Int J Thyroidol.
2023 Nov;16(2):190-194. 10.11106/ijt.2023.16.2.190.
A Case of Metastatic Prostate Cancer to the Thyroid Gland with Features of Anaplastic Thyroid Cancer
- Affiliations
-
- 1Departments of Otolaryngology-Head and Neck Surgery, Kosin University College of Medicine, Busan, Korea
- 2Departments of Pathology, Kosin University College of Medicine, Busan, Korea
- KMID: 2548747
- DOI: http://doi.org/10.11106/ijt.2023.16.2.190
Abstract
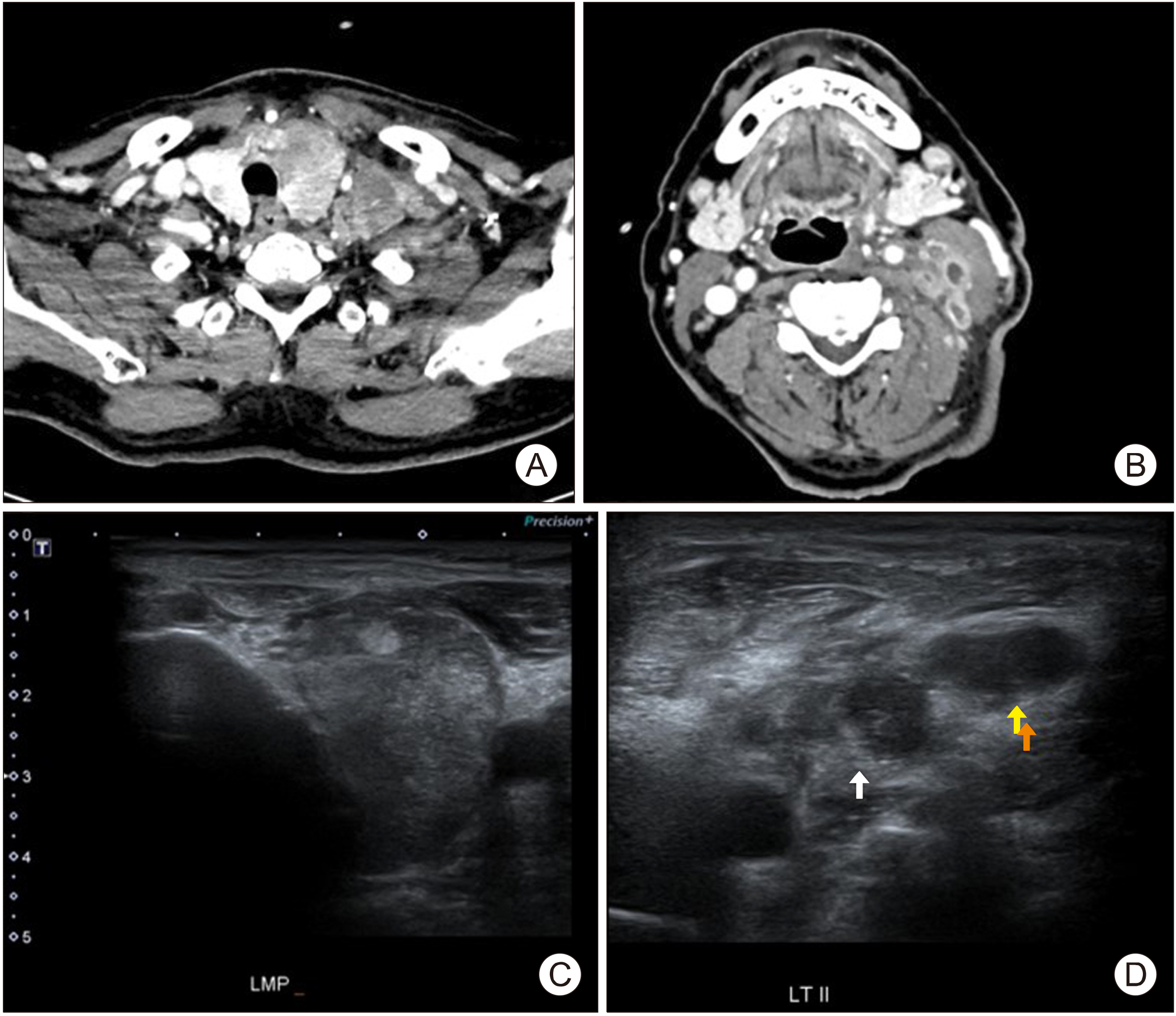
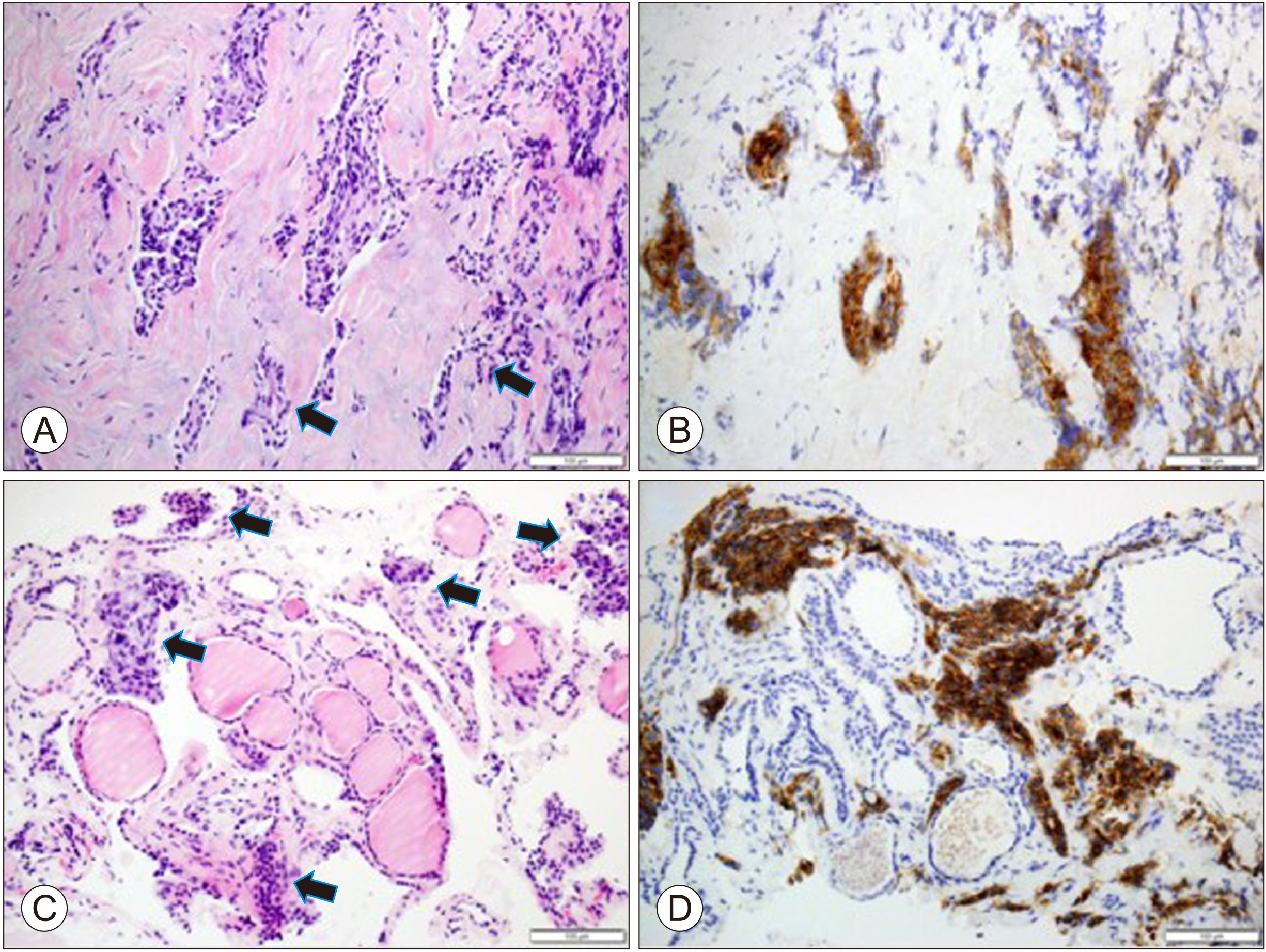
- Prostate cancer is one of the most frequent malignancies in men, and it has metastasis mainly to bones and lungs. Metastasis to cervical region is rare, and thyroid gland is one of the rarest organs with only few reports. In this case, we discuss a rare case of metastatic prostate cancer to thyroid gland and cervical lymph nodes, showing features similar to those of anaplastic thyroid cancer. A 73-year-old man with a history of prostate cancer was referred to our hospital with neck mass suggestive of anaplastic thyroid cancer, detected by fine-needle aspiration. Further examinations, including core needle biopsy, were done and it was confirmed as metastasis of prostate cancer. We focused on shortcomings of fine-needle aspiration and advantages of core-needle biopsy to avoid misdiagnosis. In addition, before diagnosis of head and neck cancer, patient’s history of other carcinomas must always be considered during differential diagnosis of metastatic lesions.
Figure
Reference
-
References
1. Rawla P. 2019; Epidemiology of prostate cancer. World J Oncol. 10(2):63–89. DOI: 10.14740/wjon1191. PMID: 31068988. PMCID: PMC6497009.
Article2. Bubendorf L, Schöpfer A, Wagner U, Sauter G, Moch H, Willi N, et al. 2000; Metastatic patterns of prostate cancer: an autopsy study of 1,589 patients. Hum Pathol. 31(5):578–83. DOI: 10.1053/hp.2000.6698. PMID: 10836297.
Article3. Ljung BM, Drejet A, Chiampi N, Jeffrey J, Goodson WH 3rd, Chew K, et al. 2001; Diagnostic accuracy of fine-needle aspiration biopsy is determined by physician training in sampling technique. Cancer. 93(4):263–8. DOI: 10.1002/cncr.9040. PMID: 11507700.
Article4. Bayram F, Soyuer I, Atmaca H, Demirci D, Gokce C, Canoz O, et al. 2004; Prostatic adenocarcinoma metastasis in the thyroid gland. Endocr J. 51(4):445–8. DOI: 10.1507/endocrj.51.445. PMID: 15351802.
Article5. Ro JY, Guerrieri C, el-Naggar AK, Ordóñez NG, Sorge JG, Ayala AG. 1994; Carcinomas metastatic to follicular adenomas of the thyroid gland. Report of two cases. Arch Pathol Lab Med. 118(5):551–6. PMID: 7514864.6. Selimoglu H, Duran C, Saraydaroglu O, Guclu M, Kiyici S, Ersoy C, et al. 2007; Prostate cancer metastasis to thyroid gland. Tumori. 93(3):292–5. DOI: 10.1177/030089160709300312. PMID: 17679467.
Article7. Gilani SM, Khan M, Barbieri A, Prasad ML. 2021; Anaplastic thyroid carcinoma: diagnostic challenges, histopathologic features and ancillary testing. Diagn Histopathol. 27(6):263–71. DOI: 10.1016/j.mpdhp.2021.03.004.
Article8. Ahmed S, Ghazarian MP, Cabanillas ME, Zafereo ME, Williams MD, Vu T, et al. 2018; Imaging of anaplastic thyroid carcinoma. AJNR Am J Neuroradiol. 39(3):547–51. DOI: 10.3174/ajnr.A5487. PMID: 29242360. PMCID: PMC7655324.
Article9. Pasieka JL. 2003; Anaplastic thyroid cancer. Curr Opin Oncol. 15(1):78–83. DOI: 10.1097/00001622-200301000-00012. PMID: 12490766.
Article10. Ha EJ, Baek JH, Lee JH, Kim JK, Song DE, Kim WB, et al. 2016; Core needle biopsy could reduce diagnostic surgery in patients with anaplastic thyroid cancer or thyroid lymphoma. Eur Radiol. 26(4):1031–6. DOI: 10.1007/s00330-015-3921-y. PMID: 26201291.
Article11. Us-Krašovec M, Golouh R, Auersperg M, Bešič N, Ruparčič-Oblak L. 1996; Anaplastic thyroid carcinoma in fine needle aspirates. Acta Cytol. 40(5):953–8. DOI: 10.1159/000334007. PMID: 8842172.
Article12. Hahn SY, Shin JH, Han BK, Ko EY, Ko ES. 2013; Ultra-sonography-guided core needle biopsy for the thyroid nodule: does the procedure hold any benefit for the diagnosis when fine-needle aspiration cytology analysis shows inconclusive results? Br J Radiol. 86(1025):20130007. DOI: 10.1259/bjr.20130007. PMID: 23564885. PMCID: PMC3635802.
Article13. Kraft M, Laeng H, Schmuziger N, Arnoux A, Gürtler N. 2008; Comparison of ultrasound-guided core-needle biopsy and fine-needle aspiration in the assessment of head and neck lesions. Head Neck. 30(11):1457–63. DOI: 10.1002/hed.20891. PMID: 18798314.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- An Unusual Case of Metastatic Non-Small Cell Lung Cancer Misidentified as Anaplastic Thyroid Cancer
- Anaplastic Transformation of Follicular Thyroid Cancer in the Lung, Liver, Bone, and Adrenal Gland
- Concurrent Primary Carcinoma and Metastatic Lesions of the Thyroid
- A Case of Metastatic Renal Cell Carcinoma to Thyroid Gland Mimicking as Anaplastic Thyroid Carcinoma
- Ultrasonographic Features and the Diagnostic Role of Core Needle Biopsy at Metastatic Breast Cancer in the Thyroid gland: A Case Report