Arch Hand Microsurg.
2023 Dec;28(4):287-295. 10.12790/ahm.23.0025.
Reconstruction of extensive scalp defects of oncologic origin using thoracodorsal artery perforator free flaps
- Affiliations
-
- 1Department of Plastic Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2548601
- DOI: http://doi.org/10.12790/ahm.23.0025
Abstract
- Purpose
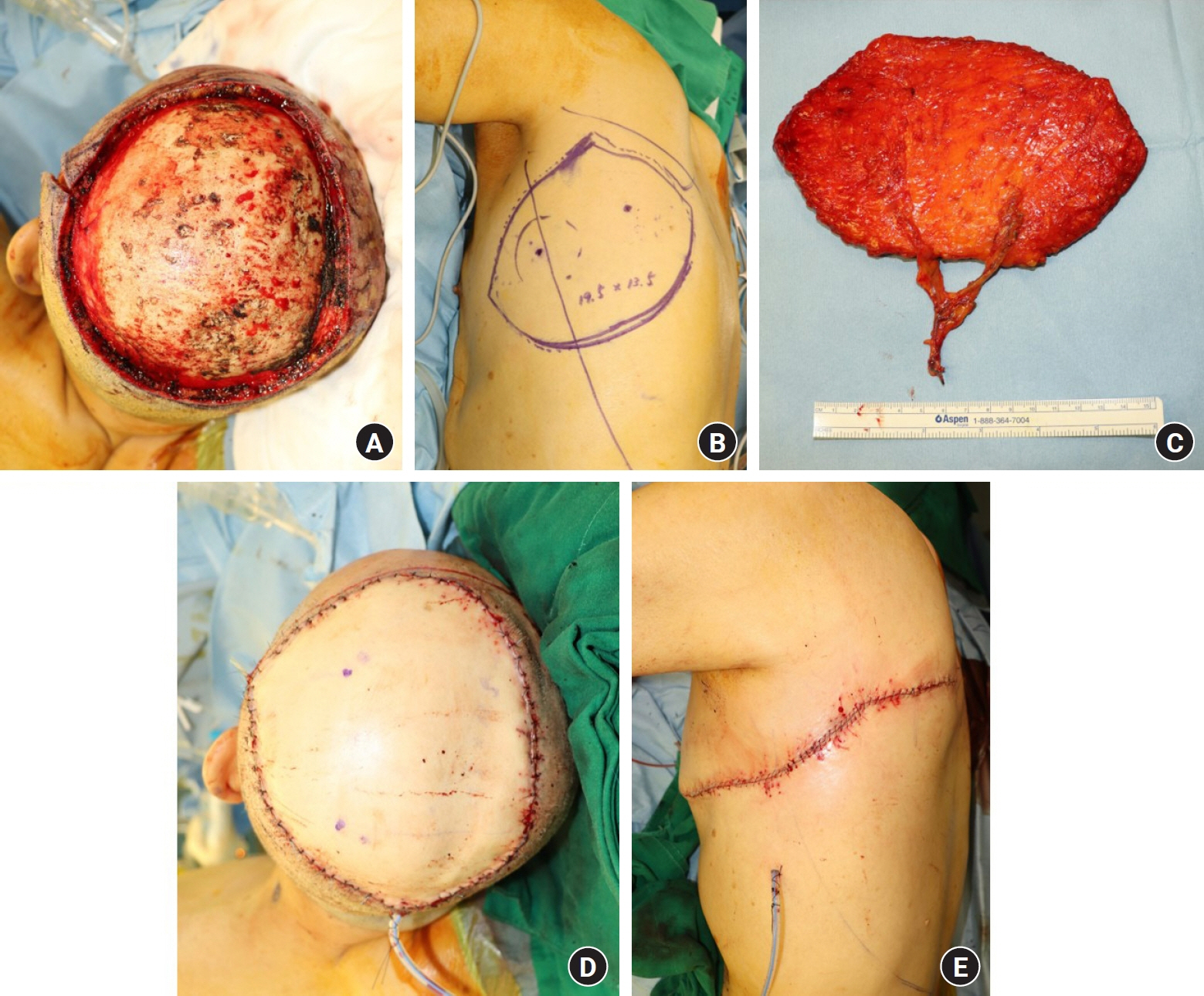
Ablation of malignant neoplasms of the scalp usually leaves extensive defects. Free musculocutaneous transfer using the latissimus dorsi muscle with a skin graft has been the gold standard for restoring such defects; however, this approach may be limited by potential functional morbidity and delayed healing of the grafted skin. This study presents a case series of microsurgical reconstruction with thoracodorsal artery perforator (TDAP) flaps for extensive scalp defects after radical oncologic resection.
Methods
Consecutive patients with malignant scalp tumors who underwent wide local excision and defect coverage with TDAP free flaps between April 2019 and January 2023 were evaluated. Operation-related data and surgical outcomes, including donor- and recipient-site complications, postoperative shoulder function, and aesthetic results, were thoroughly assessed. As an oncologic outcome, local recurrence was also recorded.
Results
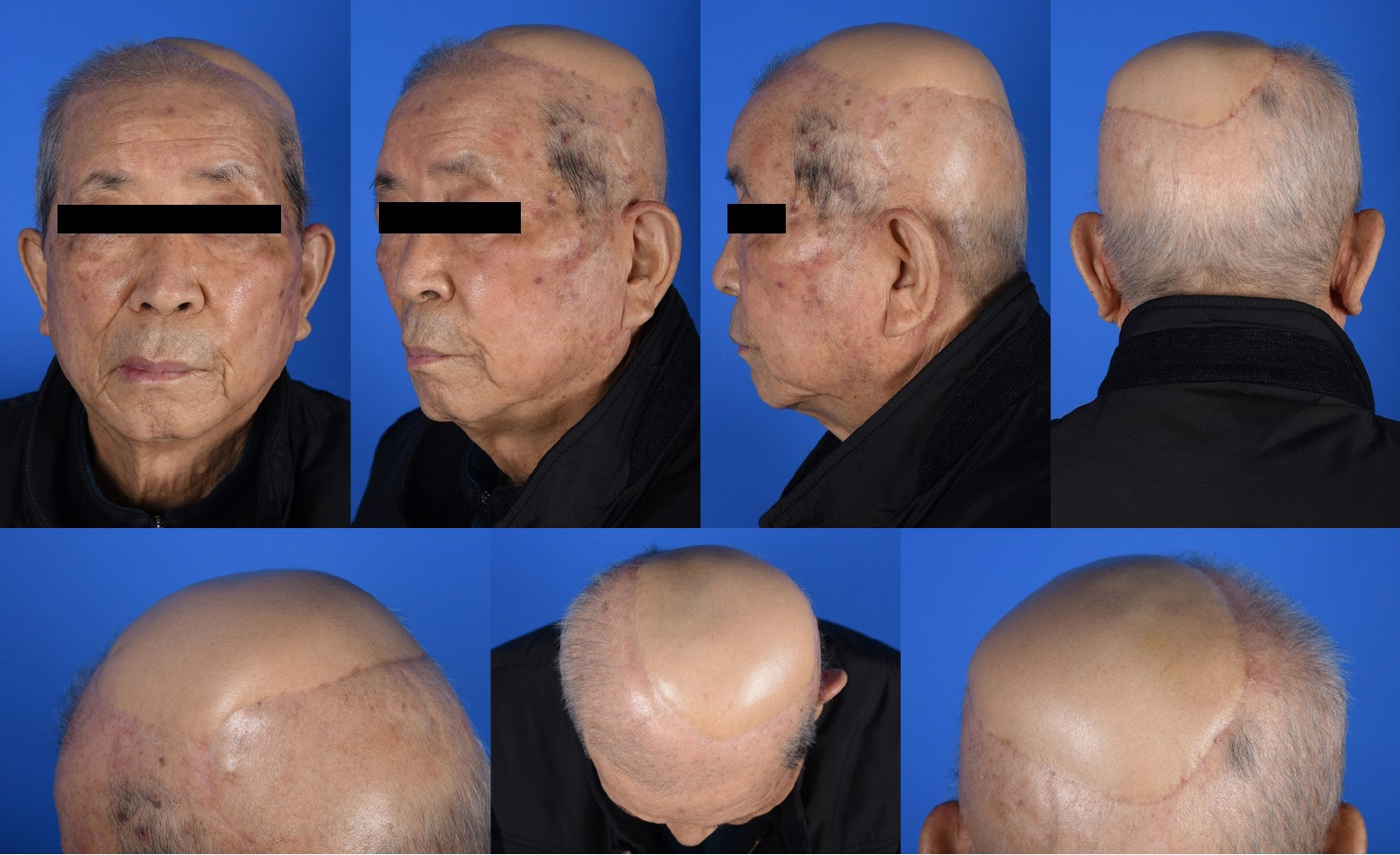
Eleven patients who underwent reconstruction with an average flap size of 223.2 cm2 (range, 160.0–406.0 cm2) were identified. The flaps were based on an average of 2.4 perforators. The donor-site wound was closed primarily in all cases. All flaps achieved complete wound healing within an average of 2 weeks and presented stable resurfacing of the scalp with satisfactory morphological outcomes. No functional shoulder disability was observed in the postoperative period. Five patients exhibited local recurrence but were appropriately treated in a timely manner.
Conclusion
The free TDAP flap could be a potential, effective reconstructive tool for extensive scalp defects of oncologic origin and can overcome the recipient- and donor-site complications associated with the conventional procedure.
Keyword
Figure
Reference
-
References
1. Jang HU, Choi YW. Scalp reconstruction: a 10-year experience. Arch Craniofac Surg. 2020; 21:237–43.
Article2. Newman MI, Hanasono MM, Disa JJ, Cordeiro PG, Mehrara BJ. Scalp reconstruction: a 15-year experience. Ann Plast Surg. 2004; 52:501–6.
Article3. Lim SY, Pyon JK, Mun GH, Bang SI, Oh KS. Surgical treatment of angiosarcoma of the scalp with superficial parotidectomy. Ann Plast Surg. 2010; 64:180–2.
Article4. Alharbi A, Kim YC, AlShomer F, Choi JW. Utility of multimodal treatment protocols in the management of scalp cutaneous angiosarcoma. Plast Reconstr Surg Glob Open. 2023; 11:e4827.
Article5. Chou PY, Kao D, Denadai R, Huang CY, Lin CH, Lin CH. Anterolateral thigh free flaps for the reconstruction of scalp angiosarcoma: 18-year experience in Chang Gung memorial hospital. J Plast Reconstr Aesthet Surg. 2019; 72:1900–8.6. Lutz BS, Wei FC, Chen HC, Lin CH, Wei CY. Reconstruction of scalp defects with free flaps in 30 cases. Br J Plast Surg. 1998; 51:186–90.
Article7. Lee KT, Wiraatmadja ES, Mun GH. Free latissimus dorsi muscle-chimeric thoracodorsal artery perforator flaps for reconstruction of complicated defects: does muscle still have a place in the domain of perforator flaps? Ann Plast Surg. 2015; 74:565–72.8. Oh SJ, Lee J, Cha J, Jeon MK, Koh SH, Chung CH. Free-flap reconstruction of the scalp: donor selection and outcome. J Craniofac Surg. 2011; 22:974–7.9. Chang KP, Lai CH, Chang CH, Lin CL, Lai CS, Lin SD. Free flap options for reconstruction of complicated scalp and calvarial defects: report of a series of cases and literature review. Microsurgery. 2010; 30:13–8.
Article10. Scaglioni MF, Giunta G. Reconstruction of cranioplasty using the thoracodorsal artery perforator (TDAP) flap: a case series. Microsurgery. 2019; 39:207–14.
Article11. Kim SW, Hwang KT, Kim JD, Kim YH. Reconstruction of postinfected scalp defects using latissimus dorsi perforator and myocutaneous free flaps. J Craniofac Surg. 2012; 23:1615–9.
Article12. Choi JH, Ahn KC, Chang H, Minn KW, Jin US, Kim BJ. Surgical treatment and prognosis of angiosarcoma of the scalp: a retrospective analysis of 14 patients in a single institution. Biomed Res Int. 2015; 2015:321896.
Article13. Lipa JE, Butler CE. Enhancing the outcome of free latissimus dorsi muscle flap reconstruction of scalp defects. Head Neck. 2004; 26:46–53.
Article14. Hierner R, van Loon J, Goffin J, van Calenbergh F. Free latissimus dorsi flap transfer for subtotal scalp and cranium defect reconstruction: report of 7 cases. Microsurgery. 2007; 27:425–8.
Article15. Lee KT, Mun GH. A systematic review of functional donor-site morbidity after latissimus dorsi muscle transfer. Plast Reconstr Surg. 2014; 134:303–14.
Article16. Angrigiani C, Grilli D, Siebert J. Latissimus dorsi musculocutaneous flap without muscle. Plast Reconstr Surg. 1995; 96:1608–14.
Article17. Hwang JH, Lim SY, Pyon JK, Bang SI, Oh KS, Mun GH. Reliable harvesting of a large thoracodorsal artery perforator flap with emphasis on perforator number and spacing. Plast Reconstr Surg. 2011; 128:140e–150e.
Article18. Ayhan S, Tuncer S, Demir Y, Kandal S. Thoracodorsal artery perforator flap: a versatile alternative for various soft tissue defects. J Reconstr Microsurg. 2008; 24:285–93.
Article19. Homsy C, Theunissen T, Sadeghi A. The thoracodorsal artery perforator flap: a powerful tool in breast reconstruction. Plast Reconstr Surg. 2022; 150:755–61.
Article20. Shustef E, Kazlouskaya V, Prieto VG, Ivan D, Aung PP. Cutaneous angiosarcoma: a current update. J Clin Pathol. 2017; 70:917–25.
Article21. Brodland DG, Zitelli JA. Surgical margins for excision of primary cutaneous squamous cell carcinoma. J Am Acad Dermatol. 1992; 27:241–8.
Article22. Lee SH, Mun GH. Transverse thoracodorsal artery perforator flaps: experience with 31 free flaps. J Plast Reconstr Aesthet Surg. 2008; 61:372–9.
Article23. Strasser EJ. Application of an objective grading system for the evaluation of cosmetic surgical results. Plast Reconstr Surg. 2002; 109:1733–40.
Article24. Larrañaga J, Rios A, Franciosi E, Mazzaro E, Figari M. Free flap reconstruction for complex scalp and forehead defects with associated full-thickness calvarial bone resections. Craniomaxillofac Trauma Reconstr. 2012; 5:205–12.
Article25. Toia F, D'Arpa S, Brenner E, Melloni C, Moschella F, Cordova A. Segmental anatomy of the vastus lateralis: guidelines for muscle-sparing flap harvest. Plast Reconstr Surg. 2015; 135:185e–98e.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Reconstruction of a Mangled Hand with a Thoracodorsal Artery Perforator Free Flap: A Report of Two Cases
- Reconstruction of the Soft Tissue Defect Using Thoracodorsal Artery Perforator Skin Flap
- Reconstruction of Greater Trochanteric defect using Lumbar Artery Perforator Free Flap: A Case Report
- Soft Tissue Reconstruction of Children's Extremity with Perforator free Flap
- Resurfacing defects from mycobacterial skin and soft tissue infections using thoracodorsal artery perforator free flaps