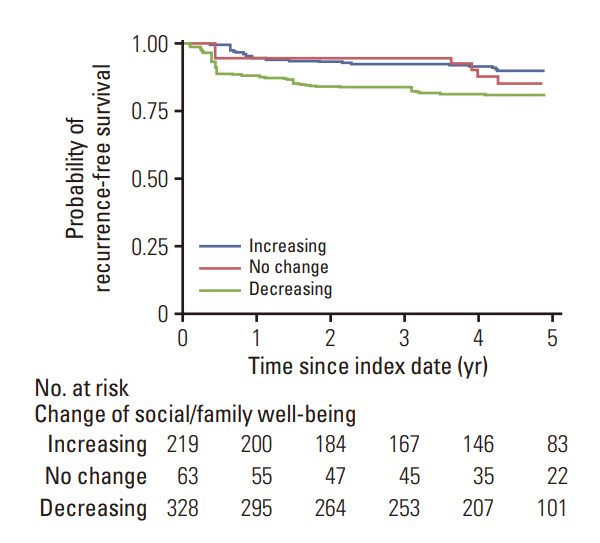
Data were obtained from a prospective cohort study (NCT03131089) conducted at Samsung Medical Center (2013-2021). The primary outcome measure was RFS. Social support was measured using the social and family well-being (SFWB) domain of the Functional Assessment of Cancer Therapy-General. We calculated the changes in SFWB scores before and during treatment and the hazard ratio for RFS by comparing such changes.
Results
The mean±standard deviation (SD) age of the patients was 35±3.9 years, and 71.5% and 64.8% of the patients were married and had children, respectively. The mean±SD SFWB score at baseline was 20.5±5.0 out of 26. After cancer treatment, 35.9%, 10.3%, and 53.8% of the participants had increasing, unchanged, and decreasing SFWB scores, respectively. The decreasing SFWB score group had a higher risk of mortality or recurrence than the increasing group. Risk factors for the decreasing score were the presence of children during diagnosis.
Conclusion
In this cohort, changes in social support after treatment were associated with RFS in young patients with breast cancer. Health professionals should develop family interventions to help them receive proper social support.
Figure
Reference
-
References
1. Kenyon M, Mayer DK, Owens AK. Late and long-term effects of breast cancer treatment and surveillance management for the general practitioner. J Obstet Gynecol Neonatal Nurs. 2014; 43:382–98.2. Choi E, Henneghan AM. Comparing fatigue, loneliness, daytime sleepiness, and stress in younger and older breast cancer survivors: a cross-sectional analysis. Clin J Oncol Nurs. 2022; 26:155–64.3. Keesing S, Rosenwax L, McNamara B. The implications of women’s activity limitations and role disruptions during breast cancer survivorship. Womens Health (Lond). 2018; 14:1745505718756381.4. Mackenzie CR. ‘It is hard for mums to put themselves first’: how mothers diagnosed with breast cancer manage the sociological boundaries between paid work, family and caring for the self. Soc Sci Med. 2014; 117:96–106.5. Ong WL, Schouwenburg MG, van Bommel ACM, Stowell C, Allison KH, Benn KE, et al. A standard set of value-based patient-centered outcomes for breast cancer: the International Consortium for Health Outcomes Measurement (ICHOM) Initiative. JAMA Oncol. 2017; 3:677–85.6. Simpson JS, Carlson LE, Beck CA, Patten S. Effects of a brief intervention on social support and psychiatric morbidity in breast cancer patients. Psychooncology. 2002; 11:282–94.7. Mirrielees JA, Breckheimer KR, White TA, Denure DA, Schroeder MM, Gaines ME, et al. Breast cancer survivor advocacy at a university hospital: development of a peer support program with evaluation by patients, advocates, and clinicians. J Cancer Educ. 2017; 32:97–104.8. Kroenke CH, Kubzansky LD, Schernhammer ES, Holmes MD, Kawachi I. Social networks, social support, and survival after breast cancer diagnosis. J Clin Oncol. 2006; 24:1105–11.9. Elovainio M, Lumme S, Arffman M, Manderbacka K, Pukkala E, Hakulinen C. Living alone as a risk factor for cancer incidence, case-fatality and all-cause mortality: a nationwide registry study. SSM Popul Health. 2021; 15:100826.10. Boen CE, Barrow DA, Bensen JT, Farnan L, Gerstel A, Hendrix LH, et al. Social relationships, inflammation, and cancer survival. Cancer Epidemiol Biomarkers Prev. 2018; 27:541–9.11. Kroenke CH, Michael YL, Poole EM, Kwan ML, Nechuta S, Leas E, et al. Postdiagnosis social networks and breast cancer mortality in the After Breast Cancer Pooling Project. Cancer. 2017; 123:1228–37.12. Sammarco A, Konecny LM. Quality of life, social support, and uncertainty among Latina breast cancer survivors. Oncol Nurs Forum. 2008; 35:844–9.13. Fong AJ, Scarapicchia TM, McDonough MH, Wrosch C, Sabiston CM. Changes in social support predict emotional well-being in breast cancer survivors. Psychooncology. 2017; 26:664–71.14. Chou AF, Stewart SL, Wild RC, Bloom JR. Social support and survival in young women with breast carcinoma. Psychooncology. 2012; 21:125–33.15. Bloom JR, Stewart SL, Johnston M, Banks P, Fobair P. Sources of support and the physical and mental well-being of young women with breast cancer. Soc Sci Med. 2001; 53:1513–24.16. Ruiz-Rodriguez I, Hombrados-Mendieta I, Melguizo-Garin A, Martos-Mendez MJ. The association of sources of support, types of support and satisfaction with support received on perceived stress and quality of life of cancer patients. Integr Cancer Ther. 2021; 20:1534735421994905.17. Yan J, Chen Y, Luo M, Hu X, Li H, Liu Q, et al. Chronic stress in solid tumor development: from mechanisms to interventions. J Biomed Sci. 2023; 30:8.18. Lee EH, Chun M, Kang S, Lee HJ. Validation of the Functional Assessment of Cancer Therapy-General (FACT-G) scale for measuring the health-related quality of life in Korean women with breast cancer. Jpn J Clin Oncol. 2004; 34:393–9.19. Chatterjee S, Simonoff JS. Handbook of regression analysis. New York: John Wiley & Sons;2013.20. Zabalegui A, Sanchez S, Sanchez PD, Juando C. Nursing and cancer support groups. J Adv Nurs. 2005; 51:369–81.21. Cho J, Smith K, Choi EK, Kim IR, Chang YJ, Park HY, et al. Public attitudes toward cancer and cancer patients: a national survey in Korea. Psychooncology. 2013; 22:605–13.22. Ernst J, Mehnert A, Dietz A, Hornemann B, Esser P. Perceived stigmatization and its impact on quality of life: results from a large register-based study including breast, colon, prostate and lung cancer patients. BMC Cancer. 2017; 17:741.23. Harms CA, Cohen L, Pooley JA, Chambers SK, Galvao DA, Newton RU. Quality of life and psychological distress in cancer survivors: the role of psycho-social resources for resilience. Psychooncology. 2019; 28:271–7.24. Zhang H, Zhao Q, Cao P, Ren G. Resilience and quality of life: exploring the mediator role of social support in patients with breast cancer. Med Sci Monit. 2017; 23:5969–79.25. Shrout MR, Renna ME, Madison AA, Alfano CM, Povoski SP, Lipari AM, et al. Relationship satisfaction predicts lower stress and inflammation in breast cancer survivors: a longitudinal study of within-person and between-person effects. Psychoneuroendocrinology. 2020; 118:104708.26. Karelina K, DeVries AC. Modeling social influences on human health. Psychosom Med. 2011; 73:67–74.27. Hinzey A, Gaudier-Diaz MM, Lustberg MB, DeVries AC. Breast cancer and social environment: getting by with a little help from our friends. Breast Cancer Res. 2016; 18:54.28. Kissane DW, Grabsch B, Love A, Clarke DM, Bloch S, Smith GC. Psychiatric disorder in women with early stage and advanced breast cancer: a comparative analysis. Aust N Z J Psychiatry. 2004; 38:320–6.29. Dinapoli L, Colloca G, Di Capua B, Valentini V. Psychological aspects to consider in breast cancer diagnosis and treatment. Curr Oncol Rep. 2021; 23:38.30. Cai T, Huang Q, Yuan C. Emotional, informational and instrumental support needs in patients with breast cancer who have undergone surgery: a cross-sectional study. BMJ Open. 2021; 11:e048515.31. Ares I, Lebel S, Bielajew C. The impact of motherhood on perceived stress, illness intrusiveness and fear of cancer recurrence in young breast cancer survivors over time. Psychol Health. 2014; 29:651–70.32. Rauch PK, Muriel AC. The importance of parenting concerns among patients with cancer. Crit Rev Oncol Hematol. 2004; 49:37–42.33. Helseth S, Ulfsaet N. Parenting experiences during cancer. J Adv Nurs. 2005; 52:38–46.34. Chen SQ, Sun N, Ge W, Su JE, Li QR. The development process of self-acceptance among Chinese women with breast cancer. Jpn J Nurs Sci. 2020; 17:e12308.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Impact of Social Cognitive Constructs on Dietary Behaviors in Breast Cancer Survivors
- Impacts of Uncertainty and Social Support on the Quality of Life of Breast Cancer Survivors after Chemotherapy: Based on Self-help Group Participants
- The Impact of Symptom Burden, Social Support, Self-Efficacy, and eHealth Literacy on the Quality of Life of Patients Undergoing Breast Cancer Treatment: A Cross-Sectional Study
- Factors Influencing Family Functioning of Couples with Breast Cancer in the Middle Adaptation Stage: Trajectory of Chronic Illness
- Symptom Distress and Coping in Young Korean Breast Cancer Survivors: The Mediating Effects of Social Support and Resilience