J Korean Med Sci.
2023 Dec;38(47):e348. 10.3346/jkms.2023.38.e348.
Clinical Course of Patients With Mediastinal Lymph Node Tuberculosis and Risk Factors for Paradoxical Responses
- Affiliations
-
- 1Division of Pulmonary and Critical Care Medicine, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Division of Pulmonary and Allergy, Department of Internal Medicine, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul, Korea
- 3Department of Laboratory Medicine and Genetics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 4Department of Pathology and Translational Genomics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2548799
- DOI: http://doi.org/10.3346/jkms.2023.38.e348
Abstract
- Background
Paradoxical responses (PR) occur more frequently in lymph node tuberculosis (LNTB) than in pulmonary tuberculosis and present difficulties in differential diagnosis of drug resistance, new infection, poor patient compliance, and adverse drug reactions. Although diagnosis of mediastinal LNTB has become much easier with the development of endosonography, limited information is available. The aim of this study was to investigate the clinical course of mediastinal LNTB and the risk factors associated with PR.
Methods
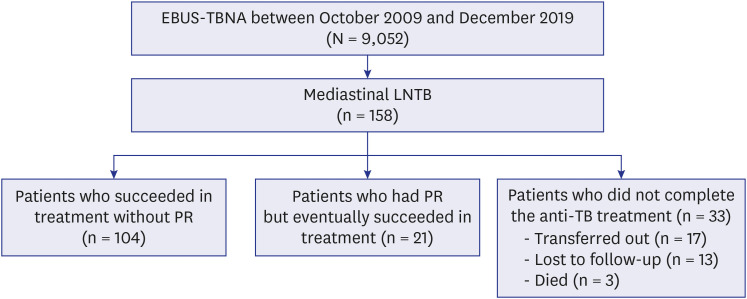
Patients diagnosed with mediastinal LNTB via endosonography were evaluated retrospectively between October 2009 and December 2019. Multivariable logistic regression was applied to evaluate the risk factors associated with PR.
Results
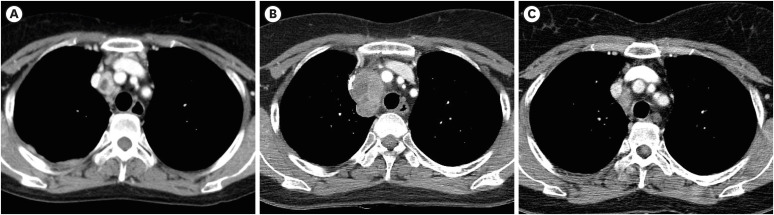
Of 9,052 patients who underwent endosonography during the study period, 158 were diagnosed with mediastinal LNTB. Of these, 55 (35%) and 41 (26%) concurrently had pulmonary tuberculosis and extrapulmonary tuberculosis other than mediastinal LNTB, respectively. Of 125 patients who completed anti-tuberculosis treatment, 21 (17%) developed PR at a median of 4.4 months after initiation of anti-tuberculosis treatment. The median duration of anti-tuberculosis treatment was 6.3 and 10.4 months in patients without and with PR, respectively. Development of PR was independently associated with age < 55 years (adjusted odds ratio [aOR], 5.72; 95% confidence interval [CI], 1.81–18.14; P = 0.003), lymphocyte count < 800/μL (aOR, 8.59; 95% CI, 1.60–46.20; P = 0.012), and short axis diameter of the largest lymph node (LN) ≥ 16 mm (aOR, 5.22; 95% CI, 1.70–16.00; P = 0.004) at the time of diagnosis of mediastinal LNTB.
Conclusion
As PR occurred in one of six patients with mediastinal LNTB during antituberculosis treatment, physicians should pay attention to patients with risk factors (younger age, lymphocytopenia, and larger LN) at the time of diagnosis.
Figure
Reference
-
1. World Health Organization. Global Tuberculosis Report 2022. Updated 2022. Accessed March 26, 2023. https://www.who.int/publications/i/item/9789240061729 .2. Peto HM, Pratt RH, Harrington TA, LoBue PA, Armstrong LR. Epidemiology of extrapulmonary tuberculosis in the United States, 1993–2006. Clin Infect Dis. 2009; 49(9):1350–1357. PMID: 19793000.
Article3. Gomes T, Reis-Santos B, Bertolde A, Johnson JL, Riley LW, Maciel EL. Epidemiology of extrapulmonary tuberculosis in Brazil: a hierarchical model. BMC Infect Dis. 2014; 14(1):9. PMID: 24400848.
Article4. Breen RA, Smith CJ, Bettinson H, Dart S, Bannister B, Johnson MA, et al. Paradoxical reactions during tuberculosis treatment in patients with and without HIV co-infection. Thorax. 2004; 59(8):704–707. PMID: 15282393.
Article5. Hawkey CR, Yap T, Pereira J, Moore DA, Davidson RN, Pasvol G, et al. Characterization and management of paradoxical upgrading reactions in HIV-uninfected patients with lymph node tuberculosis. Clin Infect Dis. 2005; 40(9):1368–1371. PMID: 15825042.
Article6. Cho OH, Park KH, Kim T, Song EH, Jang EY, Lee EJ, et al. Paradoxical responses in non-HIV-infected patients with peripheral lymph node tuberculosis. J Infect. 2009; 59(1):56–61. PMID: 19535147.
Article7. Cheng SL, Wang HC, Yang PC. Paradoxical response during anti-tuberculosis treatment in HIV-negative patients with pulmonary tuberculosis. Int J Tuberc Lung Dis. 2007; 11(12):1290–1295. PMID: 18034948.8. Ye W, Zhang R, Xu X, Liu Y, Ying K. Diagnostic efficacy and safety of endobronchial ultrasound-guided transbronchial needle aspiration in intrathoracic tuberculosis: a meta-analysis. J Ultrasound Med. 2015; 34(9):1645–1650. PMID: 26269299.
Article9. Um SW, Kim HK, Jung SH, Han J, Lee KJ, Park HY, et al. Endobronchial ultrasound versus mediastinoscopy for mediastinal nodal staging of non-small-cell lung cancer. J Thorac Oncol. 2015; 10(2):331–337. PMID: 25611227.
Article10. Lee KJ, Suh GY, Chung MP, Kim H, Kwon OJ, Han J, et al. Combined endobronchial and transesophageal approach of an ultrasound bronchoscope for mediastinal staging of lung cancer. PLoS One. 2014; 9(3):e91893. PMID: 24632834.
Article11. Seo AN, Park HJ, Lee HS, Park JO, Chang HE, Nam KH, et al. Performance characteristics of nested polymerase chain reaction vs real-time polymerase chain reaction methods for detecting Mycobacterium tuberculosis complex in paraffin-embedded human tissues. Am J Clin Pathol. 2014; 142(3):384–390. PMID: 25125630.
Article12. Ko RE, Jeong BH, Chon HR, Huh HJ, Han J, Lee H, et al. Clinical usefulness of routine AFB culture and MTB PCR of EBUS-TBNA needle rinse fluid. Respirology. 2019; 24(7):667–674. PMID: 30730098.
Article13. Huh HJ, Koh WJ, Song DJ, Ki CS, Lee NY. Evaluation of the Cobas TaqMan MTB test for the detection of Mycobacterium tuberculosis complex according to acid-fast-bacillus smear grades in respiratory specimens. J Clin Microbiol. 2015; 53(2):696–698. PMID: 25428157.
Article14. Diagnostic standards and classification of tuberculosis in adults and children. This official statement of the American Thoracic Society and the Centers for Disease Control and Prevention was adopted by the ATS Board of Directors, July 1999. This statement was endorsed by the Council of the Infectious Disease Society of America, September 1999. Am J Respir Crit Care Med. 2000; 161(4 Pt 1):1376–1395. PMID: 10764337.15. Koh WJ, Ko Y, Kim CK, Park KS, Lee NY. Rapid diagnosis of tuberculosis and multidrug resistance using a MGIT 960 system. Ann Lab Med. 2012; 32(4):264–269. PMID: 22779067.
Article16. Kim S, Lee H, Park HY, Jeon K, Huh HJ, Lee NY, et al. Outcomes of pulmonary tuberculosis in patients with discordant phenotypic isoniazid resistance testing. Respir Med. 2017; 133:6–11. PMID: 29173450.
Article17. Schwartz LH, Bogaerts J, Ford R, Shankar L, Therasse P, Gwyther S, et al. Evaluation of lymph nodes with RECIST 1.1. Eur J Cancer. 2009; 45(2):261–267. PMID: 19091550.
Article18. Lee JY. Diagnosis and treatment of extrapulmonary tuberculosis. Tuberc Respir Dis (Seoul). 2015; 78(2):47–55. PMID: 25861336.
Article19. World Health Organization. Definitions and Reporting Framework for Tuberculosis – 2013 Revision: Updated December 2014 and January 2020. Geneva, Switzerland: World Health Organization;2013.20. Holden IK, Lillebaek T, Andersen PH, Bjerrum S, Wejse C, Johansen IS. Extrapulmonary tuberculosis in Denmark from 2009 to 2014; characteristics and predictors for treatment outcome. Open Forum Infect Dis. 2019; 6(10):ofz388. PMID: 31660351.
Article21. Bewick V, Cheek L, Ball J. Statistics review 13: receiver operating characteristic curves. Crit Care. 2004; 8(6):508–512. PMID: 15566624.22. Zwischenberger JB, Savage C, Alpard SK, Anderson CM, Marroquin S, Goodacre BW. Mediastinal transthoracic needle and core lymph node biopsy: should it replace mediastinoscopy? Chest. 2002; 121(4):1165–1170. PMID: 11948048.
Article23. Bilaçeroğlu S, Günel O, Eriş N, Cağirici U, Mehta AC. Transbronchial needle aspiration in diagnosing intrathoracic tuberculous lymphadenitis. Chest. 2004; 126(1):259–267. PMID: 15249469.
Article24. Hammoud ZT, Anderson RC, Meyers BF, Guthrie TJ, Roper CL, Cooper JD, et al. The current role of mediastinoscopy in the evaluation of thoracic disease. J Thorac Cardiovasc Surg. 1999; 118(5):894–899. PMID: 10534695.
Article25. Lemaire A, Nikolic I, Petersen T, Haney JC, Toloza EM, Harpole DH Jr, et al. Nine-year single center experience with cervical mediastinoscopy: complications and false negative rate. Ann Thorac Surg. 2006; 82(4):1185–1189. PMID: 16996905.
Article26. Navani N, Molyneaux PL, Breen RA, Connell DW, Jepson A, Nankivell M, et al. Utility of endobronchial ultrasound-guided transbronchial needle aspiration in patients with tuberculous intrathoracic lymphadenopathy: a multicentre study. Thorax. 2011; 66(10):889–893. PMID: 21813622.
Article27. Sun J, Teng J, Yang H, Li Z, Zhang J, Zhao H, et al. Endobronchial ultrasound-guided transbronchial needle aspiration in diagnosing intrathoracic tuberculosis. Ann Thorac Surg. 2013; 96(6):2021–2027. PMID: 24035300.
Article28. Lucey O, Potter J, Ricketts W, Castle L, Melzer M. Utility of EBUS-TBNA in diagnosing mediastinal tuberculous lymphadenitis in East London. J Infect. 2022; 84(1):17–23. PMID: 34706281.
Article29. Dobler CC, Cheung K, Nguyen J, Martin A. Risk of tuberculosis in patients with solid cancers and haematological malignancies: a systematic review and meta-analysis. Eur Respir J. 2017; 50(2):1700157. PMID: 28838977.
Article30. Fontanilla JM, Barnes A, von Reyn CF. Current diagnosis and management of peripheral tuberculous lymphadenitis. Clin Infect Dis. 2011; 53(6):555–562. PMID: 21865192.
Article31. Mathiasen VD, Eiset AH, Andersen PH, Wejse C, Lillebaek T. Epidemiology of tuberculous lymphadenitis in Denmark: a nationwide register-based study. PLoS One. 2019; 14(8):e0221232. PMID: 31415659.
Article32. Rafay MA. Tuberculous lymphadenopathy of superior mediastinum causing vocal cord paralysis. Ann Thorac Surg. 2000; 70(6):2142–2143. PMID: 11156137.
Article33. Xiong L, Mao X, Li C, Liu Z, Zhang Z. Posterior mediastinal tuberculous lymphadenitis with dysphagia as the main symptom: a case report and literature review. J Thorac Dis. 2013; 5(5):E189–E194. PMID: 24255790.34. Sayeed A, Alqurashi EH, Alzanbagi AB, Ghaleb NAB. Tuberculosis presenting as broncho-oesophageal fistula in a young healthy man. BMJ Case Rep. 2017; 2017:bcr2017220821.
Article35. Nie D, Li J, Liu W, Wu Y, Ji M, Wang Y, et al. Esophagomediastinal fistula due to secondary esophageal tuberculosis: report of two cases. J Int Med Res. 2021; 49(7):3000605211023696. PMID: 34256638.
Article36. Barss L, Connors WJ, Fisher D. Chapter 7: extra-pulmonary tuberculosis. Canadian Respir Crit Care Sleep Med. 2022; 6(sup1):87–108.
Article37. Chahed H, Hachicha H, Berriche A, Abdelmalek R, Mediouni A, Kilani B, et al. Paradoxical reaction associated with cervical lymph node tuberculosis: predictive factors and therapeutic management. Int J Infect Dis. 2017; 54:4–7. PMID: 27810522.
Article38. Seol YJ, Park SY, Yu SN, Kim T, Lee EJ, Jeon MH, et al. Is the initial size of tuberculous lymphadenopathy associated with lymph node enlargement during treatment? Infect Chemother. 2017; 49(2):130–134. PMID: 28608659.
Article39. Breen RA, Smith CJ, Cropley I, Johnson MA, Lipman MC. Does immune reconstitution syndrome promote active tuberculosis in patients receiving highly active antiretroviral therapy? AIDS. 2005; 19(11):1201–1206. PMID: 15990574.
Article40. Narita M, Ashkin D, Hollender ES, Pitchenik AE. Paradoxical worsening of tuberculosis following antiretroviral therapy in patients with AIDS. Am J Respir Crit Care Med. 1998; 158(1):157–161. PMID: 9655723.
Article41. Cheng VC, Yam WC, Woo PC, Lau SK, Hung IF, Wong SP, et al. Risk factors for development of paradoxical response during antituberculosis therapy in HIV-negative patients. Eur J Clin Microbiol Infect Dis. 2003; 22(10):597–602. PMID: 14508660.
Article42. Jeon K, Choi WI, An JS, Lim SY, Kim WJ, Park GM, et al. Paradoxical response in HIV-negative patients with pleural tuberculosis: a retrospective multicentre study. Int J Tuberc Lung Dis. 2012; 16(6):846–851. PMID: 22507441.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Severe Paradoxical Reaction Requiring Tracheostomy in a Human Immunodeficiency Virus (HIV)-negative Patient with Cervical Lymph Node Tuberculosis
- Paradoxical response as a cervical lymph node enlargement after termination of anti-tuberculosis treatment in a patient with pulmonary tuberculosis
- Noninvasive Diagnosis of Mediastinal Metastasis of Lung Cancer
- A Case of Eosinophilic Granuloma in Lung and Mediastinal Lymph Node
- Video-Assisted Thoracic Surgery Mediastinal Lymph Node Dissection in Lung Cancer Surgery