J Rhinol.
2023 Nov;30(3):144-148. 10.18787/jr.2023.00054.
Correlation of Upper Lateral Cartilage Collapse and Nasal Septal Deviation
- Affiliations
-
- 1Department of Otorhinolaryngology, Dankook University College of Medicine, Cheonan, Republic of Korea
- 2Department of Otolaryngology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Republic of Korea
- KMID: 2548191
- DOI: http://doi.org/10.18787/jr.2023.00054
Abstract
- Background and Objectives
This study aimed to elucidate the relationship between nasal septal deviation (NSD) and upper lateral cartilage (ULC) collapse.
Methods
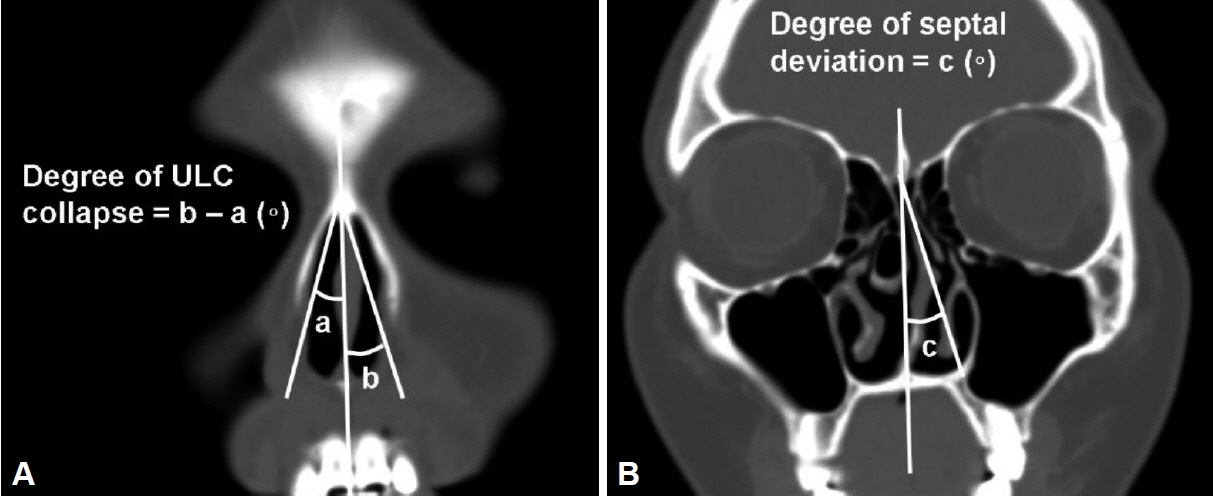
We conducted a retrospective review of 142 paranasal sinus computed tomography scans from patients who had undergone septoplasty due to confirmed NSD. The ULC angle was measured on both the narrow and wide sides of the nasal cavities, and these measurements were compared to evaluate the extent of ULC collapse in relation to the degree of NSD and patient age. The correlation between the degree of NSD and the degree of ULC collapse was also analyzed.
Results
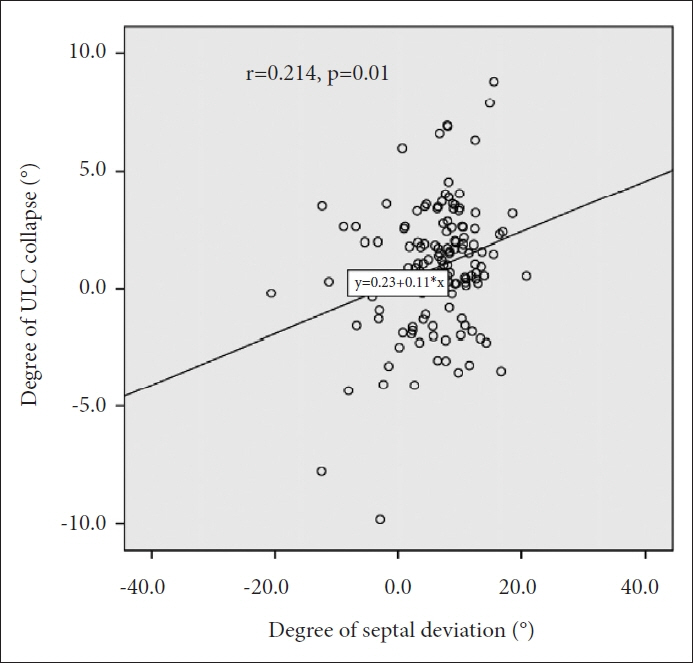
The mean ULC angle was found to be 13.4°±2.7° on the narrow side and 14.3°±2.7° on the wide side, with a statistically significant difference between the two (p<0.001). When comparing caudal and non-caudal NSD patients, there was no significant difference in the degree of ULC on either side (p=0.166). When comparing the ULC angle between two age groups (≥50 vs. <50 years), the difference in ULC angles was significantly greater in the group of patients aged under 50 years (0.3°±3.8° vs. 1.1°±2.2°, p=0.014). There was a significant positive correlation between the degree of ULC collapse and the degree of septal deviation (r=0.214, p=0.01).
Conclusion
NSD was associated with ULC collapse on the narrow side and a narrow internal nasal valve area. This result indicates that clinicians should check for concomitant ULC collapse in patients with NSD.
Figure
Reference
-
References
1. Fuller JC, Levesque PA, Lindsay RW. Assessment of the EuroQol 5-dimension questionnaire for detection of clinically significant global health-related quality-of-life improvement following functional septorhinoplasty. JAMA Facial Plast Surg. 2017; 19(2):95–100.2. Barrett DM, Casanueva FJ, Cook TA. Management of the nasal valve. Facial Plast Surg Clin North Am. 2016; 24(3):219–34.
Article3. Bridger GP. Physiology of the nasal valve. Arch Otolaryngol. 1970; 92(6):543–53.
Article4. Nigro CE, Nigro JF, Mion O, Mello JF Jr. Nasal valve: anatomy and physiology. Braz J Otorhinolaryngol. 2009; 75(2):305–10.
Article5. Wittkopf M, Wittkopf J, Ries WR. The diagnosis and treatment of nasal valve collapse. Curr Opin Otolaryngol Head Neck Surg. 2008; 16(1):10–3.
Article6. Bailey BJ. Head and neck surgery: otolaryngology. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins;1998.7. Lee J, White WM, Constantinides M. Surgical and nonsurgical treatments of the nasal valves. Otolaryngol Clin North Am. 2009; 42(3):495–511.
Article8. Miman MC, Deliktaş H, Ozturan O, Toplu Y, Akarçay M. Internal nasal valve: revisited with objective facts. Otolaryngol Head Neck Surg. 2006; 134(1):41–7.
Article9. Cole P, Chaban R, Naito K, Oprysk D. The obstructive nasal septum. Effect of simulated deviations on nasal airflow resistance. Arch Otolaryngol Head Neck Surg. 1988; 114(4):410–2.
Article10. Hamilton GS 3rd. The external nasal valve. Facial Plast Surg Clin North Am. 2017; 25(2):179–94.
Article11. Khosh MM, Jen A, Honrado C, Pearlman SJ. Nasal valve reconstruction: experience in 53 consecutive patients. Arch Facial Plast Surg. 2004; 6(3):167–71.12. Rhee JS, Weaver EM, Park SS, Baker SR, Hilger PA, Kriet JD, et al. Clinical consensus statement: diagnosis and management of nasal valve compromise. Otolaryngol Head Neck Surg. 2010; 143(1):48–59.
Article13. Aksoy F, Veyseller B, Yildirim YS, Acar H, Demirhan H, Ozturan O. Role of nasal muscles in nasal valve collapse. Otolaryngol Head Neck Surg. 2010; 142(3):365–9.
Article14. Clark DW, Del Signore AG, Raithatha R, Senior BA. Nasal airway obstruction: prevalence and anatomic contributors. Ear Nose Throat J. 2018; 97(6):173–6.
Article15. Most SP. Comparing methods for repair of the external valve: one more step toward a unified view of lateral wall insufficiency. JAMA Facial Plast Surg. 2015; 17(5):345–6.16. O’Neill G, Tolley NS. Theoretical considerations of nasal airflow mechanics and surgical implications. Clin Otolaryngol Allied Sci. 1988; 13(4):273–7.
Article17. Bloom JD, Sridharan S, Hagiwara M, Babb JS, White WM, Constantinides M. Reformatted computed tomography to assess the internal nasal valve and association with physical examination. Arch Facial Plast Surg. 2012; 14(5):331–5.
Article18. Setlur J, Goyal P. Relationship between septal body size and septal deviation. Am J Rhinol Allergy. 2011; 25(6):397–400.
Article19. Wiederkehr I, Kawabata Y, Tsumiyama S, Hosokawa Y, Iimura J, Otori N, et al. Caudal septal deviation: a computed tomography-based evaluation method. Ann Plast Surg. 2022; 89(1):95–9.20. Chen XB, Lee HP, Chong VF, Wang de Y. Assessment of septal deviation effects on nasal air flow: a computational fluid dynamics model. Laryngoscope. 2009; 119(9):1730–6.
Article21. Li L, Zang H, Han D, London NR Jr. Impact of varying types of nasal septal deviation on nasal airflow pattern and warming function: a computational fluid dynamics analysis. Ear Nose Throat J. 2021; 100(6):NP283–9.
Article22. Berger G, Hammel I, Berger R, Avraham S, Ophir D. Histopathology of the inferior turbinate with compensatory hypertrophy in patients with deviated nasal septum. Laryngoscope. 2000; 110(12):2100–5.
Article23. Akoğlu E, Karazincir S, Balci A, Okuyucu S, Sumbas H, Dağli AS. Evaluation of the turbinate hypertrophy by computed tomography in patients with deviated nasal septum. Otolaryngol Head Neck Surg. 2007; 136(3):380–4.
Article24. Yu MS, Choi CH, Jung MS, Kim HC. Correlation between septal body size and inferior turbinate hypertrophy on computerised tomography scans in fifty patients: a radiological analysis. Clin Otolaryngol. 2018; 43(3):952–5.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The functional and cosmetic aspects of alar batten graft
- Using nasal septal cartilage-bone complex for anterior septal reconstruction in Asians
- How to Adjust the Thickness of the Spreader Graft in Nasal Valve Collapse
- Correction of the deviated tip and columella in crooked nose
- Reconstruction of Nasal Septal Deformities by L-Shaped Nasal Septal Cartilage