Korean J Transplant.
2023 Dec;37(4):260-268. 10.4285/kjt.23.0037.
Modified patch-conduit venoplasty for portal vein hypoplasia in pediatric liver transplantation
- Affiliations
-
- 1Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Department of Pediatrics, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2550237
- DOI: http://doi.org/10.4285/kjt.23.0037
Abstract
- Background
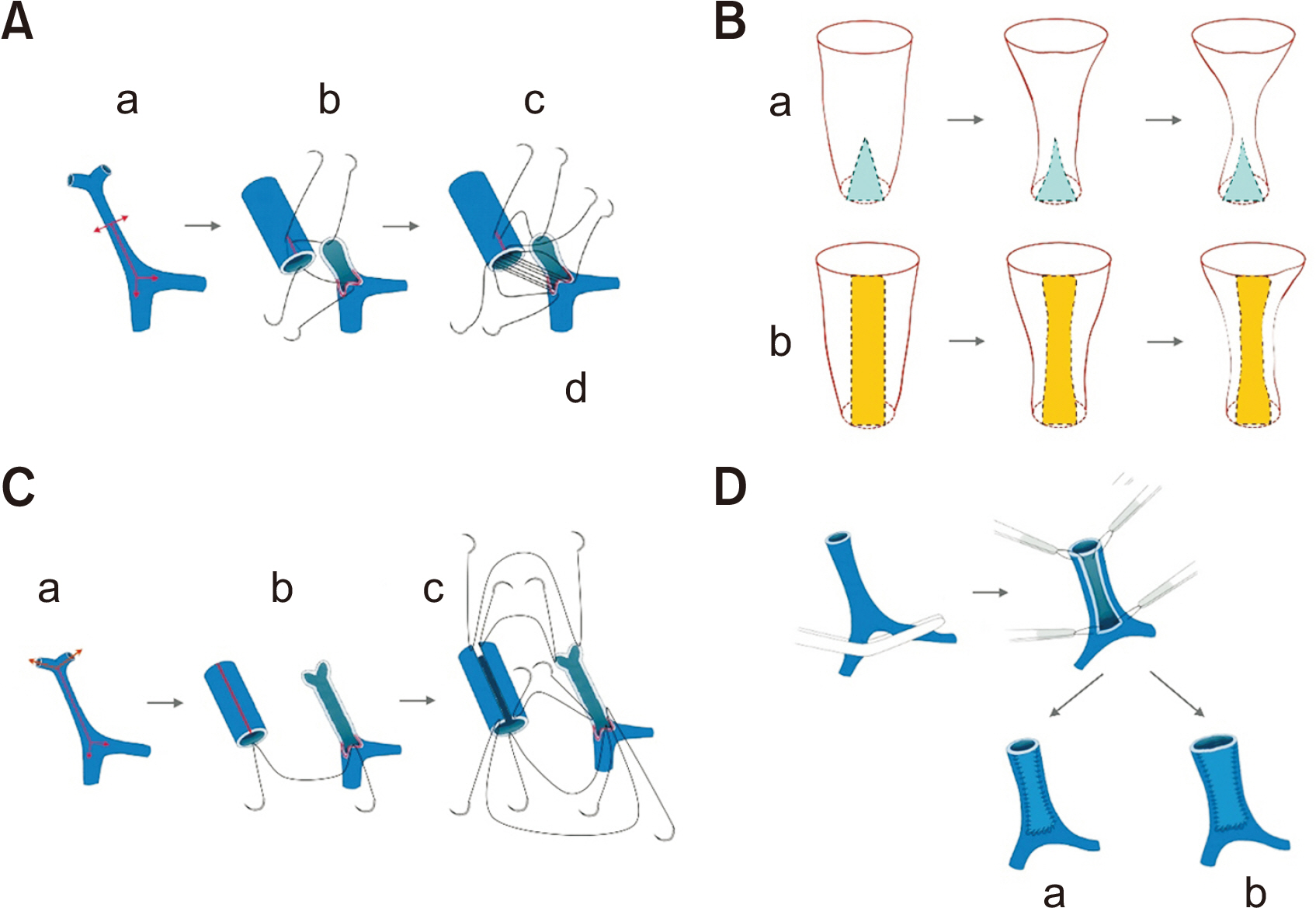
Portal vein (PV) interposition can induce various PV-related complications, making more reliable techniques necessary. The present study describes the development of a modified patch venoplasty technique, combining the native PV wall and a vein homograft conduit, called modified patch-conduit venoplasty (MPCV).
Methods
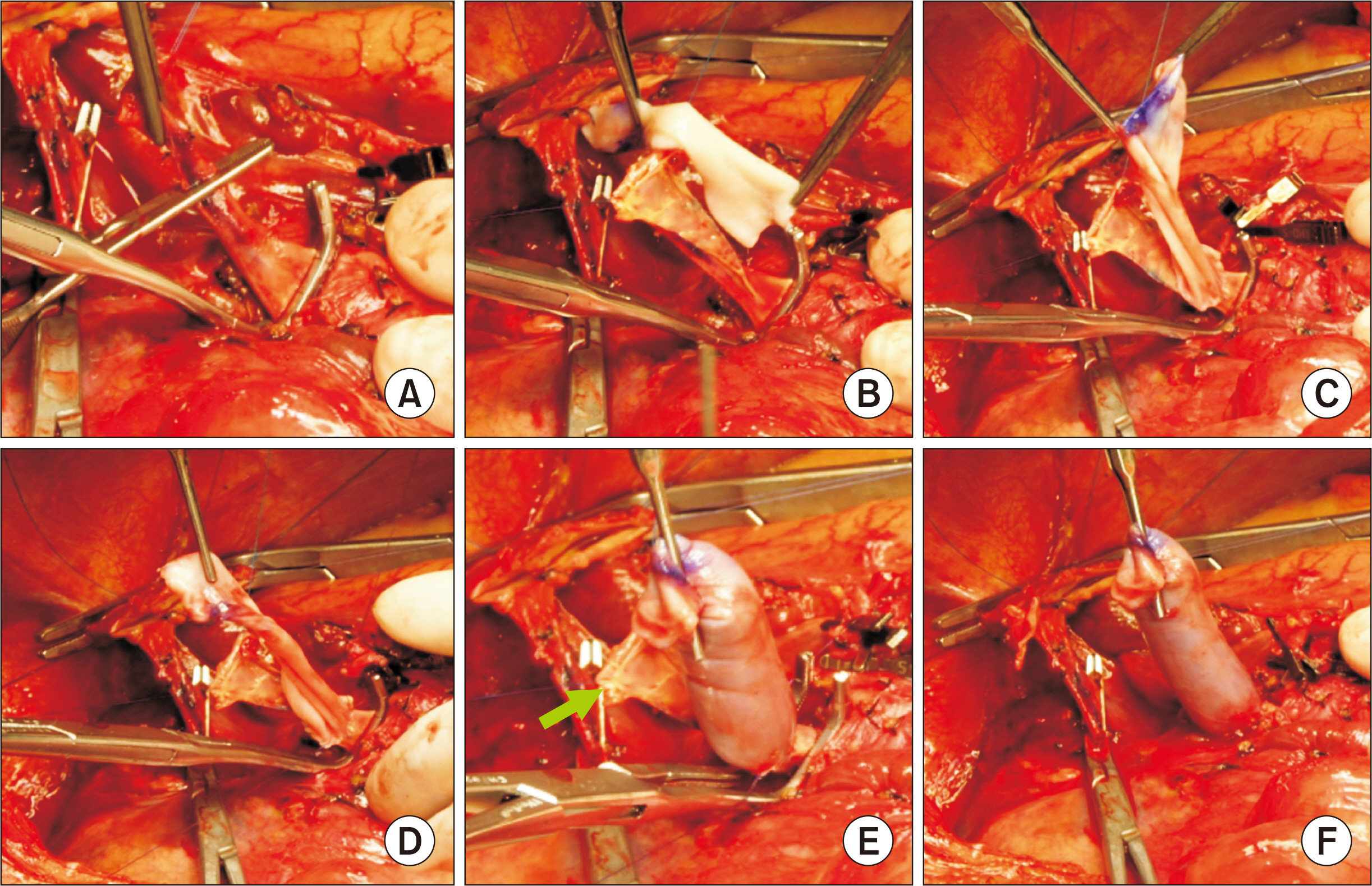
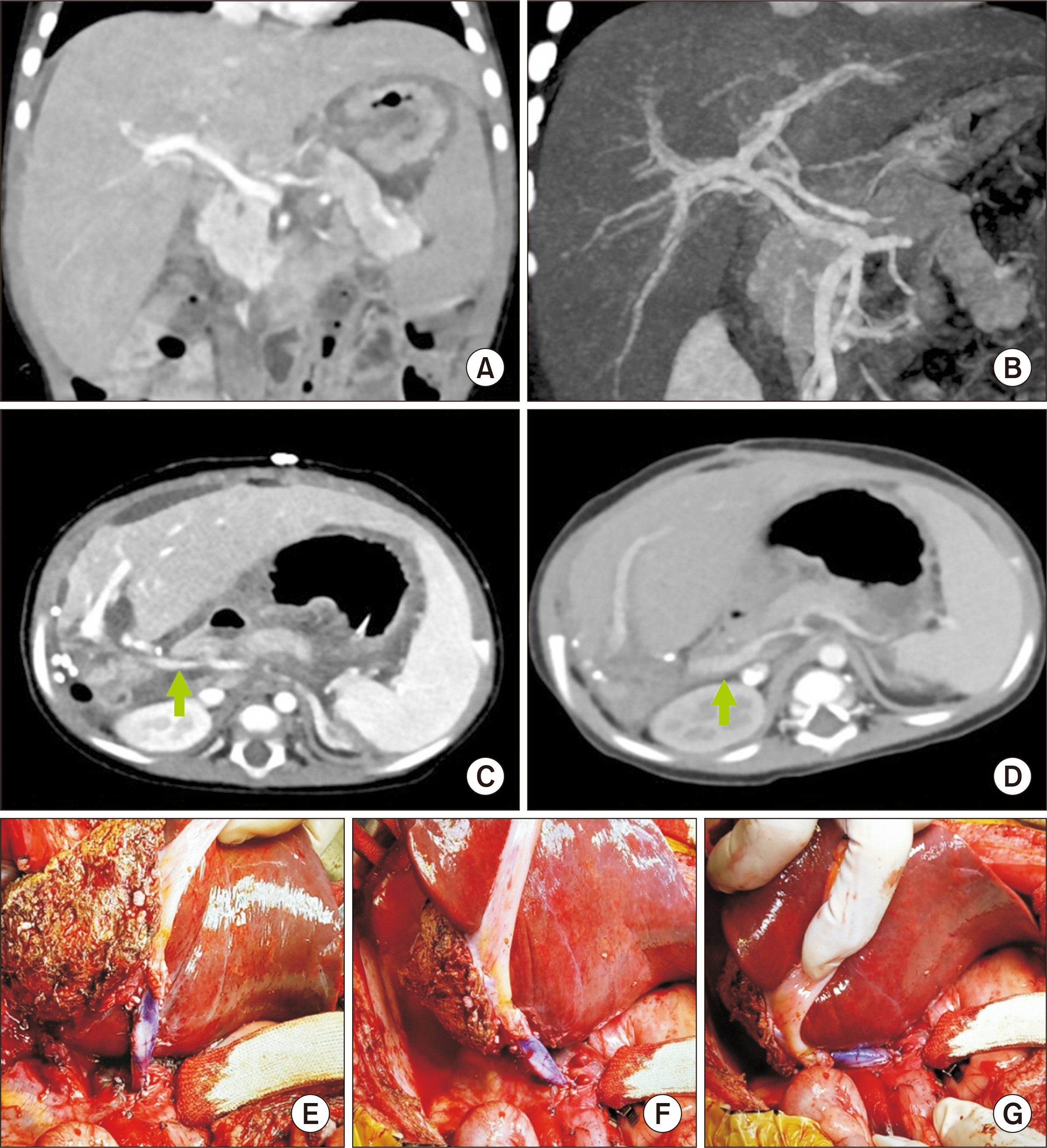
The surgical technique for MPCV was optimized by simulation and applied to seven pediatric patients undergoing liver transplantation (LT) for biliary atresia combined with PV hypoplasia.
Results
The simulation study revealed that inserting the whole-length native PV wall as a longitudinal rectangular patch was more effective in preventing PV conduit stenosis than the conventional technique using triangular partial insertion. These findings were used to develop the MPCV technique, in which the native PV wall was converted into a long rectangular patch, acting as a backbone for PV reconstruction. A longitudinal incision on the vein conduit converted the cylindrical vein into a large vein patch. The wall of the native PV was fully preserved as the posterior wall of the PV conduit, thus preventing longitudinal redundancy and unwanted rotation of the reconstructed PV. This technique was applied to seven patients with biliary atresia undergoing living-donor and deceased-donor split LT. None of these patients has experienced PV complications for up to 12 months after transplantation.
Conclusions
This newly devised MCPV technique can replace conventional PV interposition. MCPV may be a surgical option for reliable PV reconstruction using fresh or cryopreserved vein homografts during pediatric LT.
Keyword
Figure
Cited by 1 articles
-
Living donor liver transplantation with pericholedochal collateral vein anastomosis in a pediatric patient with congenital absence of the portal vein
Jung-Man Namgoong, Shin Hwang, Gil-Chun Park, Sujin Kang, Kyung Mo Kim, Seak Hee Oh
Ann Liver Transplant. 2023;3(2):118-127. doi: 10.52604/alt.23.0016.
Reference
-
1. Sakamoto S, Uchida H, Kitajima T, Shimizu S, Yoshimura S, Takeda M, et al. 2020; The outcomes of portal vein reconstruction with vein graft interposition in pediatric liver transplantation for small children with biliary atresia. Transplantation. 104:90–6. DOI: 10.1097/TP.0000000000002793. PMID: 31205260.2. Namgoong JM, Hwang S, Ko GY, Kwon H, Ha S, Oh SH, et al. 2022; Usability of intraoperative cine-portogram during liver transplantation in young pediatric patients with biliary atresia. Pediatr Transplant. 26:e14207. DOI: 10.1111/petr.14207. PMID: 34888999.3. Hwang S, Kim DY, Ahn CS, Moon DB, Kim KM, Park GC, et al. 2013; Computational simulation-based vessel interposition reconstruction technique for portal vein hypoplasia in pediatric liver transplantation. Transplant Proc. 45:255–8. DOI: 10.1016/j.transproceed.2012.05.090. PMID: 23375311.4. Marwan IK, Fawzy AT, Egawa H, Inomata Y, Uemoto S, Asonuma K, et al. 1999; Innovative techniques for and results of portal vein reconstruction in living-related liver transplantation. Surgery. 125:265–70. DOI: 10.1016/S0039-6060(99)70236-9. PMID: 10076610.5. Mitchell A, John PR, Mayer DA, Mirza DF, Buckels JA, De Ville De Goyet J. 2002; Improved technique of portal vein reconstruction in pediatric liver transplant recipients with portal vein hypoplasia. Transplantation. 73:1244–7. DOI: 10.1097/00007890-200204270-00009. PMID: 11981415.6. Takahashi Y, Nishimoto Y, Matsuura T, Hayashida M, Tajiri T, Soejima Y, et al. 2009; Surgical complications after living donor liver transplantation in patients with biliary atresia: a relatively high incidence of portal vein complications. Pediatr Surg Int. 25:745–51. DOI: 10.1007/s00383-009-2430-y. PMID: 19655151.7. Ueda M, Egawa H, Ogawa K, Uryuhara K, Fujimoto Y, Kasahara M, et al. 2005; Portal vein complications in the long-term course after pediatric living donor liver transplantation. Transplant Proc. 37:1138–40. DOI: 10.1016/j.transproceed.2005.01.044. PMID: 15848648.8. Kuang AA, Renz JF, Ferrell LD, Ring EJ, Rosenthal P, Lim RC, et al. 1996; Failure patterns of cryopreserved vein grafts in liver transplantation. Transplantation. 62:742–7. DOI: 10.1097/00007890-199609270-00007. PMID: 8824470.9. Sugawara Y, Makuuchi M, Tamura S, Matsui Y, Kaneko J, Hasegawa K, et al. 2006; Portal vein reconstruction in adult living donor liver transplantation using cryopreserved vein grafts. Liver Transpl. 12:1233–6. DOI: 10.1002/lt.20786. PMID: 16724339.10. Namgoong JM, Hwang S, Ko GY, Park GC, Kim KM, Oh SH. 2023; Endovascular stenting for late-onset stricture of interposed portal vein conduit following pediatric liver transplantation. Ann Liver Transplant. 3:29–34. DOI: 10.52604/alt.23.0007.11. Alfares BA, Bokkers RP, Verkade HJ, Dierckx RA, Gupte G, Franchi-Abella S, et al. 2021; Portal vein obstruction after pediatric liver transplantation: a systematic review of current treatment strategies. Transplant Rev (Orlando). 35:100630. DOI: 10.1016/j.trre.2021.100630. PMID: 34107368.12. Ueno T, Toyama C, Deguchi K, Masahata K, Nomura M, Watanabe M, et al. 2022; Long-term outcome of portal vein stenting after pediatric living donor liver transplantation. Transplant Proc. 54:454–6. DOI: 10.1016/j.transproceed.2022.01.008. PMID: 35148883.13. Bukova M, Funken D, Pfister ED, Baumann U, Richter N, Vondran FF, et al. 2022; Long-term outcome of primary percutaneous stent angioplasty for pediatric posttransplantation portal vein stenosis. Liver Transpl. 28:1463–74. DOI: 10.1002/lt.26488. PMID: 35447015.14. Ko GY, Sung KB, Lee S, Yoon HK, Kim KR, Kim KM, et al. 2007; Stent placement for the treatment of portal vein stenosis or occlusion in pediatric liver transplant recipients. J Vasc Interv Radiol. 18:1215–21. DOI: 10.1016/j.jvir.2007.06.029. PMID: 17911510.15. Namgoong JM, Hwang S, Yoon YI, Cho YP, Kang WH, Kwon YJ, et al. 2021; Third retransplantation using a whole liver graft for late graft failure from hepatic vein stent stenosis in a pediatric patient who underwent split liver retransplantation. Ann Hepatobiliary Pancreat Surg. 25:299–306. DOI: 10.14701/ahbps.2021.25.2.299. PMID: 34053936. PMCID: PMC8180402.16. Moon DB, Lee SG, Chung YK, Kang WH, Kim KH, Song GW, et al. 2021; Over 500 liver transplants including more than 400 living-donor liver transplants in 2019 at Asan Medical Center. Transplant Proc. 53:83–91. DOI: 10.1016/j.transproceed.2020.08.027. PMID: 33010937.17. Hwang S, Ha TY, Ahn CS, Moon DB, Kim KH, Song GW, et al. 2016; Standardized surgical techniques for adult living donor liver transplantation using a modified right lobe graft: a video presentation from bench to reperfusion. Korean J Hepatobiliary Pancreat Surg. 20:97–101. DOI: 10.14701/kjhbps.2016.20.3.97. PMID: 27621745. PMCID: PMC5018955.18. Hwang S, Bae JH, Kim IO, Hong JJ. 2021; Current vascular allograft procurement, cryopreservation and transplantation techniques in the Asan Medical Center Tissue Bank. Ann Liver Transplant. 1:79–85. DOI: 10.52604/alt.21.0016.19. Feng M, Wan P, Qiu B, Zhou T, Luo Y, Gu L, et al. 2018; Improved portal vein venoplasty with an autogenous patch in pediatric living donor liver transplantation. Liver Transpl. 24:1084–90. DOI: 10.1002/lt.25011. PMID: 29328523.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Modified patch-conduit venoplasty for hypoplastic portal vein in pediatric liver transplantation
- Tailored standardization of portal vein reconstruction for pediatric liver transplantation at Asan Medical Center
- Clinical applicability of autologous great saphenous vein for living donor liver transplantation
- Wedged-patch venoplasty for graft left portal vein in pediatric living donor liver transplantation
- Usability of cryopreserved homologous great saphenous vein for hepatobiliarypancreatic surgery and living donor liver transplantation