Ann Surg Treat Res.
2024 Jan;106(1):45-50. 10.4174/astr.2024.106.1.45.
Training efficacy of robotic duct-to-mucosa pancreaticojejunostomy simulation using silicone models for surgical fellows
- Affiliations
-
- 1Department of Surgery and Cancer Research Institute, Seoul National University College of Medicine, Seoul, Korea
- 2Department of Surgery, Korea University Guro Hospital, Korea University College of Medicine, Seoul, Korea
- 3Department of Surgery, Korea University Anam Hospital, Korea University College of Medicine, Seoul, Korea
- 4Department of Surgery, Chung-Ang University Gwangmyeong Hospital, Gwangmyeong, Korea
- KMID: 2550250
- DOI: http://doi.org/10.4174/astr.2024.106.1.45
Abstract
- Purpose
In the era of minimally invasive surgery (MIS), robotic pancreatoduodenectomy (PD) is actively performed, and clinical fellows need to thoroughly prepare for MIS-PD during the training process. Although pancreaticojejunostomy (PJ) is a difficult anastomosis that requires repeated practice, there are obstacles preventing its practice that concerns patient safety and limited time in the actual operating room. This study evaluated the efficacy of simulation-based training of robotic duct-to-mucosa PJ using pancreatic and intestinal silicone models using a scoring system.
Methods
Three pancreatobiliary clinical fellows who had never performed a real robotic PJ participated in this study. Each trainee, who was well acquainted with master’s video created by a senor surgeon, performed the robotic PJ procedures 9 times, and 3 independent pancreatobiliary surgeons assessed the videos and analyzed the scores using a blind method.
Results
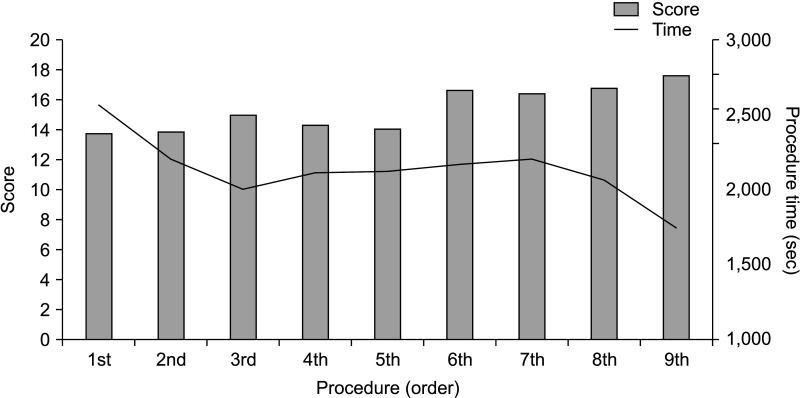
The mean robotic PJ times for the 3 trainees were 42.8 and 29.1 minutes for the first and 9th videos, respectively. The mean score was 13.8 (range, 6–17) for the first video and 17.7 (range, 15–19) for the 9th video. When comparing earlier and later attempts, the PJ time decreased significantly (2,201.67 seconds vs. 2,045.50 seconds, P = 0.007), whereas test scores increased significantly (total score 14.22 vs. 16.89, P = 0.011).
Conclusion
This robotic education system will help pancreatobiliary trainees overcome the learning curves efficiently and quickly without raising ethical concerns associated with animal models or direct practice with human subjects. This will be of practical assistance to trainees preparing for MIS-PD.
Keyword
Figure
Reference
-
1. Egle JP, Malladi SV, Gopinath N, Mittal VK. Simulation training improves resident performance in hand-sewn vascular and bowel anastomoses. J Surg Educ. 2015; 72:291–296. PMID: 25481803.
Article2. Kang JS, Sohn HJ, Choi YJ, Byun Y, Lee JM, Lee M, et al. The development and clinical efficacy of simulation training of open duct-to-mucosa pancreaticojejunostomy using pancreas and intestine silicone models. Ann Surg Treat Res. 2022; 102:328–334. PMID: 35800994.
Article3. Bergmeister KD, Aman M, Kramer A, Schenck TL, Riedl O, Daeschler SC, et al. Simulating surgical skills in animals: systematic review, costs & acceptance analyses. Front Vet Sci. 2020; 7:570852. PMID: 33195561.4. Kang YH, Kang JS, Lee M, Jung HS, Yun WG, Cho YJ, et al. Comparisons of short-term outcomes of anastomotic methods of duct-to-mucosa pancreaticojejunostomy: out-layer continuous suture versus modified Blumgart method. Ann Surg Treat Res. 2022; 103:331–339. PMID: 36601337.5. Tseng JF, Pisters PW, Lee JE, Wang H, Gomez HF, Sun CC, et al. The learning curve in pancreatic surgery. Surgery. 2007; 141:456–463. PMID: 17383522.6. van Hilst J, de Rooij T, Bosscha K, Brinkman DJ, van Dieren S, Dijkgraaf MG, et al. Laparoscopic versus open pancreatoduodenectomy for pancreatic or periampullary tumours (LEOPARD-2): a multicentre, patient-blinded, randomised control led phase 2/3 trial. Lancet Gastroenterol Hepatol. 2019; 4:199–207. PMID: 30685489.7. Casciani F, Trudeau MT, Asbun HJ, Ball CG, Bassi C, Behrman SW, et al. Surgeon experience contributes to improved outcomes in pancreatoduodenectomies at high risk for fistula development. Surgery. 2021; 169:708–720. PMID: 33386129.8. Chan KS, Wang ZK, Syn N, Goh BK. Learning curve of laparoscopic and robotic pancreas resections: a systematic review. Surgery. 2021; 170:194–206. PMID: 33541746.9. Park HM, Han SS, Park SJ, Kim SW. Learning curve for pancreatoduodenectomy: can it be generalized? ANZ J Surg. 2020; 90:1414–1421. PMID: 32255265.10. Takagi K, Umeda Y, Yoshida R, Yagi T, Fujiwara T, Zureikat AH, et al. Surgical training model and safe implementation of robotic pancreatoduodenectomy in Japan: a technical note. World J Surg Oncol. 2021; 19:55. PMID: 33608019.11. Alaker M, Wynn GR, Arulampalam T. Virtual reality training in laparoscopic surgery: a systematic review & meta-analysis. Int J Surg. 2016; 29:85–94. PMID: 26992652.12. Portelli M, Bianco SF, Bezzina T, Abela JE. Virtual reality training compared with apprenticeship training in laparoscopic surgery: a meta-analysis. Ann R Coll Surg Engl. 2020; 102:672–684. PMID: 32820649.13. Jensen K, Ringsted C, Hansen HJ, Petersen RH, Konge L. Simulation-based training for thoracoscopic lobectomy: a randomized controlled trial: virtual-reality versus black-box simulation. Surg Endosc. 2014; 28:1821–1829. PMID: 24442678.14. Kryklywy JH, Roach VA, Todd RM. Assessing the efficacy of tablet-based simulations for learning pseudo-surgical instrumentation. PLoS One. 2021; 16:e0245330. PMID: 33444407.15. Ritter FE, Yeh MK, Yan Y, Siu KC, Oleynikov D. Effects of varied surgical simulation training schedules on motor-skill acquisition. Surg Innov. 2020; 27:68–80. PMID: 31631788.16. Tam V, Zenati M, Novak S, Chen Y, Zureikat AH, Zeh HJ 3rd, et al. Robotic pancreatoduodenectomy biotissue curriculum has validity and improves technical performance for surgical oncology fellows. J Surg Educ. 2017; 74:1057–1065. PMID: 28578981.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- CORRIGENDUM: Training efficacy of robotic duct-to-mucosa pancreaticojejunostomy simulation using silicone models for surgical fellows
- The development and clinical efficacy of simulation training of open duct-to-mucosa pancreaticojejunostomy using pancreas and intestine silicone models
- Technical Feasibility of Robotic Single Site Central Pancreatectomy with Duct-to-Mucosa Pancreaticojejunostomy in Cadaveric Experiment
- Congenital Heart Surgery Skill Training Using Simulation Models: Not an Option but a Necessity
- Usefulness of the new articulating laparoscopic instrument in laparoscopic pancreaticoduodenectomy