J Yeungnam Med Sci.
2023 Nov;40(Suppl):S1-S8. 10.12701/jyms.2023.00080.
Cytotoxicity of dental self-curing resin for a temporary crown: an in vitro study
- Affiliations
-
- 1Department of Dental Technology, Daegu Health College, Daegu, Korea
- 2Department of Public Health, Graduate School of Environment and Public Health Studies, Yeungnam University, Daegu, Korea
- 3Department of Occupational and Environmental Medicine, Yeungnam University Hospital, Daegu, Korea
- 4Department of Preventive Medicine and Public Health, Yeungnam University College of Medicine, Daegu, Korea
- 5Department of Dentistry, Yeungnam University College of Medicine, Daegu, Korea
- KMID: 2548336
- DOI: http://doi.org/10.12701/jyms.2023.00080
Abstract
- Background
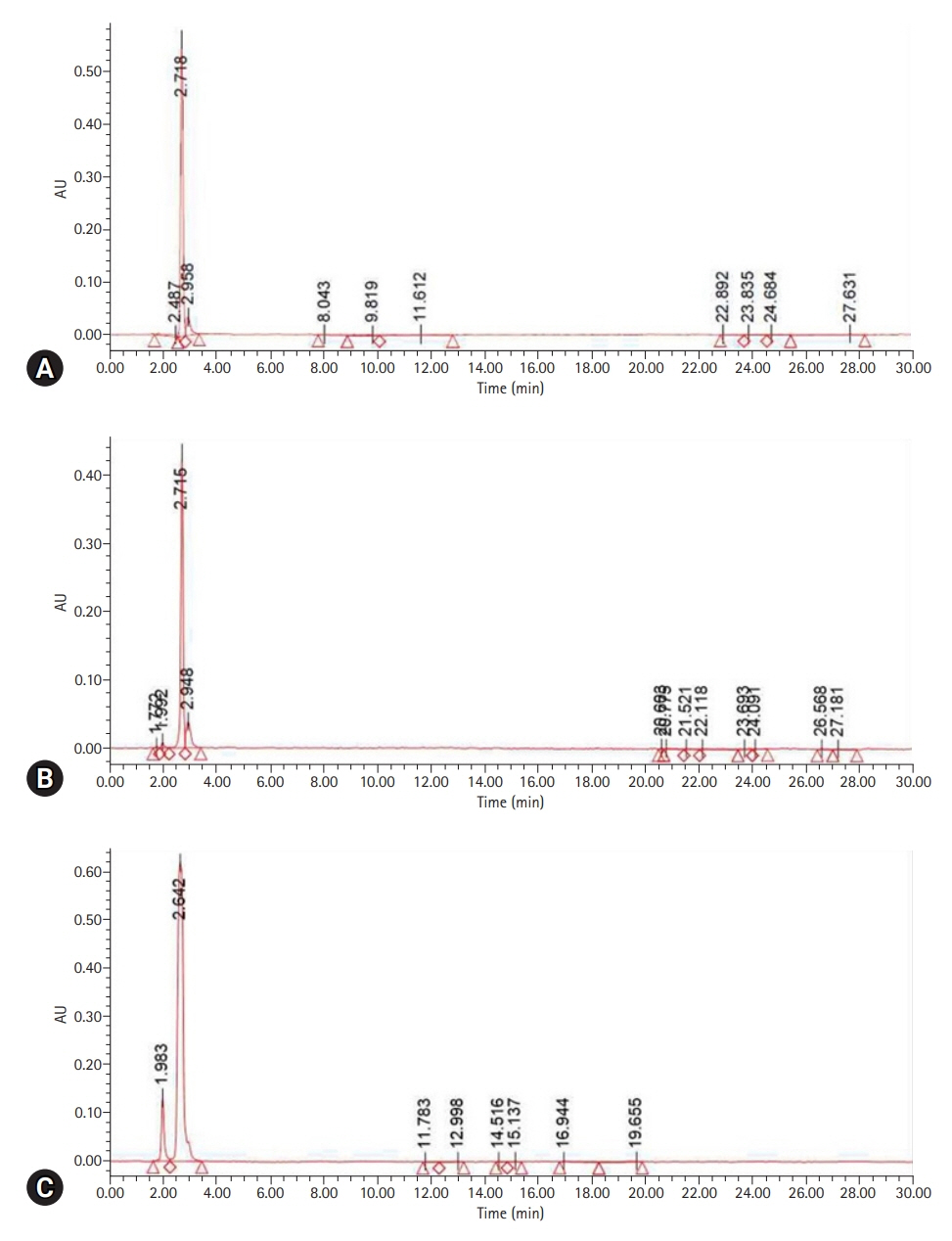
Residual monomer tests using high-performance liquid chromatography and cytotoxicity tests were performed to analyze the effect on the oral mucosa of a self-curing resin for provisional crown production.
Methods
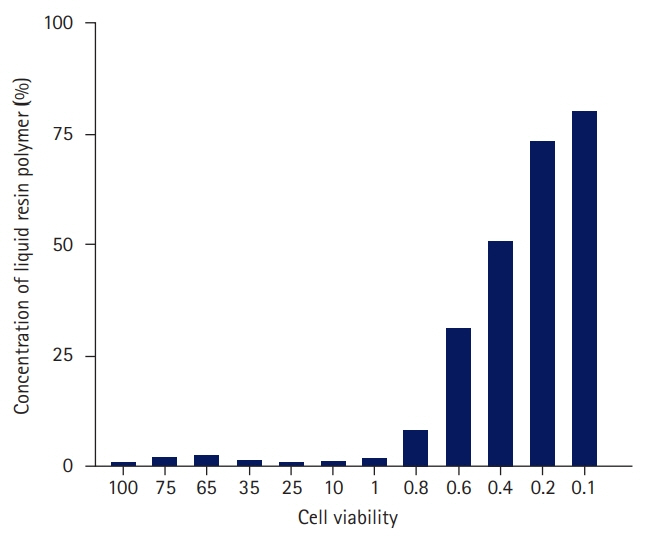
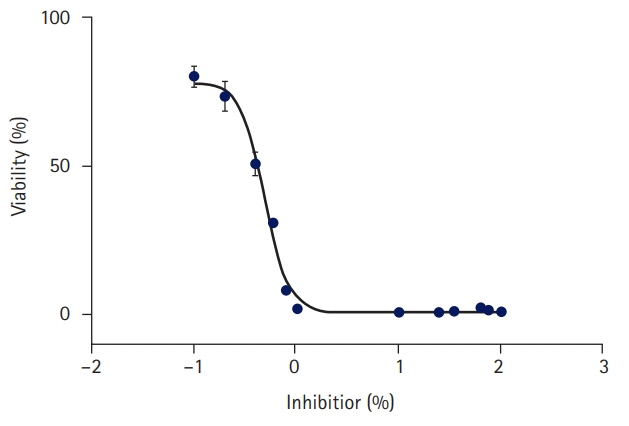
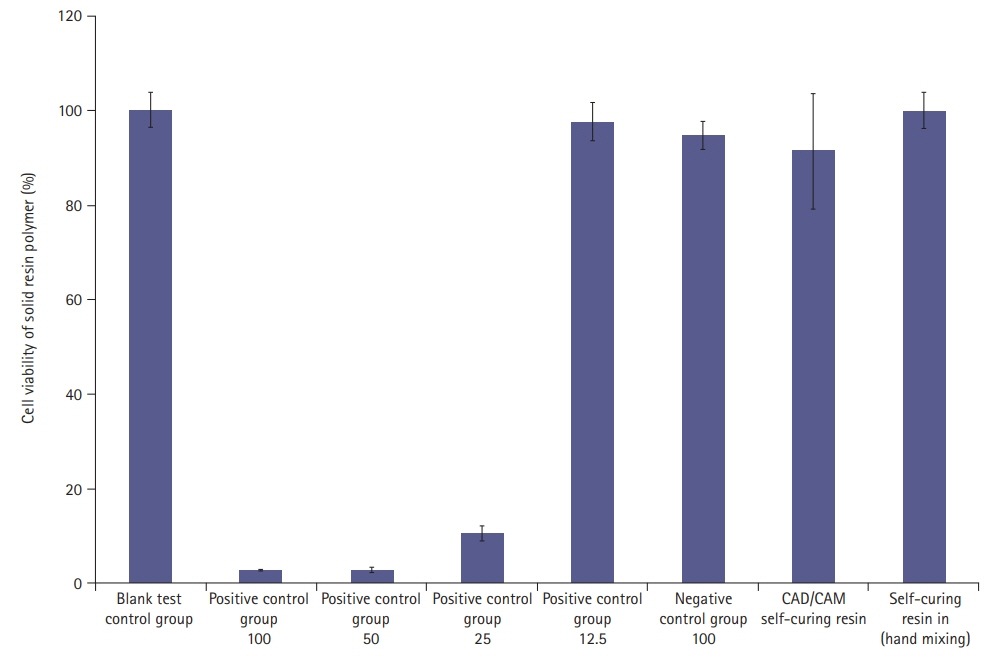
A cytotoxicity test was performed to confirm whether leaked residual monomers directly affected oral mucosal cells. The cytotoxicity of the liquid and solid resin polymers was measured using a water-soluble tetrazolium (WST) test and microplate reader.
Results
In the WST assay using a microplate reader, 73.4% of the cells survived at a concentration of 0.2% liquid resin polymer. The cytotoxicity of the liquid resin polymer was low at ≤0.2%. For the solid resins, when 100% of the eluate was used from each specimen, the average cell viability was 91.3% for the solid resin polymer and 100% for the hand-mixed self-curing resin, which is higher than the cell viability standard of 70%. The cytotoxicity of the solid resin polymer was low.
Conclusion
Because the polymerization process of the self-curing resin may have harmful effects on the oral mucosa during the second and third stages, the solid resin should be manufactured indirectly using a dental model.
Keyword
Figure
Reference
-
References
1. Magne P, Magne M, Belser U. The diagnostic template: a key element to the comprehensive esthetic treatment concept. Int J Periodontics Restorative Dent. 1996; 16:560–9.2. Alpert RL. A method to record optimum anterior guidance for restorative dental treatment. J Prosthet Dent. 1996; 76:546–9.
Article3. Hernandez EP, Oshida Y, Platt JA, Andres CJ, Barco MT, Brown DT. Mechanical properties of four methylmethacrylate-based resins for provisional fixed restorations. Biomed Mater Eng. 2004; 14:107–22.4. Kerby RE, Knobloch LA, Sharples S, Peregrina A. Mechanical properties of urethane and bis-acryl interim resin materials. J Prosthet Dent. 2013; 110:21–8.
Article5. Burns DR, Beck DA, Nelson SK; Committee on Research in Fixed Prosthodontics of the Academy of Fixed Prosthodontics. A review of selected dental literature on contemporary provisional fixed prosthodontic treatment: report of the Committee on Research in Fixed Prosthodontics of the Academy of Fixed Prosthodontics. J Prosthet Dent. 2003; 90:474–97.
Article6. Fondriest JF. Using provisional restorations to improve results in complex aesthetic restorative cases. Pract Proced Aesthet Dent. 2006; 18:217–23.7. Priest G. Esthetic potential of single-implant provisional restorations: selection criteria of available alternatives. J Esthet Restor Dent. 2006; 18:326–38.
Article8. Staehle HJ, Sekundo C. The origins of acrylates and adhesive technologies in dentistry. J Adhes Dent. 2021; 23:397–406.9. Harrison A, Huggett R. Effect of the curing cycle on residual monomer levels of acrylic resin denture base polymers. J Dent. 1992; 20:370–4.
Article10. Abdallah MN, Tran SD, Abughanam G, Laurenti M, Zuanazzi D, Mezour MA, et al. Biomaterial surface proteomic signature determines interaction with epithelial cells. Acta Biomater. 2017; 54:150–63.
Article11. Souto-Lopes M, Azevedo Á, Teixeira A, Bastos-Aires D, Lordelo J, Pérez-Mongiovi D. Cytotoxicity of acrylic-based resin compounds in a human gingival fibroblast cell line. Rev Port Estomatol Med Dent Cir Maxilofac. 2013; 54:87–90.
Article12. Wiegand A, Stucki L, Hoffmann R, Attin T, Stawarczyk B. Repairability of CAD/CAM high-density PMMA- and composite-based polymers. Clin Oral Investig. 2015; 19:2007–13.
Article13. Herráez-Galindo C, Rizo-Gorrita M, Luna-Oliva I, Serrera-Figallo MÁ, Castillo-Oyagüe R, Torres-Lagares D. In vitro comparative study of fibroblastic behaviour on polymethacrylate (PMMA) and lithium disilicate polymer surfaces. Polymers (Basel). 2019; 11:744.
Article14. Lee HJ, Kim CW, Kim YS. The level of residual monomer in injection molded denture base materials. J Korean Acad Prosthodont. 2003; 41:360–8.15. Kedjarune U, Charoenworaluk N, Koontongkaew S. Release of methyl methacrylate from heat-cured and autopolymerized resins: cytotoxicity testing related to residual monomer. Aust Dent J. 1999; 44:25–30.
Article16. Naji A, Harmand MF. Study of the effect of the surface state on the cytocompatibility of a Co-Cr alloy using human osteoblasts and fibroblasts. J Biomed Mater Res. 1990; 24:861–71.
Article17. Arossi GA, Lehmann M, Dihl RR, Reguly ML, de Andrade HH. Induced DNA damage by dental resin monomers in somatic cells. Basic Clin Pharmacol Toxicol. 2010; 106:124–9.
Article18. Gautam R, Singh RD, Sharma VP, Siddhartha R, Chand P, Kumar R. Biocompatibility of polymethylmethacrylate resins used in dentistry. J Biomed Mater Res B Appl Biomater. 2012; 100:1444–50.
Article19. Al-Hiyasat AS, Darmani H, Milhem MM. Cytotoxicity evaluation of dental resin composites and their flowable derivatives. Clin Oral Investig. 2005; 9:21–5.
Article20. Kang S. Mineralization-inducing potentials of calcium silicate-based pulp capping materials in human dental pulp cells. Yeungnam Univ J Med. 2020; 37:217–25.
Article21. Lai YL, Chen YT, Lee SY, Shieh TM, Hung SL. Cytotoxic effects of dental resin liquids on primary gingival fibroblasts and periodontal ligament cells in vitro. J Oral Rehabil. 2004; 31:1165–72.22. Freshney RI. Transformation and immortalization. In : Freshney RI, editor. Culture of animal cells: a manual of basic technique and specialized applications. 6th ed. New Jersey: Wiley-Blackwell;2010. p. 279–97.23. Chaves CA, Machado AL, Carlos IZ, Giampaolo ET, Pavarina AC, Vergani CE. Cytotoxicity of monomers, plasticizer and degradation by-products released from dental hard chairside reline resins. Dent Mater. 2010; 26:1017–23.
Article24. Göpferich A, Schedl L, Langer R. The precipitation of monomers during the erosion of a class of polyanhydrides. Polymer. 1996; 37:3861–9.
Article25. Jorge JH, Giampaolo ET, Machado AL, Vergani CE. Cytotoxicity of denture base acrylic resins: a literature review. J Prosthet Dent. 2003; 90:190–3.
Article26. Trivedi SC, Talim ST. The response of human gingiva to restorative materials. J Prosthet Dent. 1973; 29:73–80.
Article27. Pituru SM, Greabu M, Totan A, Imre M, Pantea M, Spinu T, et al. A review on the biocompatibility of PMMA-based dental materials for interim prosthetic restorations with a glimpse into their modern manufacturing techniques. Materials (Basel). 2020; 13:2894.
Article28. Kim EK, Park EY, Kang S. Three-dimensional printing of temporary crowns with polylactic acid polymer using the fused deposition modeling technique: a case series. J Yeungnam Med Sci. 2023; 40:302–7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Surface Microhardness of the Flowable Bulk-Fill Resin and the Packable Bulk-Fill Resin according to Light Curing Time and Distance
- Color Stability of Self-Cured Temporary Crown Resin according to Different Surface Treatments
- A Study on the Accuracy of the record base of the Complete Denture to the Master Cast according to Kinds of Resin and Polymerization Method
- In Vitro Study on the Bond Strength Between 3D-Printed Resin and Resin Cement for Pediatric Crown Restoration
- Comparison of polymerization shrinkage of dual-cure core build-up resin according to shade and curing mode