Ann Rehabil Med.
2023 Oct;47(5):326-336. 10.5535/arm.23108.
Post-Stroke Spastic Movement Disorder and Botulinum Toxin A Therapy: Early Detection And Early Injection
- Affiliations
-
- 1Department of Neurology, Neurorehabilitation Unit, Vivantes Klinikum Spandau, Berlin, Germany
- 2Neurology at Wittenbergplatz, Berlin, Germany
- KMID: 2548392
- DOI: http://doi.org/10.5535/arm.23108
Abstract
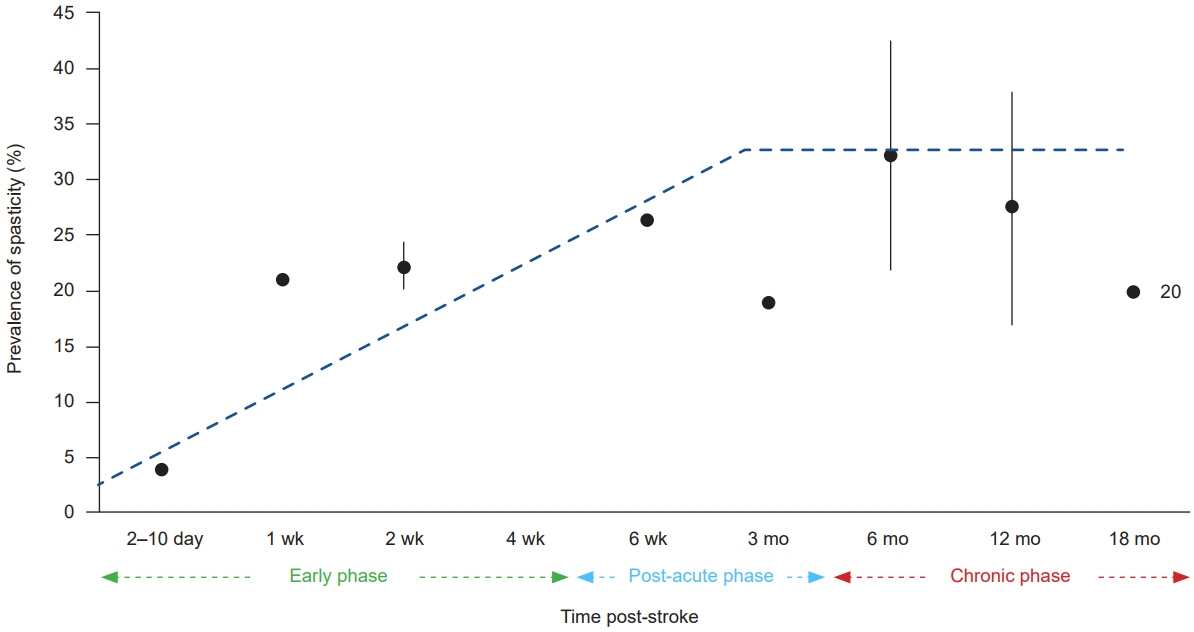
- Post-stroke spastic movement disorder (PS-SMD) develops in up to 40% of stroke survivors after a first ever stroke within the first year. Chronic PS-SMD is often associated with severe disabilities and complications, emphasizing the importance of its early recognition and early adequate management. Extensive research has aimed to accurately predict and sensitively detect a PS-SMD. Symptomatic therapies include conventional rehabilitation and local intramuscular injections of botulinum toxin A (BoNT-A). The latter is widely used, but primarily in the chronic phase of stroke. However, recent studies have shown the safety and efficacy of BoNT-A therapy even in the acute phase and early sub-acute phase after stroke, i.e., within three months post-stroke, leading to an improved long-term outcome in stroke rehabilitation. Local BoNT-A injections evolve as the primary approach in focal, multifocal, and segmental chronic or acute/subacute PS-SMD. Patients at high risk for or manifest PS-SMD should be identified by an early spasticity risk assessment. By doing so, PS-SMD can be integral part of the patient-centered goal-setting process of a multiprofessional spasticity-experienced team. The benefit of an early PS-SMD treatment by BoNT-A should predominate putative degenerative muscle changes due to long-term BoNT-A therapy by far. This, as early treatment effectively avoids complications typically associated with a PS-SMD, i.e., contractures, pain, skin lesions. The management of PS-SMD requires a comprehensive and multidisciplinary approach. Early assessment, patient-centered goal setting, early intervention, and early use of BoNT-A therapy prevents from PS-SMD complications and may improve rehabilitation outcome after stroke.
Keyword
Figure
Cited by 1 articles
-
Early Is Better, Then, How Early and How to Apply: Practical Approach of Botulinum Toxin Injection
Joon-Ho Shin
Ann Rehabil Med. 2023;47(6):439-440. doi: 10.5535/arm.230010.
Reference
-
1. Wissel J, Manack A, Brainin M. Toward an epidemiology of poststroke spasticity. Neurology. 2013; 80(3 Suppl 2):S13–9.
Article2. Wissel J, Ri S. Assessment, goal setting, and botulinum neurotoxin a therapy in the management of post-stroke spastic movement disorder: updated perspectives on best practice. Expert Rev Neurother. 2022; 22:27–42.
Article3. Platz T, Wissel J, Donauer E, Vogel M, Tholen R, Lehmler L. [S2k: treatment of spastic syndromes] [Internet]. Deutsche Gesellschaft für Neurologie. 2018 [cited 2023 Jul 13]. Available from: https://register.awmf.org/assets/guidelines/030-078k_S2k_Therapie_spastisches_Syndrom_2019-06-verlaengert.pdf. German.4. Zeng H, Chen J, Guo Y, Tan S. Prevalence and risk factors for spasticity after stroke: a systematic review and meta-analysis. Front Neurol. 2021; 11:616097.
Article5. Mills PB, Phadke CP, Boulias C, Dukelow SP, Ismail F, McNeil SM, et al. Spasticity management teams, evaluations, and tools: a Canadian cross-sectional survey. Can J Neurol Sci. 2022. doi: 10.1017/cjn.2022.326. [Epub ahead of print].
Article6. Wissel J, Ward AB, Erztgaard P, Bensmail D, Hecht MJ, Lejeune TM, et al. European consensus table on the use of botulinum toxin type A in adult spasticity. J Rehabil Med. 2009; 41:13–25.
Article7. Biering-Sørensen F, Charlifue S, Chen Y, New PW, Noonan V, Post MWM, et al. International Spinal Cord Injury Core Data Set (version 3.0)-including standardization of reporting. Spinal Cord. 2023; 61:65–8.
Article8. Platz T, Vuadens P, Eickhof C, Arnold P, Van Kaick S, Heise K. REPAS, a summary rating scale for resistance to passive movement: item selection, reliability and validity. Disabil Rehabil. 2008; 30:44–53.
Article9. Pandyan AD, Gregoric M, Barnes MP, Wood D, Van Wijck F, Burridge J, et al. Spasticity: clinical perceptions, neurological realities and meaningful measurement. Disabil Rehabil. 2005; 27:2–6.
Article10. Wissel J, Camões-Barbosa A, Carda S, Hoad D, Jacinto J. A practical guide to botulinum neurotoxin treatment of shoulder spasticity 2: injection techniques, outcome measurement scales, and case studies. Front Neurol. 2022; 13:1022549.
Article11. Bernhardt J, Hayward KS, Kwakkel G, Ward NS, Wolf SL, Borschmann K, et al. Agreed definitions and a shared vision for new standards in stroke recovery research: The Stroke Recovery and Rehabilitation Roundtable taskforce. Neurorehabil Neural Repair. 2017; 31:793–9.
Article12. Wissel J, Ri S, Kivi A. Early versus late injections of Botulinumtoxin type A in post-stroke spastic movement disorder: a literature review. Toxicon. 2023; 229:107150.
Article13. Burke D, Wissel J, Donnan GA. Pathophysiology of spasticity in stroke. Neurology. 2013; 80(3 Suppl 2):S20–6.
Article14. Lance JW. The control of muscle tone, reflexes, and movement: Robert Wartenberg Lecture. Neurology. 1980; 30:1303–13.
Article15. Li S, Francisco GE. New insights into the pathophysiology of post-stroke spasticity. Front Hum Neurosci. 2015; 9:192.
Article16. Mukherjee A, Chakravarty A. Spasticity mechanisms - for the clinician. Front Neurol. 2010; 1:149.
Article17. Li S. Spasticity, motor recovery, and neural plasticity after stroke. Front Neurol. 2017; 8:120.
Article18. Toda T, Ishida K, Kiyama H, Yamashita T, Lee S. Down-regulation of KCC2 expression and phosphorylation in motoneurons, and increases the number of in primary afferent projections to motoneurons in mice with post-stroke spasticity. PLoS One. 2014; 9:e114328.
Article19. Chen CL, Tang FT, Chen HC, Chung CY, Wong MK. Brain lesion size and location: effects on motor recovery and functional outcome in stroke patients. Arch Phys Med Rehabil. 2000; 81:447–52.
Article20. Ri S, Kivi A, Urban PP, Wolf T, Wissel J. Site and size of lesion predict post-stroke spasticity: a retrospective magnetic resonance imaging study. J Rehabil Med. 2020; 52:jrm00065.
Article21. Ri S, Glaess-Leistner S, Wissel J. Early brain imaging predictors of post-stroke spasticity. J Rehabil Med. 2021; 53:jrm00169.
Article22. Gracies JM. Pathophysiology of spastic paresis. I: paresis and soft tissue changes. Muscle Nerve. 2005; 31:535–51.
Article23. Baude M, Nielsen JB, Gracies JM. The neurophysiology of deforming spastic paresis: a revised taxonomy. Ann Phys Rehabil Med. 2019; 62:426–30.
Article24. Dietz V. [Clinical treatment of spasticity--spastic movement disorders]. Nervenarzt. 2013; 84:1508–11. German.25. Wissel J, Schelosky LD, Scott J, Christe W, Faiss JH, Mueller J. Early development of spasticity following stroke: a prospective, observational trial. J Neurol. 2010; 257:1067–72.
Article26. Urban PP, Wolf T, Uebele M, Marx JJ, Vogt T, Stoeter P, et al. Occurence and clinical predictors of spasticity after ischemic stroke. Stroke. 2010; 41:2016–20.
Article27. Lundström E, Smits A, Terént A, Borg J. Time-course and determinants of spasticity during the first six months following first-ever stroke. J Rehabil Med. 2010; 42:296–301.
Article28. Picelli A, Tamburin S, Gajofatto F, Zanette G, Praitano M, Saltuari L, et al. Association between severe upper limb spasticity and brain lesion location in stroke patients. Biomed Res Int. 2014; 2014:162754.
Article29. Opheim A, Danielsson A, Alt Murphy M, Persson HC, Sunnerhagen KS. Early prediction of long-term upper limb spasticity after stroke: part of the SALGOT study. Neurology. 2015; 85:873–80.
Article30. Kong KH, Lee J, Chua KS. Occurrence and temporal evolution of upper limb spasticity in stroke patients admitted to a rehabilitation unit. Arch Phys Med Rehabil. 2012; 93:143–8.
Article31. Leathley MJ, Gregson JM, Moore AP, Smith TL, Sharma AK, Watkins CL. Predicting spasticity after stroke in those surviving to 12 months. Clin Rehabil. 2004; 18:438–43.
Article32. Ryu JS, Lee JW, Lee SI, Chun MH. Factors predictive of spasticity and their effects on motor recovery and functional outcomes in stroke patients. Top Stroke Rehabil. 2010; 17:380–8.
Article33. Cheung DK, Climans SA, Black SE, Gao F, Szilagyi GM, Mochizuki G. Lesion characteristics of individuals with upper limb spasticity after stroke. Neurorehabil Neural Repair. 2016; 30:63–70.
Article34. Glaess-Leistner S, Ri SJ, Audebert HJ, Wissel J. Early clinical predictors of post-stroke spasticity. Top Stroke Rehabil. 2021; 28:508–18.35. Wissel J, Verrier M, Simpson DM, Charles D, Guinto P, Papapetropoulos S, et al. Post-stroke spasticity: predictors of early development and considerations for therapeutic intervention. PM R. 2015; 7:60–7.
Article36. Bavikatte G, Subramanian G, Ashford S, Allison R, Hicklin D. Early identification, intervention and management of post-stroke spasticity: expert consensus recommendations. J Cent Nerv Syst Dis. 2021; 13:11795735211036576.
Article37. Glaess-Leistner S, Ri SJ, Audebert HJ, Wissel J. Early clinical predictors of post stroke spasticity. Top Stroke Rehabil. 2021; 28:508–18.
Article38. Jacinto J, Camões-Barbosa A, Carda S, Hoad D, Wissel J. A practical guide to botulinum neurotoxin treatment of shoulder spasticity 1: anatomy, physiology, and goal setting. Front Neurol. 2022; 13:1004629.
Article39. Turner-Stokes L, Baguley IJ, De Graaff S, Katrak P, Davies L, McCrory P, et al. Goal attainment scaling in the evaluation of treatment of upper limb spasticity with botulinum toxin: a secondary analysis from a double-blind placebo-controlled randomized clinical trial. J Rehabil Med. 2010; 42:81–9.
Article40. Esquenazi A, Brashear A, Deltombe T, Rudzinska-Bar M, Krawczyk M, Skoromets A, et al. The effect of repeated abobotulinumtoxinA (Dysport®) injections on walking velocity in persons with spastic hemiparesis caused by stroke or traumatic brain injury. PM R. 2021; 13:488–95.41. Kivi A, Ri S, Wissel J. What clinicians and patients want: the past, the presence, and the future of the botulinum toxins. Toxicon. 2020; 177:46–51.
Article42. Rosales RL, Efendy F, Teleg ES, Delos Santos MM, Rosales MC, Ostrea M, et al. Botulinum toxin as early intervention for spasticity after stroke or non-progressive brain lesion: a meta-analysis. J Neurol Sci. 2016; 371:6–14.
Article43. Varvarousis DN, Martzivanou C, Dimopoulos D, Dimakopoulos G, Vasileiadis GI, Ploumis A. The effectiveness of botulinum toxin on spasticity and gait of hemiplegic patients after stroke: a systematic review and meta-analysis. Toxicon. 2021; 203:74–84.
Article44. Fheodoroff K, Scheschonka A, Wissel J. Goal analysis in patients with limb spasticity treated with incobotulinumtoxinA in the TOWER study. Disabil Rehabil. 2022; 44:1367–73.
Article45. Karri J, Mas MF, Francisco GE, Li S. Practice patterns for spasticity management with phenol neurolysis. J Rehabil Med. 2017; 49:482–8.
Article46. Creamer M, Cloud G, Kossmehl P, Yochelson M, Francisco GE, Ward AB, et al. Intrathecal baclofen therapy versus conventional medical management for severe poststroke spasticity: results from a multicentre, randomised, controlled, open-label trial (SISTERS). J Neurol Neurosurg Psychiatry. 2018; 89:642–50.
Article47. Lindsay C, Ispoglou S, Helliwell B, Hicklin D, Sturman S, Pandyan A. Can the early use of botulinum toxin in post stroke spasticity reduce contracture development? A randomised controlled trial. Clin Rehabil. 2021; 35:399–409.
Article48. Nielsen JB, Christensen MS, Farmer SF, Lorentzen J. Spastic movement disorder: should we forget hyperexcitable stretch reflexes and start talking about inappropriate prediction of sensory consequences of movement? Exp Brain Res. 2020; 238:1627–36.
Article49. Fortuna R, Vaz MA, Youssef AR, Longino D, Herzog W. Changes in contractile properties of muscles receiving repeat injections of botulinum toxin (Botox). J Biomech. 2011; 44:39–44.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Botulinum Toxin A Treatment for the Improvement of Hand Function in Spastic Hemiplegia
- Effects of Botulinum Toxin A Treatment in Cerebral Palsy
- Botulinum Toxin Injection for Achalasia and Non-achalasia Esophageal Motility Disorders
- Improvement of Lingual Dystonia Following Cerebellar Infarction through Botulinum Toxin Injection: a Case Report
- A Case of Palatal Myoclonus Tinnitus Treated with Botolinum Toxin Injection