Korean Circ J.
2023 Dec;53(12):829-839. 10.4070/kcj.2023.0063.
Trends and Outcomes of Type 2 Myocardial Infarction During the COVID-19 Pandemic in the United States
- Affiliations
-
- 1Department of Cardiology, West Virginia University School of Medicine, Morgantown, WV, USA
- 2Department of Internal Medicine, St. Luke’s University Health Network, Bethlehem, PA, USA
- 3University of Texas at Austin, Austin, TX, USA
- 4Department of Internal Medicine, Bassett Healthcare Network, Cooperstown, NY, USA
- 5University of Iowa College of Public Health, Iowa City, IA, USA
- 6Department of Medicine, University of Kansas School of Medicine, Wichita, KS, USA
- 7Department of Internal Medicine, New York Medical College/Landmark Medical Center, Woonsocket, RI, USA
- 8Department of Internal Medicine, Bassett Medical Center, Cooperstown, NY, USA
- 9Department of Cardiology, Stanford University School of Medicine, CA, USA
- KMID: 2548790
- DOI: http://doi.org/10.4070/kcj.2023.0063
Abstract
- Background and Objectives
There is limited data on the impact of type 2 myocardial infarction (T2MI) during the coronavirus disease 2019 (COVID-19) pandemic.
Methods
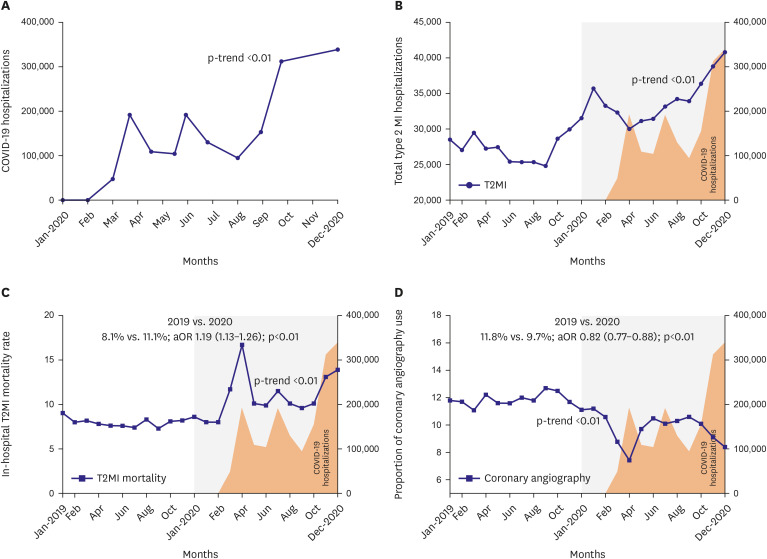
The National Inpatient Sample (NIS) database from January 2019 to December 2020 was queried to identify T2MI hospitalizations based on the appropriate International Classification of Disease, Tenth Revision-Clinical Modification codes. Monthly trends of COVID-19 and T2MI hospitalizations were evaluated using Joinpoint regression analysis. In addition, the multivariate logistic and linear regression analysis was used to compare inhospital mortality, coronary angiography use, and resource utilization between 2019 and 2020.
Results
A total of 743,535 patients hospitalized with a diagnosis of T2MI were identified in the years 2019 (n=331,180) and 2020 (n=412,355). There was an increasing trend in T2MI hospitalizations throughout the study period corresponding to the increase in COVID-19 hospitalizations in 2020. The adjusted odds of in-hospital mortality associated with T2MI hospitalizations were significantly higher in 2020 compared with 2019 (11.1% vs. 8.1%: adjusted odds ratio, 1.19 [1.13–1.26]; p<0.01). In addition, T2MI hospitalizations were associated with lower odds of coronary angiography and higher total hospitalization charges,with no difference in the length of stay in 2020 compared with 2019.
Conclusions
We found a significant increase in T2MI hospitalizations with higher inhospital mortality, total hospitalization costs, and lower coronary angiography use during the early COVID-19 pandemic corresponding to the trends in the rise of COVID-19 hospitalizations. Further research into the factors associated with increased mortality can increase our preparedness for future pandemics.
Figure
Reference
-
1. Cuadros DF, Branscum AJ, Mukandavire Z, Miller FD, MacKinnon N. Dynamics of the COVID-19 epidemic in urban and rural areas in the United States. Ann Epidemiol. 2021; 59:16–20. PMID: 33894385.2. Long B, Brady WJ, Koyfman A, Gottlieb M. Cardiovascular complications in COVID-19. Am J Emerg Med. 2020; 38:1504–1507. PMID: 32317203.3. Clerkin KJ, Fried JA, Raikhelkar J, et al. COVID-19 and cardiovascular disease. Circulation. 2020; 141:1648–1655. PMID: 32200663.4. Di Fusco M, Shea KM, Lin J, et al. Health outcomes and economic burden of hospitalized COVID-19 patients in the United States. J Med Econ. 2021; 24:308–317. PMID: 33555956.5. Talanas G, Dossi F, Parodi G. Type 2 myocardial infarction in patients with coronavirus disease 2019. J Cardiovasc Med (Hagerstown). 2021; 22:603–605. PMID: 33186240.6. Shi S, Qin M, Shen B, et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020; 5:802–810. PMID: 32211816.7. Lala A, Johnson KW, Januzzi JL, et al. Prevalence and impact of myocardial injury in patients hospitalized with COVID-19 infection. J Am Coll Cardiol. 2020; 76:533–546. PMID: 32517963.8. Saaby L, Poulsen TS, Diederichsen AC, et al. Mortality rate in type 2 myocardial infarction: observations from an unselected hospital cohort. Am J Med. 2014; 127:295–302. PMID: 24457000.9. Chapman AR, Shah AS, Lee KK, et al. Long-term outcomes in patients with type 2 myocardial infarction and myocardial injury. Circulation. 2018; 137:1236–1245. PMID: 29150426.10. White K, Kinarivala M, Scott I. Diagnostic features, management and prognosis of type 2 myocardial infarction compared to type 1 myocardial infarction: a systematic review and meta-analysis. BMJ Open. 2022; 12:e055755.11. Sattar Y, Taha A, Patel N, et al. Cardiovascular outcomes of type 2 myocardial infarction among COVID-19 patients: a propensity matched national study. Expert Rev Cardiovasc Ther. 2023; 21:365–371. PMID: 37038300.12. Thygesen K, Alpert JS, Jaffe AS, et al. Fourth Universal Definition of Myocardial Infarction (2018). Circulation. 2018; 138:e618–e651. PMID: 30571511.13. Weber B, Siddiqi H, Zhou G, et al. Relationship between myocardial injury during index hospitalization for SARS-CoV-2 infection and longer-term outcomes. J Am Heart Assoc. 2022; 11:e022010. PMID: 34970914.14. Sandoval Y, Januzzi JL Jr, Jaffe AS. Cardiac troponin for assessment of myocardial injury in COVID-19: JACC review topic of the week. J Am Coll Cardiol. 2020; 76:1244–1258. PMID: 32652195.15. Elyaspour Z, Zibaeenezhad MJ, Razmkhah M, Razeghian-Jahromi I. Is it all about endothelial dysfunction and thrombosis formation? The secret of COVID-19. Clin Appl Thromb Hemost. 2021; 27:10760296211042940. PMID: 34693754.16. Kwok CS, Gale CP, Kinnaird T, et al. Impact of COVID-19 on percutaneous coronary intervention for ST-elevation myocardial infarction. Heart. 2020; 106:1805–1811. PMID: 32868280.17. DeFilippis AP, Chapman AR, Mills NL, et al. Assessment and treatment of patients with type 2 myocardial infarction and acute nonischemic myocardial injury. Circulation. 2019; 140:1661–1678. PMID: 31416350.18. Fox ER, Stolbach AI, Mazer-Amirshahi M. The landscape of prescription drug shortages during the COVID-19 pandemic. J Med Toxicol. 2020; 16:311–313. PMID: 32458230.19. De Luca G, Verdoia M, Cercek M, et al. Impact of COVID-19 pandemic on mechanical reperfusion for patients with STEMI. J Am Coll Cardiol. 2020; 76:2321–2330. PMID: 33183506.20. Sun C, Dyer S, Salvia J, Segal L, Levi R. Worse cardiac arrest outcomes during the COVID-19 pandemic in boston can be attributed to patient reluctance to seek care. Health Aff (Millwood). 2021; 40:886–895. PMID: 34038193.21. Raudenská J, Steinerová V, Javůrková A, et al. Occupational burnout syndrome and post-traumatic stress among healthcare professionals during the novel coronavirus disease 2019 (COVID-19) pandemic. Best Pract Res Clin Anaesthesiol. 2020; 34:553–560. PMID: 33004166.22. Ohsfeldt RL, Choong CK, Mc Collam PL, Abedtash H, Kelton KA, Burge R. Inpatient hospital costs for COVID-19 patients in the United States. Adv Ther. 2021; 38:5557–5595. PMID: 34609704.23. McCarthy CP, Kolte D, Kennedy KF, Vaduganathan M, Wasfy JH, Januzzi JL Jr. Patient characteristics and clinical outcomes of type 1 versus type 2 myocardial infarction. J Am Coll Cardiol. 2021; 77:848–857. PMID: 33602466.24. McCarthy CP, Murphy S, Cohen JA, et al. Underutilization of cardiac rehabilitation for type 2 myocardial infarction. J Am Coll Cardiol. 2019; 73:2005–2007. PMID: 30846342.25. Nazir S, Minhas AM, Kamat IS, et al. Patient characteristics and outcomes of type 2 myocardial infarction during heart failure hospitalizations in the United States. Am J Med. 2021; 134:1371–1379.e2. PMID: 34214459.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Trends in gastrointestinal infections before and during non-pharmaceutical interventions in Korea in comparison with the United States
- Trends and Outcomes of Acute Myocardial Infarction During the Early COVID-19 Pandemic in the United States: A National Inpatient Sample Study
- New York City Vascular Surgeons during the COVID-19 Pandemic
- COVID-19 Vaccination and Herd Immunity
- The Pandemic League of COVID-19: Korea Versus the United States, With Lessons for the Entire World