J Cerebrovasc Endovasc Neurosurg.
2023 Dec;25(4):452-461. 10.7461/jcen.2023.E2022.10.011.
Endovascular treatment for anterior inferior cerebellar artery-posterior inferior cerebellar artery (AICA-PICA) common trunk variant aneurysms: Technical note and literature review
- Affiliations
-
- 1Division of Neurosurgery, Sunnybrook Health Sciences Centre, University of Toronto, Toronto, ON, Canada
- 2Department of Pathology, Stanford School of Medicine, Stanford University Medical Centre, Stanford, CA, USA
- 3Department of Neurosurgery, Trauma Center, Gamma Knife Center, Cannizzaro Hospital, Catania, Italy
- 4Department of Radiology, Health Sciences North, Northern Ontario School of Medicine University, Sudbury, ON, Canada
- 5Division of Neurosurgery, Health Sciences North, Northern Ontario School of Medicine University, Sudbury, ON, Canada
- 6Department of Neurosurgery, Neurosurgery Clinic, Birgunj, Nepal
- KMID: 2549452
- DOI: http://doi.org/10.7461/jcen.2023.E2022.10.011
Abstract
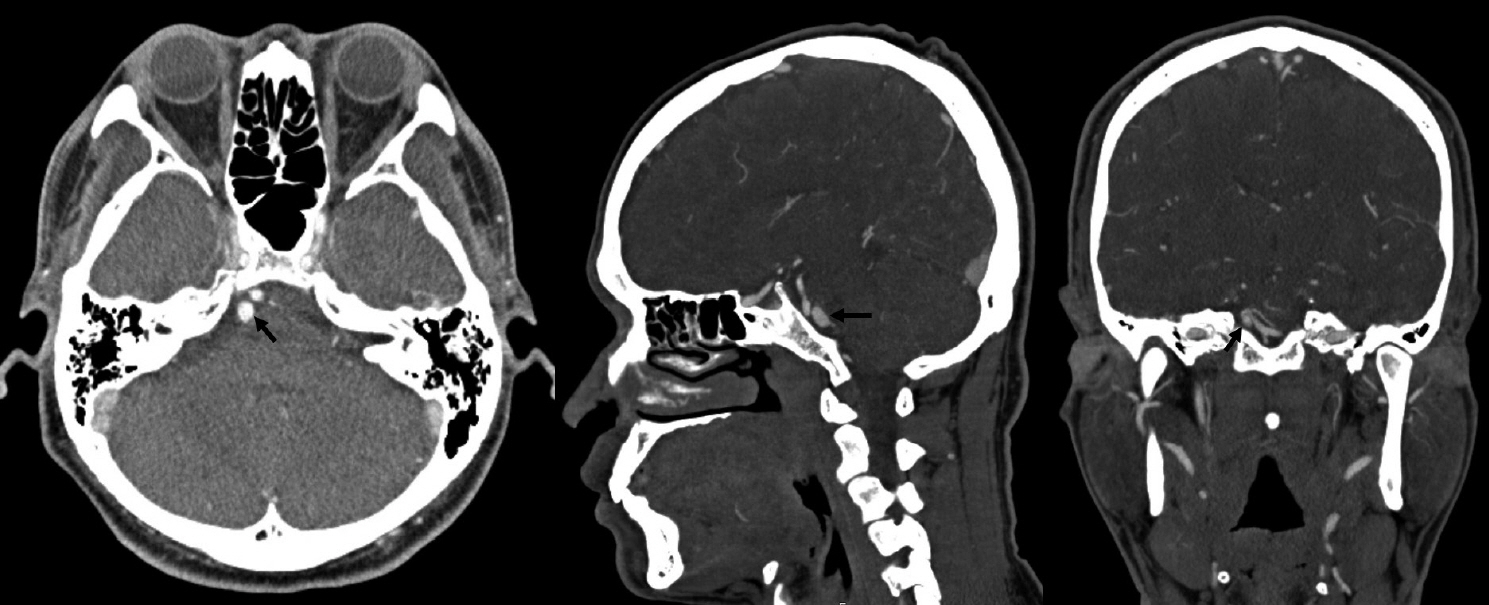
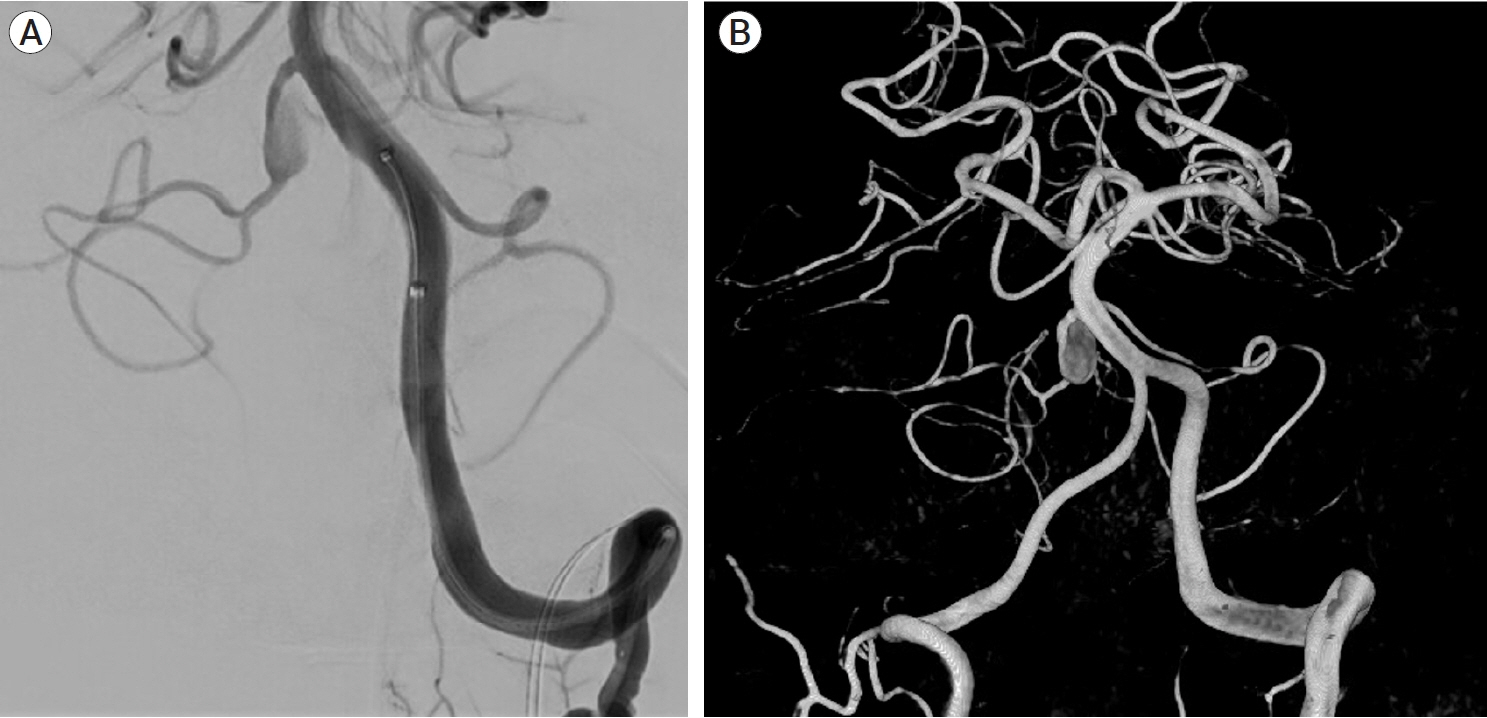
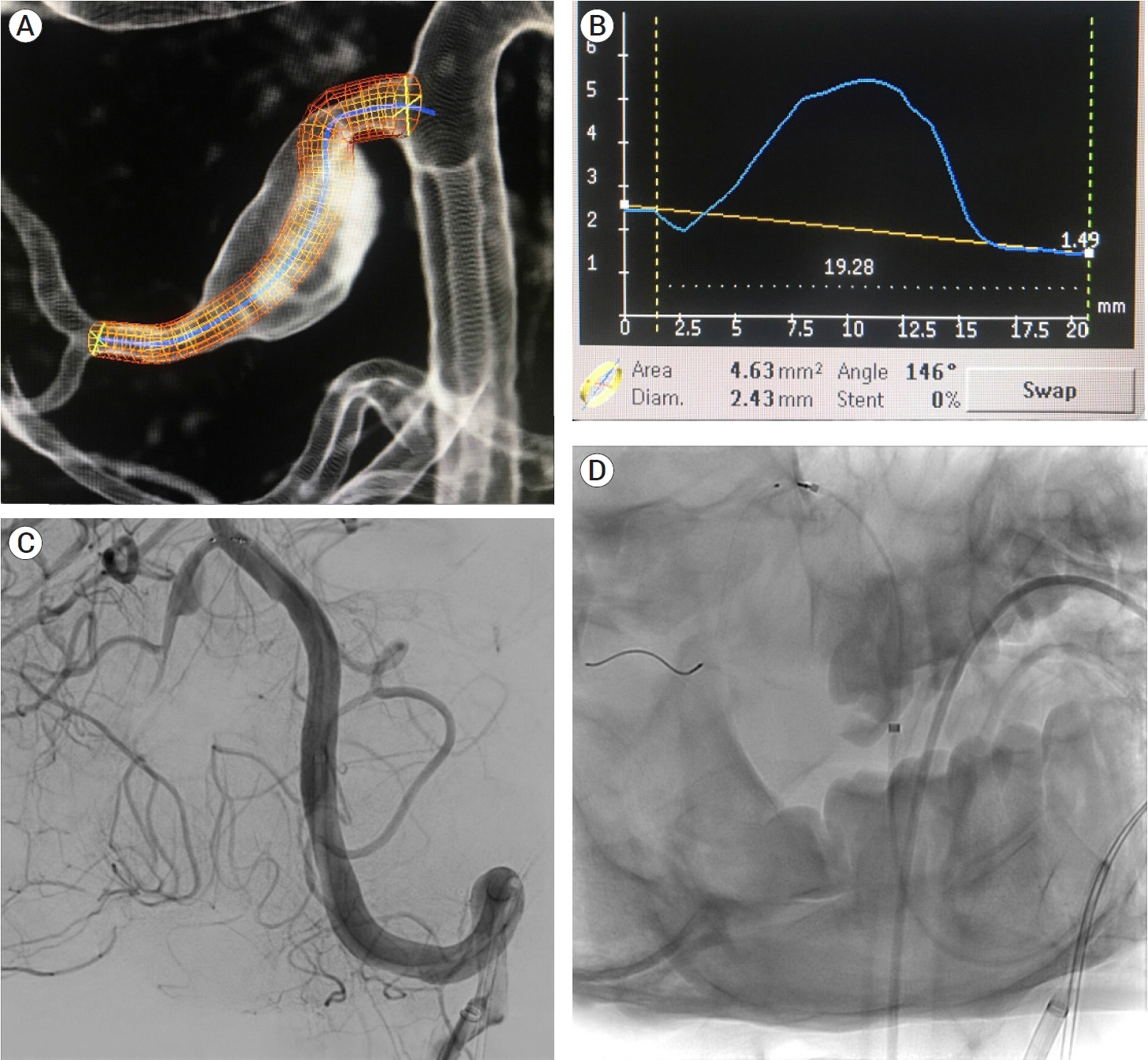
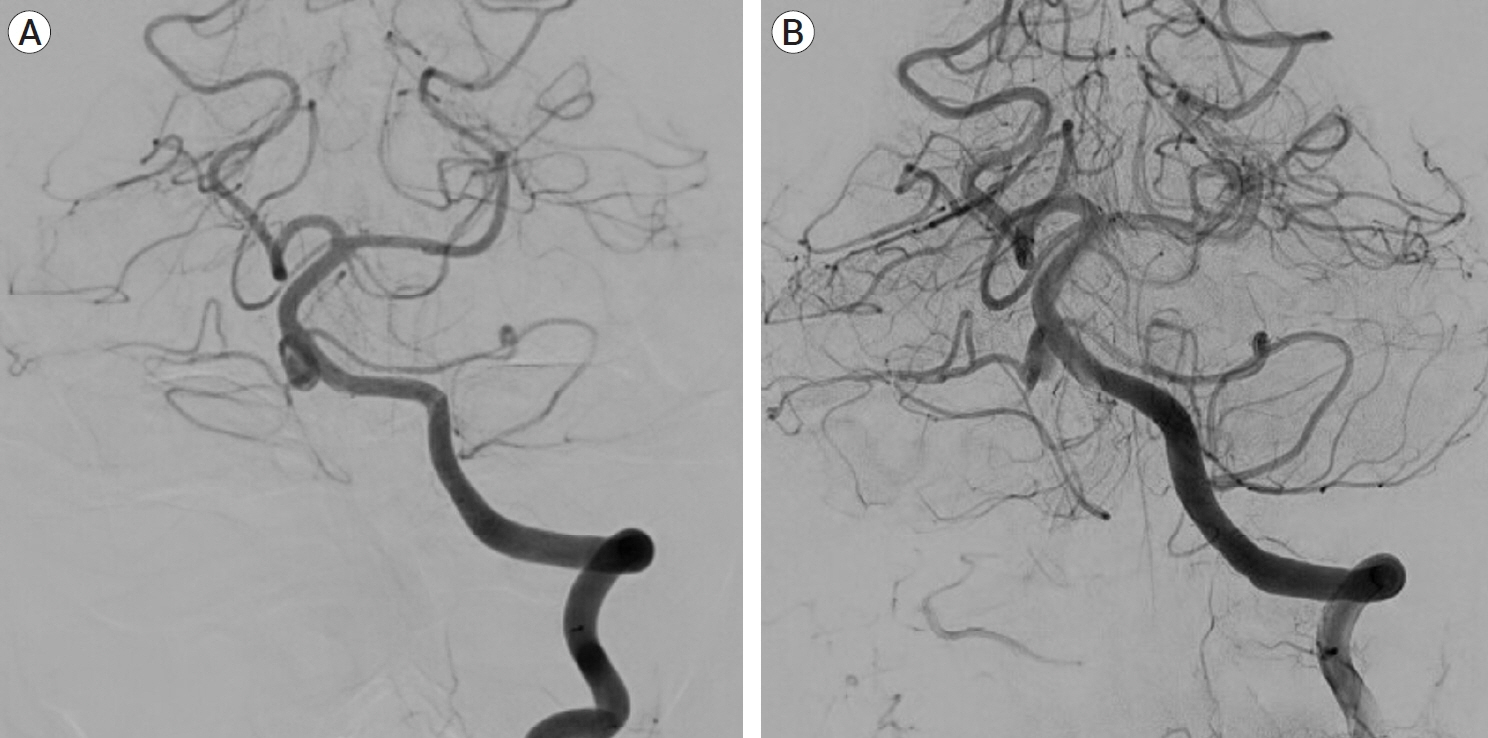
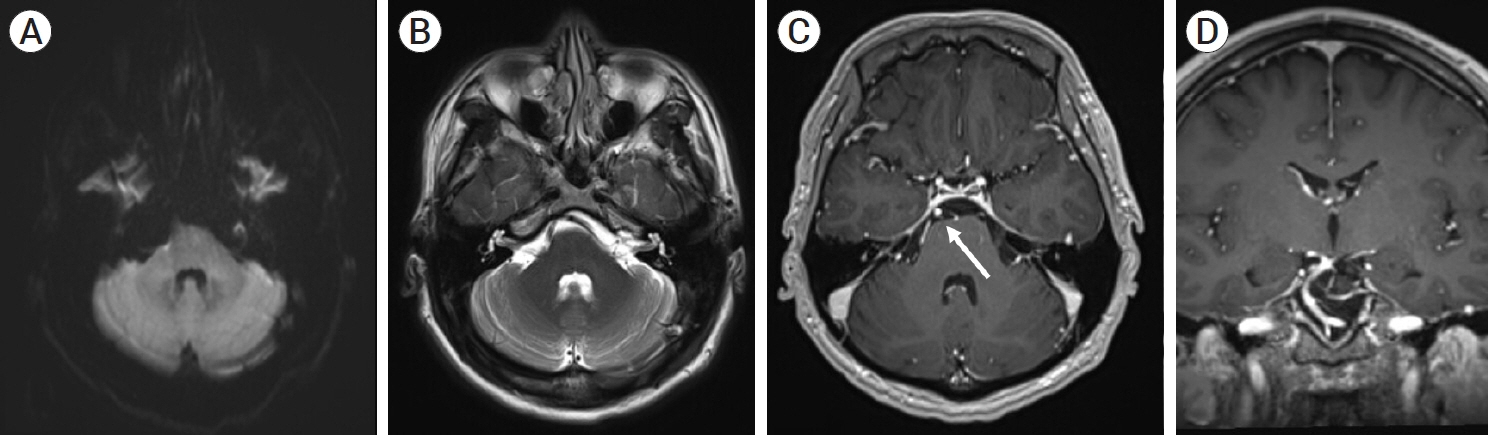
- The Anterior Inferior Cerebellar Artery-Posterior Inferior Cerebellar Artery (AICA-PICA) common trunk is a rare variant of cerebral posterior circulation in which a single vessel originating from either the basilar or vertebral arteries supplies both cerebellum and brainstem territories. We present the first case of an unruptured right AICA-PICA aneurysm treated with flow diversion using a Shield-enhanced pipeline endovascular device (PED, VANTAGE Embolization Device with Shield Technology, Medtronic, Canada). We expand on this anatomic variant and review the relevant literature. A 39-year-old man presented to our treatment center with vertigo and right hypoacusis. The initial head CT/CTA was negative, but a 4-month follow-up MRI revealed a 9 mm fusiform dissecting aneurysm of the right AICA. The patient underwent a repeat head CTA and cerebral angiogram, which demonstrated the presence of an aneurysm on the proximal portion of an AICA-PICA anatomical variant. This was treated with an endovascular approach that included flow diversion via a PED equipped with Shield Technology. The patient’s post-procedure period was uneventful, and he was discharged home after two days with an intact neurological status. The patient is still asymptomatic after a 7-month follow-up, with MR angiogram evidence of stable aneurysm obliteration and no ischemic lesions. Aneurysms of the AICA-PICA common trunk variants have a high morbidity risk due to the importance and extent of the territory vascularized by a single vessel. Endovascular treatment with flow diversion proved to be both safe and effective in obliterating unruptured cases.
Figure
Cited by 1 articles
-
Transcranial Doppler emboli monitoring for stroke prevention after flow diverting stents
Matias Costa, Paul Schmitt, Jaleel N, Matias Baldoncini, Juan Vivanco-Suarez, Bipin Chaurasia, Colleen Douville, Loh Yince, Akshal Patel, Stephen Monteith
J Cerebrovasc Endovasc Neurosurg. 2024;26(1):23-29. doi: 10.7461/jcen.2023.E2023.05.002.
Reference
-
1. Ansari A, Rahman A, Ahmed N, Hossain ABMM, Samadder S, Arifin MS, et al. Co-existence of arterio-venous malformation and saccular bifurcation aneurysm of a 48 years old patient, presented with massive intracranial hemorrhage: case report. J Neurol Stroke. 2019; 9(4):189–94.2. Ansari KA, Menon G, Nair S, Abraham M. Aneurysm of anterior inferior cerebellar artery-posterior inferior cerebellar artery variant. Asian J Neurosurg. 2018; Jan-Mar. 13(1):53–5.3. Anxionnat R, Tonnelet R, Derelle AL, Liao L, Barbier C, Bracard S. Endovascular treatment of ruptured intracranial aneurysms: indications, techniques and results. Diagn Interv Imaging. 2015; Jul-Aug. 96(7-8):667–75.4. Atasoy D, Kandasamy N, Hart J, Lynch J, Yang SH, Walsh D, et al. Outcome study of the pipeline embolization device with shield technology in unruptured aneurysms (PEDSU). AJNR Am J Neuroradiol. 2019; Dec. 40(12):2094–101.5. Backes D, Rinkel GJE, Laban KG, Algra A, Vergouwen MDI. Patient- and aneurysm-specific risk factors for intracranial aneurysm growth. Stroke. 2016; Apr. 47(4):951–7.6. Backes D, Vergouwen MDI, Tiel Groenestege AT, Bor ASE, Velthuis BK, Greving JP, et al. PHASES score for prediction of intracranial aneurysm growth. Stroke. 2015; May. 46(5):1221–6.7. Başkaya MK, Coscarella E, Jea A, Morcos JJ. Aneurysm of the anterior inferior cerebellar artery-posterior inferior cerebellar artery variant: case report with anatomical description in the cadaver. Neurosurgery. 2006; Feb. 58(2):e388.8. Briganti F, Leone G, Marseglia M, Mariniello G, Caranci F, Brunetti A, et al. Endovascular treatment of cerebral aneurysms using flow-diverter devices: a systematic review. Neuroradiol J. 2015; Aug. 28(4):365–75.9. Brinjikji W, Murad MH, Lanzino G, Cloft HJ, Kallmes DF. Endovascular treatment of intracranial aneurysms with flow diverters: a meta-analysis. Stroke. 2013; Feb. 44(2):442–7.10. Brinjikji W, Zhu YQ, Lanzino G, Cloft HJ, Murad MH, Wang Z, et al. Risk factors for growth of intracranial aneurysms: a systematic review and meta-analysis. AJNR Am J Neuroradiol. 2016; Apr. 37(4):615–20.11. Chowdhury D, Ahmed N, Chaurasia B, Barua KK. Azygos anterior cerebral artery aneurysm with subarachnoid hemorrhage. Neuroimmunology and Neuroinflammation. 2018; Sep. 5(9):39.12. Ebara M, Tanaka T, Sawauchi S, Morooka S, Yuhki K, Abe T. A ruptured aneurysm of the anterior and posterior inferior cerebellar artery: a case report. No Shinkei Geka. 1999; Nov. 27(11):1013–7.13. Eliezer M, Verillaud B, Guichard JP, Kania R, Toupet M, Herman P, et al. Labyrinthine infarction caused by vertebral artery dissection: consideration based on MRI. J Neurol. 2019; Oct. 266(10):2575–7.14. Fujii K, Lenkey C, Rhoton AL. Microsurgical anatomy of the choroidal arteries. Fourth ventricle and cerebellopontine angles. J Neurosurg. 1980; Apr. 52(4):504–24.15. Fukushima S, Hirohata M, Okamoto Y, Yamashita S, Ishida S, Shigemori M. Anterior inferior cerebellar artery dissecting aneurysm in a juvenile: case report. Neurol Med Chir (Tokyo). 2009; Feb. 49(2):81–4.16. Girdhar G, Andersen A, Pangerl E, Jahanbekam R, Ubl S, Nguyen K, et al. Thrombogenicity assessment of Pipeline Flex, Pipeline Shield, and FRED flow diverters in an in vitro human blood physiological flow loop model. J Biomed Mater Res A. 2018; Dec. 106(12):3195–202.17. Gonzalez LF, Alexander MJ, McDougall CG, Spetzler RF. Anteroinferior cerebellar artery aneurysms: surgical approaches and outcomes—a review of 34 cases. Neurosurgery. 2004; Nov. 55(5):1025–35.18. Gopalakrishnan CV, Menon G, Nair S. Aneurysm of the anterior inferior cerebellar artery-posterior inferior cerebellar artery variant: two case reports and review of literature. Br J Neurosurg. 2009; 23(5):554–6.19. Griessenauer CJ, Ogilvy CS, Adeeb N, Dmytriw AA, Foreman PM, Shallwani H, et al. Pipeline embolization of posterior circulation aneurysms: a multicenter study of 131 aneurysms. J Neurosurg. 2018; May. 130(3):923–35.20. Gross BA, Frerichs KU, Du R. Microsurgical treatment of a ruptured dissecting labyrinthine artery aneurysm. Clin Neurol Neurosurg. 2013; Oct. 115(10):2277–9.21. Hou K, Li G, Luan T, Xu K, Xu B, Yu J. Anatomical study of anterior inferior cerebellar artery and its reciprocal relationship with posterior inferior cerebellar artery based on angiographic data. World Neurosurg. 2020; Jan. 133:e459–72.22. Kalani MYS, Yashar S, Ramey W, Albuquerque FC, McDougall CG, Nakaji P, et al. Revascularization and aneurysm surgery: techniques, indications, and outcomes in the endovascular era. Neurosurgery. 2014; 74(5):482–98.23. Kusaka N, Maruo T, Nishiguchi M, Takayama K, Maeda Y, Ogihara K, et al. Embolization for aneurysmal dilatation associated with ruptured dissecting anterior inferior cerebellar artery aneurysm with preservation of the parent artery: case report. No Shinkei Geka. 2006; Jul. 34(7):729–34.24. Lister RJ, Rhoton AL, Matsushima T, Peace DA. Microsurgical anatomy of the posterior inferior cerebellar artery. Neurosurgery. 1982; Feb. 10(2):170–99.25. Lv X, Yang H, Liu P, Li Y. Flow-diverter devices in the treatment of intracranial aneurysms: a meta-analysis and systematic review. Neuroradiol J. 2016; Feb. 29(1):66–71.26. Madaelil TP, Moran CJ, Cross DT 3rd, Kansagra AP. Flow diversion in ruptured intracranial aneurysms: a meta-analysis. AJNR Am J Neuroradiol. 2017; Mar. 38(3):590–5.27. Manning NW, Cheung A, Phillips TJ, Wenderoth JD. Pipeline shield with single antiplatelet therapy in aneurysmal subarachnoid haemorrhage: multicentre experience. J Neurointerv Surg. 2019; Jul. 11(7):694–8.28. Martin RG, Grant JL, Peace D, Theiss C, Rhoton AL. Microsurgical relationships of the anterior inferior cerebellar artery and the facial-vestibulocochlear nerve complex. Neurosurgery. 1980; May. 6(5):483–507.29. Menovsky T, André Grotenhuis J, Bartels RHMA. Aneurysm of the anterior inferior cerebellar artery (AICA) associated with high-flow lesion: report of two cases and review of literature. J Clin Neurosci. 2002; Mar. 9(2):207–11.30. Munich SA, Tan LA, Keigher KM, Chen M, Moftakhar R, Lopes DK. The pipeline embolization device for the treatment of posterior circulation fusiform aneurysms: lessons learned at a single institution. J Neurosurg. 2014; Nov. 121(5):1077–84.31. Nagahata M, Hosoya T, Fuse T, Aoyagi M, Yamaguchi K. Arterial dissection of the vertebrobasilar systems: a possible cause of acute sensorineural hearing loss. Am J Otol. 1997; Jan. 18(1):32–8.32. Ooigawa H, Morikawa E, Ishihara S, Ogura T, Takeda R, Kurita H. Partially thrombosed giant aneurysm arising from a distal anterior inferior cerebellar artery–posterior inferior cerebellar artery variant: a case report. Interdisciplinary Neurosurgery. 2015; 2(3):123–5.33. Pasarikovski CR, Waggass G, Cardinell J, Howard P, da Costa L, Yang VX. Pipeline embolisation device with shield technology for the treatment of ruptured intracranial aneurysm. Neuroradiol J. 2019; Jun. 32(3):189–92.34. Peluso JPP, van Rooij WJ, Sluzewski M, Beute GN. Distal aneurysms of cerebellar arteries: incidence, clinical presentation, and outcome of endovascular parent vessel occlusion. AJNR Am J Neuroradiol. 2007; Sep. 28(8):1573–8.35. Petr O, Brinjikji W, Thomé C, Lanzino G. Safety and efficacy of microsurgical treatment of previously coiled aneurysms: a systematic review and meta-analysis. Acta Neurochir (Wien). 2015; Oct. 157(10):1623–32.36. Rhoton AL. The cerebellar arteries. Neurosurgery. 2000; 47:S29–68.37. Sato H, Kawagishi K. Labyrinthine artery detection in patients with idiopathic sudden sensorineural hearing loss by 7-T MRI. Otolaryngol Neck Surg. 2014; Mar. 150(3):455–9.38. Srinivasan VM, Shlobin NA, Karahalios K, Scherschinski L, Rahmani R, Graffeo CS, et al. Adoption of advanced microneurosurgical technologies: an international survey. World Neurosurg. 2022; Jan. 157:e473–83.39. Suh SH, Kim DJ, Kim DI, Kim BM, Chung TS, Hong CK, et al. Management of anterior inferior cerebellar artery aneurysms: endovascular treatment and clinical outcome. AJNR Am J Neuroradiol. 2011; Jan. 32(1):159–64.40. Takahashi M, Wilson G, Hanafee W. The anterior inferior cerebellar artery: its radiographic anatomy and significance in the diagnosis of extra-axial tumors of the posterior fossa. Radiology. 1968; 90(2):281–7.41. Takeuchi S, Takasato Y, Masaoka H, Hayakawa T, Otani N, Yoshino Y, et al. Trapping of ruptured dissecting aneurysm of distal anterior inferior cerebellar artery--case report. Brain Nerve. 2009; Feb. 61(2):203–7.42. Tumialán LM, Zhang YJ, Cawley CM, Dion JE, Tong FC, Barrow DL. Intracranial hemorrhage associated with stent-assisted coil embolization of cerebral aneurysms: a cautionary report. J Neurosurg. 2008; Jun. 108(6):1122–9.43. Wu X, Tian Z, Liu J, Zhang Y, Li W, Zhang Y, et al. Patency of posterior circulation branches covered by flow diverter device: a hemodynamic study. Front Neurol. 2019; Jun. 10:658.44. Zager EL, Shaver EG, Hurst RW, Flamm ES. Distal anterior inferior cerebellar artery aneurysms. J Neurosurg. 2002; Sep. 97(3):692–6.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment Results of Posterior Inferior Cerebellar Artery Aneurysms
- Aneurysm of the Posterior Inferior Cerebellar Artery: Clinical Features and Surgical Results
- The Clinical Presentation and Treatment of Distal Posterior Inferior Cerebellar artery Aneurysms: Report on 2 cases
- Neuro-otological aspects of cerebellar stroke
- Simultaneous Vertebral Artery Dissection and Contralateral Posterior Inferior Cerebellar Artery Dissecting Aneurysm