Korean J Transplant.
2023 Dec;37(4):299-305. 10.4285/kjt.23.0045.
T cell posttransplant lymphoproliferative disorder after kidney transplantation progressing to acute liver failure: a case report
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea
- 2Organ Transplantation Center, Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea
- 3Department of Surgery, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2550242
- DOI: http://doi.org/10.4285/kjt.23.0045
Abstract
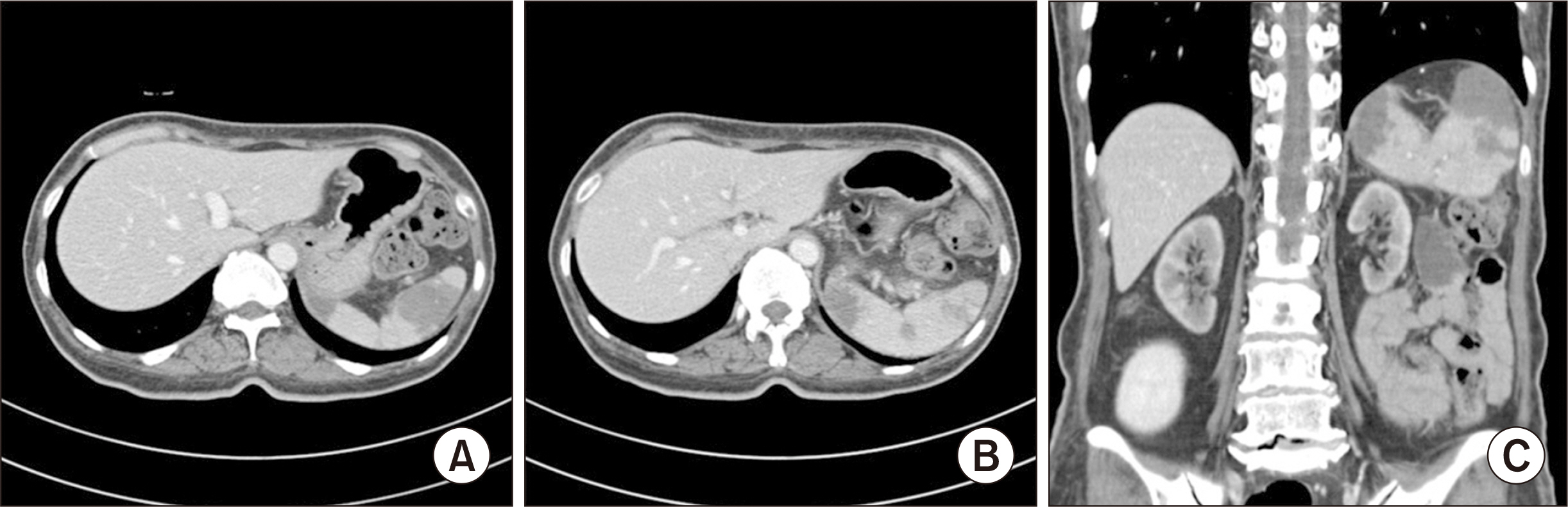
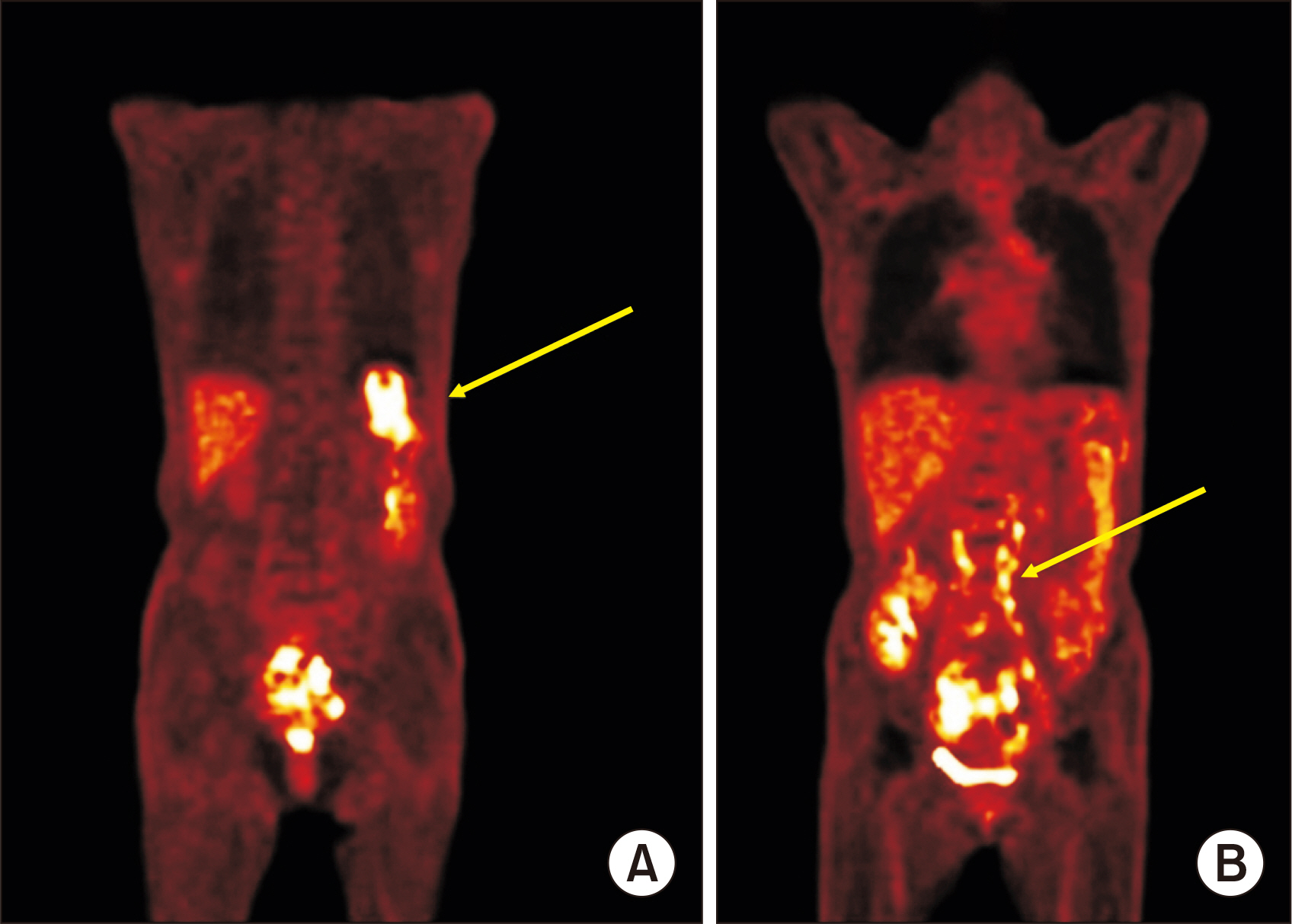
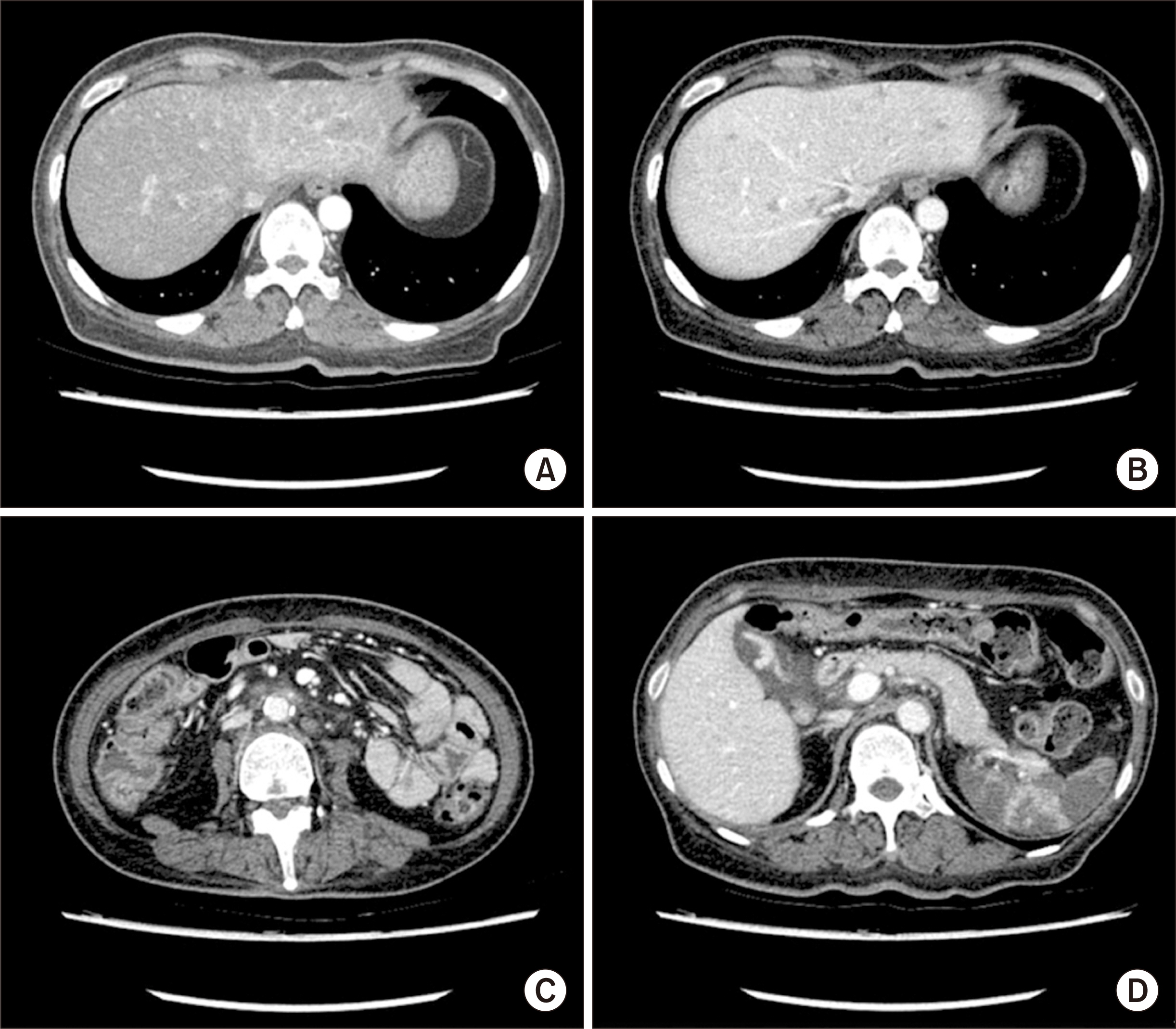
- Posttransplant lymphoproliferative disorder (PTLD) is a rare and serious complication of kidney transplantation (KT), with 85% of cases being of B cell lineage. We present a case of T cell PTLD (T-PTLD) that rapidly progressed to liver failure, septic shock, and death despite various therapeutic interventions. A 50-year-old woman underwent ABO- and human leukocyte antigen-compatible preemptive living donor KT for diabetic endstage kidney disease under basiliximab induction therapy. During routine monitoring, 2 months after KT, her Epstein-Barr (EB) viral load was found to be elevated to 318,443 copies/mL. Despite a reduction in maintenance immunosuppressants and preemptive rituximab treatment, the EB viremia continued to increase. Eight months after KT, abdominopelvic computed tomography revealed multifocal splenic lesions and nonspecific lymph node enlargement. Concurrently, the patient’s liver function tests began to deteriorate without evidence of viral hepatitis infection. A liver biopsy confirmed the di- agnosis of EB virus-associated T-PTLD with CD3 and CD56 expression. Only 2 months after the PTLD diagnosis, the patient developed acute and severe liver failure. She died 12 days after being hospitalized, despite the administration of rescue cytotoxic chemo-therapy. This case exemplifies the challenges of managing refractory EB virus-associated T-PTLD after KT, for which no specific treatment options are currently available. Further research into preventative and therapeutic methods for T-PTLD is warranted.
Keyword
Figure
Reference
-
1. Dierickx D, Habermann TM. 2018; Post-transplantation lymphoproliferative disorders in adults. N Engl J Med. 378:549–62. DOI: 10.1056/NEJMra1702693. PMID: 29414277.2. Francis A, Johnson DW, Teixeira-Pinto A, Craig JC, Wong G. 2018; Incidence and predictors of post-transplant lymphoproliferative disease after kidney transplantation during adulthood and childhood: a registry study. Nephrol Dial Transplant. 33:881–9. DOI: 10.1093/ndt/gfx356. PMID: 29342279.3. Tiede C, Maecker-Kolhoff B, Klein C, Kreipe H, Hussein K. 2013; Risk factors and prognosis in T-cell posttransplantation lymphoproliferative diseases: reevaluation of 163 cases. Transplantation. 95:479–88. DOI: 10.1097/TP.0b013e3182762e07. PMID: 23296147.4. Sprangers B, Riella LV, Dierickx D. 2021; Posttransplant lymphoproliferative disorder following kidney transplantation: a review. Am J Kidney Dis. 78:272–81. DOI: 10.1053/j.ajkd.2021.01.015. PMID: 33774079.5. Ashrafi F, Shahidi S, Mehrzad V, Mortazavi M, Hosseini SF. 2021; Survival of post-transplant lymphoproliferative disorder after kidney transplantation in patients under rapamycin treatment. Int J Hematol Oncol Stem Cell Res. 15:239–48. DOI: 10.18502/ijhoscr.v15i4.7479. PMID: 35291663. PMCID: PMC8888361.6. Barba T, Bachy E, Maarek A, Fossard G, Genestier L, Anglicheau D, et al. 2021; Characteristics of T- and NK-cell lymphomas after renal transplantation: a French national multicentric cohort study. Transplantation. 105:1858–68. DOI: 10.1097/TP.0000000000003568. PMID: 33560724.7. Cazzola M. 2016; Introduction to a review series: the 2016 revision of the WHO classification of tumors of hematopoietic and lymphoid tissues. Blood. 127:2361–4. DOI: 10.1182/blood-2016-03-657379. PMID: 27069255.8. Swerdlow SH, Campo E, Pileri SA, Harris NL, Stein H, Siebert R, et al. 2016; The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 127:2375–90. DOI: 10.1182/blood-2016-01-643569. PMID: 26980727. PMCID: PMC4874220.9. Campo E, Swerdlow SH, Harris NL, Pileri S, Stein H, Jaffe ES. 2011; The 2008 WHO classification of lymphoid neoplasms and beyond: evolving concepts and practical applications. Blood. 117:5019–32. DOI: 10.1182/blood-2011-01-293050. PMID: 21300984. PMCID: PMC3109529.10. Dierickx D, Tousseyn T, Gheysens O. 2015; How I treat posttransplant lymphoproliferative disorders. Blood. 126:2274–83. DOI: 10.1182/blood-2015-05-615872. PMID: 26384356.11. Dotti G, Fiocchi R, Motta T, Mammana C, Gotti E, Riva S, et al. 2002; Lymphomas occurring late after solid-organ transplantation: influence of treatment on the clinical outcome. Transplantation. 74:1095–102. DOI: 10.1097/00007890-200210270-00007. PMID: 12438953.12. Quinlan SC, Pfeiffer RM, Morton LM, Engels EA. 2011; Risk factors for early-onset and late-onset post-transplant lymphoproliferative disorder in kidney recipients in the United States. Am J Hematol. 86:206–9. DOI: 10.1002/ajh.21911. PMID: 21264909. PMCID: PMC3311225.13. Fischer E, Delibrias C, Kazatchkine MD. 1991; Expression of CR2 (the C3dg/EBV receptor, CD21) on normal human peripheral blood T lymphocytes. J Immunol. 146:865–9. DOI: 10.4049/jimmunol.146.3.865. PMID: 1703182.14. Herreman A, Dierickx D, Morscio J, Camps J, Bittoun E, Verhoef G, et al. 2013; Clinicopathological characteristics of posttransplant lymphoproliferative disorders of T-cell origin: single-center series of nine cases and meta-analysis of 147 reported cases. Leuk Lymphoma. 54:2190–9. DOI: 10.3109/10428194.2013.775436. PMID: 23402267.15. Magro CM, Weinerman DJ, Porcu PL, Morrison CD. 2007; Post-transplant EBV-negative anaplastic large-cell lymphoma with dual rearrangement: a propos of two cases and review of the literature. J Cutan Pathol. 34 Suppl 1:1–8. DOI: 10.1111/j.1600-0560.2006.00712.x. PMID: 17997729.16. Henter JI, Horne A, Aricó M, Egeler RM, Filipovich AH, Imashuku S, et al. 2007; HLH-2004: diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 48:124–31. DOI: 10.1002/pbc.21039. PMID: 16937360.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hematopoietic Stem Cell Transplantation after Posttransplant Lymphoproliferative Disorder
- Posttransplant Lymphoproliferative Disorder: A Report of 4 Cases
- A Case Report of Posttransplant Lymphoproliferative Disorders Successfully Treated with R-CHOP in Korea
- Post-transplantation Lymphoproliferative Disorder in Transplanted Liver: A Case Report
- Four Cases of Posttransplant Lymphoproliferative Disease (PTLD) Following Renal Transplantation