J Cerebrovasc Endovasc Neurosurg.
2023 Dec;25(4):462-467. 10.7461/jcen.2023.E2023.01.002.
Intra-aneurysmatic thrombectomy in a distal anterior cerebral artery aneurysm
- Affiliations
-
- 1Department of Neurosurgery, National Institute of Neurology and Neurosurgery, Mexico City, Mexico
- KMID: 2549453
- DOI: http://doi.org/10.7461/jcen.2023.E2023.01.002
Abstract
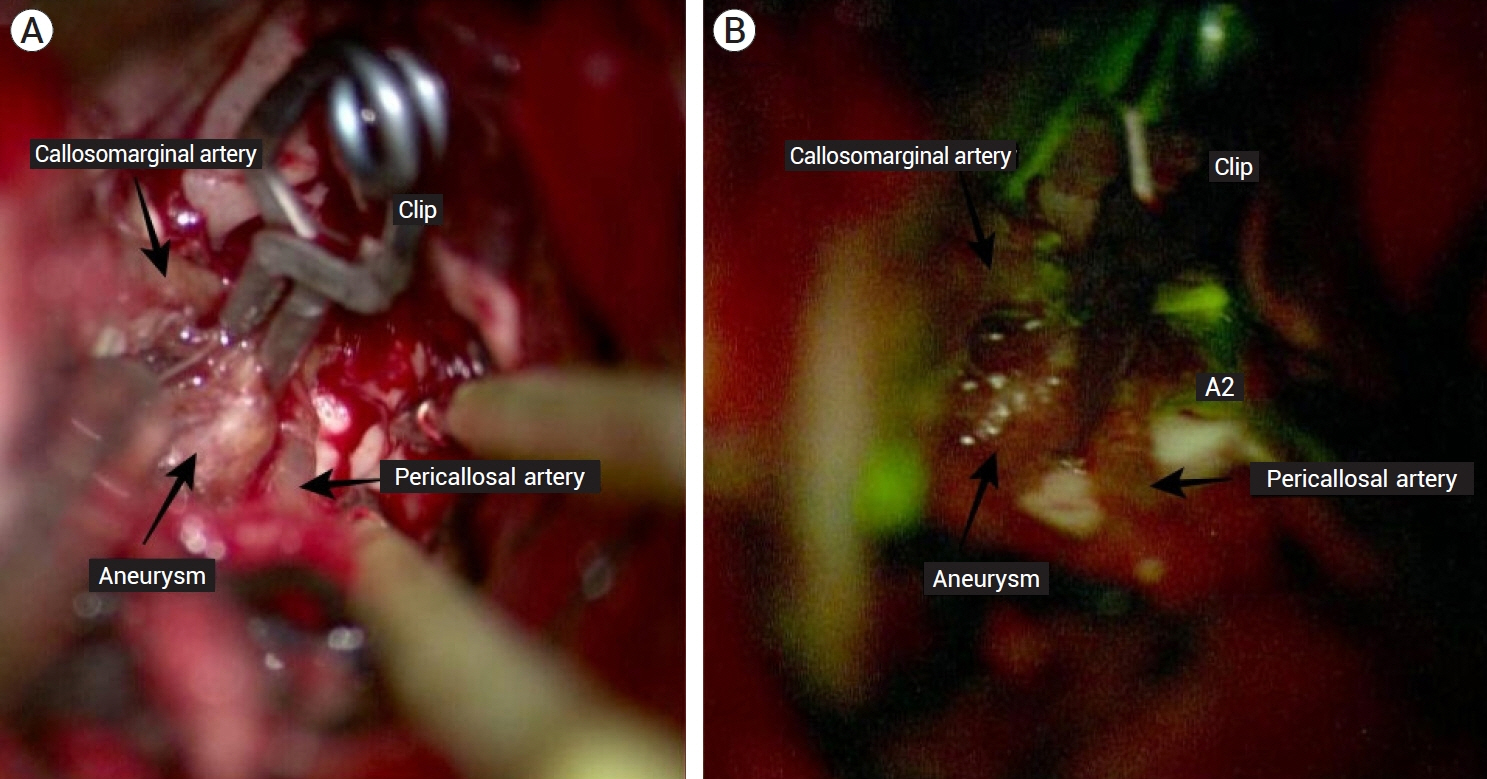
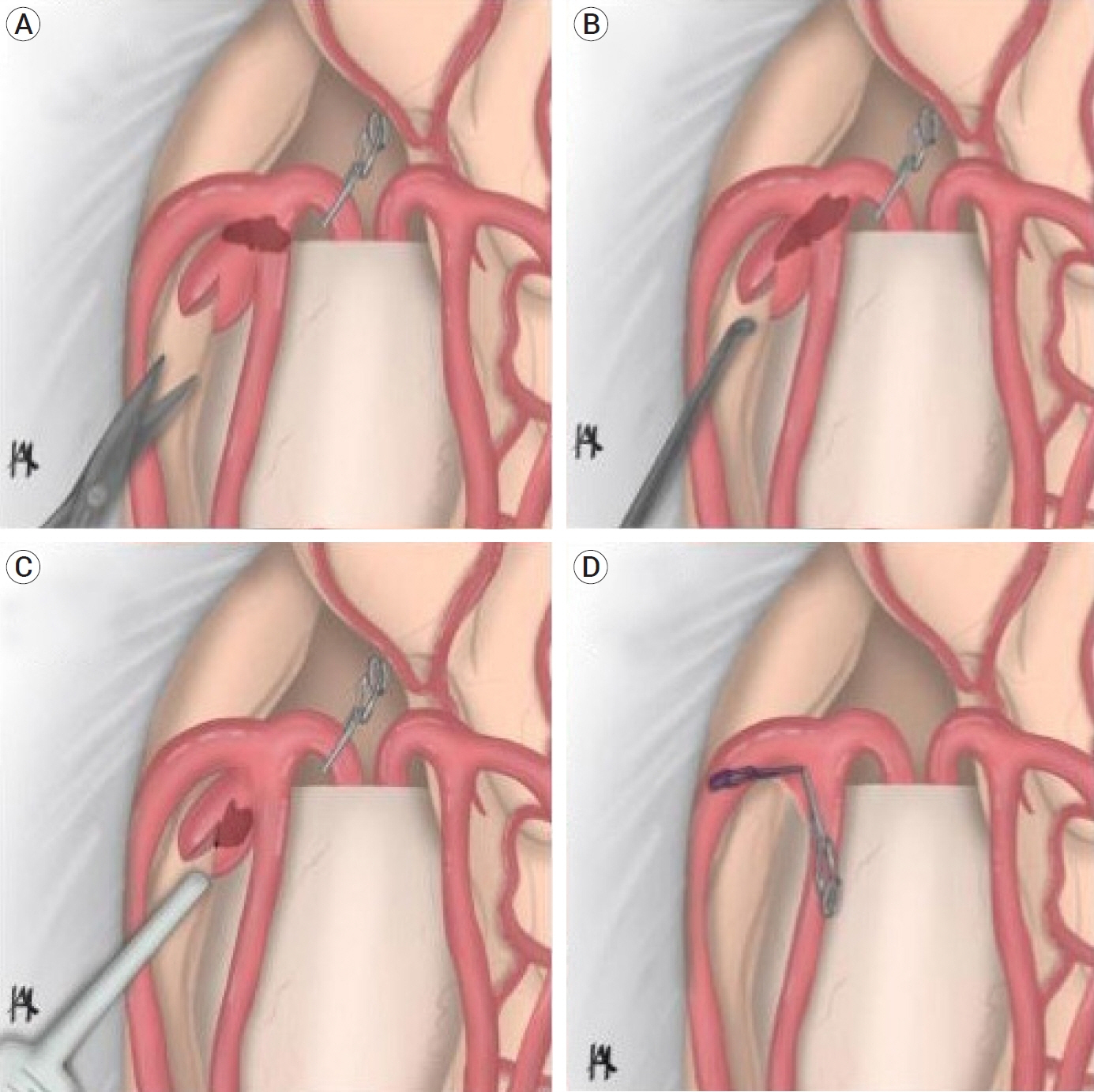
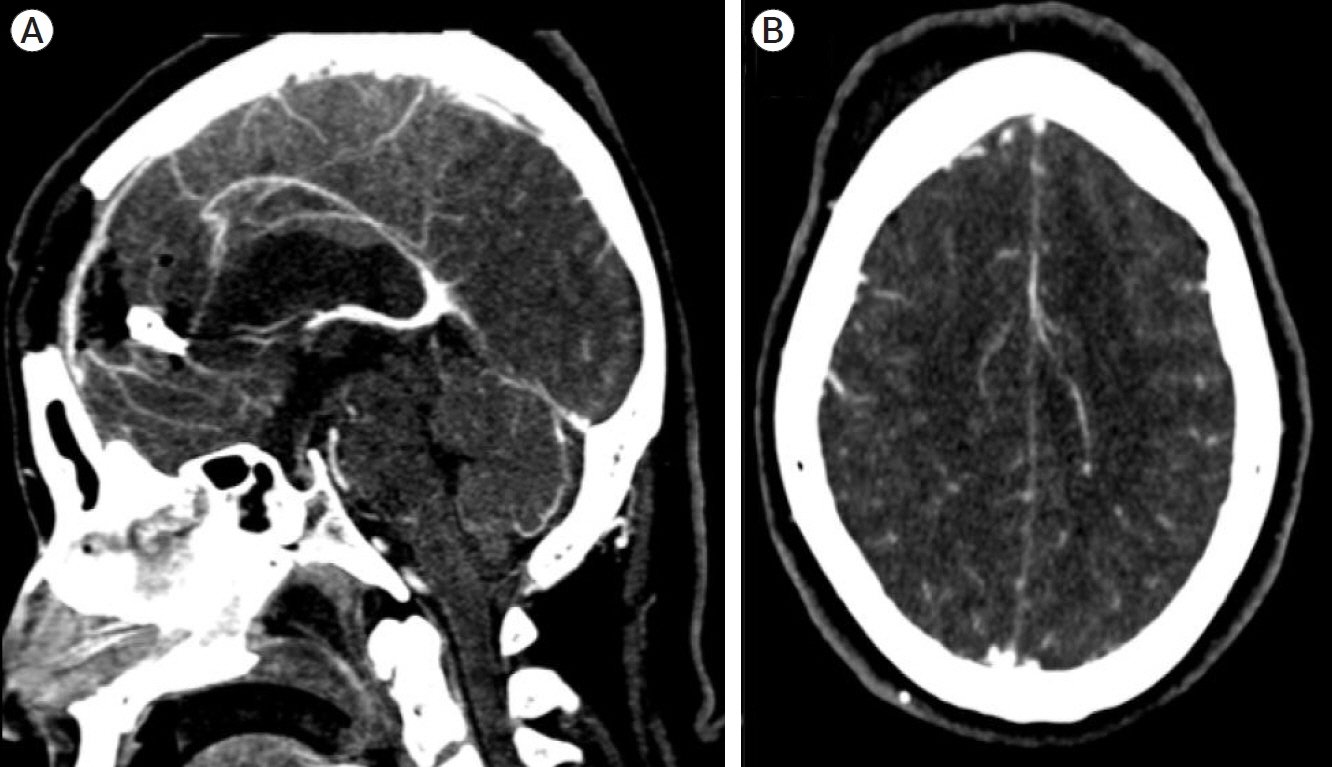
- Thrombectomy procedures following intra-aneurysmatic lesions are extremely rare, and few cases have been reported. This article describes a microsurgical intra-aneurysmatic thrombectomy (MIaT) for a distal anterior cerebral artery (DACA) aneurysm. We present the case of a 48-year-old female that was admitted to the emergency room, showing neurologic deterioration with focal deficits. A computed tomography angiography (CTA) scan revealed an aneurysm located in the distal segment of the left anterior cerebral artery. During the surgical procedure, after clipping, a wellformed clot was visualized through the aneurysm’s wall obstructing the left DACA flow. We proceeded to open the aneurysm’s dome to remove the thrombus and clip the aneurysm neck, re-establishing the flow of the left DACA. Intra-aneurysmatic thrombosis can occur as a complication during clipping, obstructing the distal flow of vital arteries and causing fatal results in the patient’s postoperative status. MIaT is a good technique for restoring the flow of the affected vessel and allows a secure aneurysm clipping after thrombus removal.
Figure
Reference
-
1. Ahn JH, Jun HS, Song JH, Cho BM, Lee HK, Kim BC, et al. Rescue mechanical thrombectomy using a retrievable stent for thromboembolic occlusion occurring during coil embolization of ruptured intracranial aneurysms. J Neurointerv Surg. 2017; Mar. 9(3):244–9.2. Briganti F, Leone G, Marseglia M, Chiaramonte C, Solari D, Caranci F, et al. Mechanical thrombectomy in the treatment of distal occlusions during coil embolization of ruptured intracranial aneurysms. NMC Case Rep J. 2016; Sep. 3(4):115–7.3. Harada K, Kurokawa T, Kato S, Ishihara H, Saka M, Oka F, et al. Operative open intra-aneurysmal thrombectomy for ruptured cerebral aneurysm and peripheral ischemia associated with vasospasm. J Clin Neurosci. 2010; Apr. 17(4):517–20.4. Hirata K, Yamazaki T, Kato N, Yasuda S, Matsumura A. Mechanical thrombectomy for occlusion near a ruptured intracranial aneurysm: A case report. Surg Neurol Int. 2020; May. 11:120.5. Hirano Y, Ono H, Inoue T, Mitani T, Tanishima T, Tamura A, et al. Emergent surgical embolectomy for middle cerebral artery occlusion related to cerebral angiography followed by neck clipping for an unruptured aneurysm in the anterior communicating artery. Surg Neurol Int. 2020; Dec. 11:420.6. Horiuchi T, Nitta J, Miyaoka Y, Nagm A, Tsutsumi K, Ito K, et al. Open embolectomy of large vessel occlusion in the endovascular era: Results of a 12-year single-center experience. World Neurosurg. 2017; Jun. 102:65–71.7. Kheĭreddin AS, Filatov IuM. Microsurgical treatment of partially thrombosed giant cerebral aneurysms--technique of endoaneurysmal thrombectomy. Zh Vopr Neirokhir Im N N Burdenko. (Russian). 2008; Oct-Dec. (4):49–51. discussion 51.8. Lehecka M, Dashti R, Lehto H, Kivisaari R, Niemelä M, Hernesniemi J. Distal anterior cerebral artery aneurysms. Acta Neurochir Suppl. 2010; 107:15–26.9. Pfaff J, Herweh C, Pham M, Schieber S, Ringleb PA, Bendszus M, et al. Mechanical thrombectomy of distal occlusions in the anterior cerebral artery: Recanalization rates, periprocedural complications, and clinical outcome. AJNR Am J Neuroradiol. 2016; Apr. 37(4):673–8.10. Sugita M, Kinouchi H, Nishiyama Y, Kanemaru K, Yoshioka H, Horikoshi T. Direct clipping of a thrombosed giant cerebral aneurysm after thrombectomy without bleeding to minimize the temporary occlusion time: Technical case report. Neurol Med Chir (Tokyo). 2009; Dec. 49(12):600–3.11. Singh J, Wolfe SQ. Stent retriever thrombectomy with aneurysm in target vessel: Technical note. Interv Neuroradiol. 2016; Oct. 22(5):544–7.12. Suzuki T, Kaku S, Nishimura K, Teshigawara A, Sasaki Y, Aoki K, et al. Multistage “hybrid” (open and endovascular) surgical treatment of vertebral artery-thrombosed giant aneurysm by trapping and thrombectomy. World Neurosurg. 2018; Jun. 114:144–50.13. Uno J, Kameda K, Otsuji R, Ren N, Nagaoka S, Kazushi M, et al. Mechanical thrombectomy for acute anterior cerebral artery occlusion. World Neurosurg. 2018; Dec. 120:e957–61.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Multiple Aneurysms of the Distal Anterior Cerebral Artery: Case Report
- Interhemispheric Approach for Intracranial Aneurysms
- Surgical Management of the Distal Anterior Cerebral Artery Aneurysms
- Ruptured proximal anterior cerebral artery (A1) aneurysm located at an anomalous branching of the fronto-orbital artery--a case report
- Microsurgical anatomy of the Anterior Cerebral-anterior Communicating Artery