Restor Dent Endod.
2022 Feb;47(1):e2. 10.5395/rde.2022.47.e2.
How do imaging protocols affect the assessment of root-end fillings?
- Affiliations
-
- 1Department of Restorative Dentistry, São Paulo State University (UNESP), School of Dentistry, Araraquara, SP, Brazil
- 2OMFS IMPATH Research Group, Department of Imaging & Pathology, Faculty of Medicine, KU Leuven and Oral and Maxillofacial Surgery, University Hospitals Leuven, Leuven, Belgium
- 3Department of Dental Medicine, Karolinska Institute, Stockholm, Sweden
- 4Department of Nuclear Energy, Federal University of Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brazil
- KMID: 2548111
- DOI: http://doi.org/10.5395/rde.2022.47.e2
Abstract
Objectives
This study investigated the impact of micro-computed tomography (micro-CT)-based voxel size on the analysis of material/dentin interface voids and thickness of different endodontic cements.
Materials and Methods
Following root-end resection and apical preparation, maxillary premolars were filled with mineral trioxide aggregate (MTA), Biodentine, and intermediate restorative material (IRM) (n = 24). The samples were scanned using micro-CT (SkyScan 1272; Bruker) and the cement/dentin interface and thickness of materials were evaluated at voxel sizes of 5, 10, and 20 µm. Analysis of variance and the Tukey test were conducted, and the degree of agreement between different voxel sizes was evaluated using the Bland and Altman method (p < 0.05).
Results
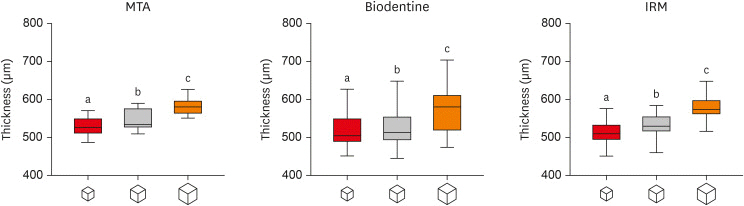
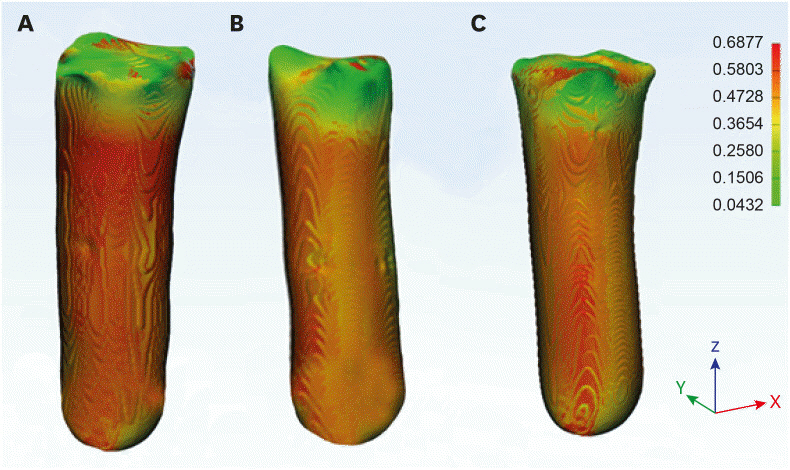
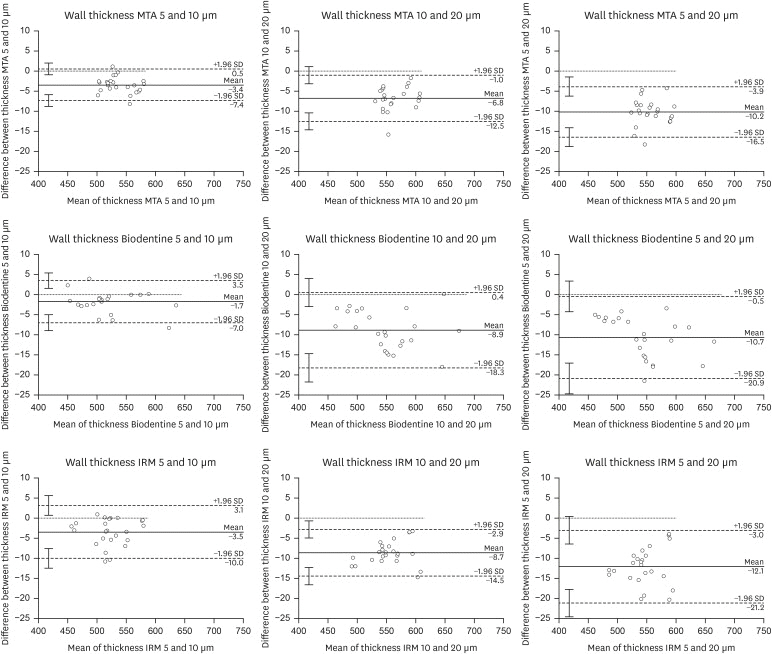
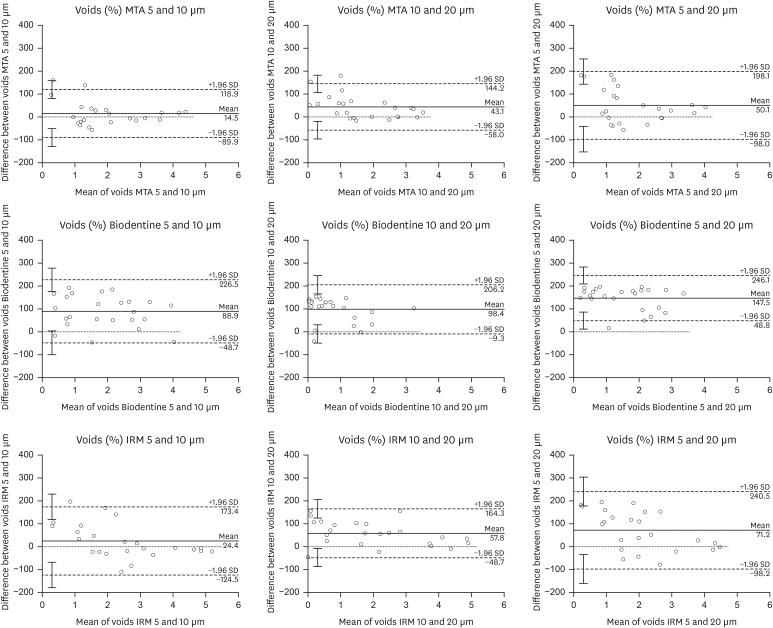
All materials showed an increase in thickness from 5 to 10 and 20 µm (p < 0.05). When evaluating the interface voids, materials were similar at 5 µm (p > 0.05), while at 10 and 20 µm Biodentine showed the lowest percentage of voids (p < 0.05). A decrease in the interface voids was observed for MTA and IRM at 20 µm, while Biodentine showed differences among all voxel sizes (p < 0.05). The Bland-Altman plots for comparisons among voxel sizes showed the largest deviations when comparing images between 5 and 20 µm.
Conclusions
Voxel size had an impact on the micro-CT evaluation of thickness and interface voids of endodontic materials. All cements exhibited an increase in thickness and a decrease in the void percentage as the voxel size increased, especially when evaluating images at 20 µm.
Keyword
Figure
Reference
-
1. Parirokh M, Torabinejad M, Dummer PM. Mineral trioxide aggregate and other bioactive endodontic cements: an updated overview - part I: vital pulp therapy. Int Endod J. 2018; 51:177–205. PMID: 28836288.
Article2. Raina A, Sawhny A, Paul S, Nandamuri S. Comparative evaluation of the bond strength of self-adhering and bulk-fill flowable composites to MTA Plus, Dycal, Biodentine, and TheraCal: an in vitro study. Restor Dent Endod. 2020; 45:e10. PMID: 32110539.
Article3. Torres FF, Jacobs R, EzEldeen M, Guerreiro-Tanomaru JM, Dos Santos BC, Lucas-Oliveira É, Bonagamba TJ, Tanomaru-Filho M. Micro-computed tomography high resolution evaluation of dimensional and morphological changes of 3 root-end filling materials in simulated physiological conditions. J Mater Sci Mater Med. 2020; 31:14. PMID: 31965336.
Article4. Torres FF, Guerreiro-Tanomaru JM, Chavez-Andrade GM, Pinto JC, Berbert FL, Tanomaru-Filho M. Micro-computed tomographic evaluation of the flow and filling ability of endodontic materials using different test models. Restor Dent Endod. 2020; 45:e11. PMID: 32483530.
Article5. Biočanin V, Antonijević Đ, Poštić S, Ilić D, Vuković Z, Milić M, Fan Y, Li Z, Brković B, Đurić M. Marginal gaps between 2 calcium silicate and glass ionomer cements and apical root dentin. J Endod. 2018; 44:816–821. PMID: 29336880.
Article6. Ozlek E, Gündüz H, Akkol E, Neelakantan P. Dentin moisture conditions strongly influence its interactions with bioactive root canal sealers. Restor Dent Endod. 2020; 45:e24. PMID: 32483541.
Article7. Aksel H, Arslan E, Puralı N, Uyanık Ö, Nagaş E. Effect of ultrasonic activation on dentinal tubule penetration of calcium silicate-based cements. Microsc Res Tech. 2019; 82:624–629. PMID: 30614139.
Article8. Karadas M, Atıcı MG. Bond strength and adaptation of pulp capping materials to dentin. Microsc Res Tech. 2020; 83:514–522. PMID: 31912929.
Article9. Kim K, Kim DV, Kim SY, Yang S. A micro-computed tomographic study of remaining filling materials of two bioceramic sealers and epoxy resin sealer after retreatment. Restor Dent Endod. 2019; 44:e18. PMID: 31149616.
Article10. Orhan K, Jacobs R, Celikten B, Huang Y, de Faria Vasconcelos K, Nicolielo LF, Buyuksungur A, Van Dessel J. Evaluation of threshold values for root canal filling voids in micro-CT and nano-CT images. Scanning. 2018; 2018:9437569. PMID: 30116470.
Article11. Yanpiset K, Banomyong D, Chotvorrarak K, Srisatjaluk RL. Bacterial leakage and micro-computed tomography evaluation in round-shaped canals obturated with bioceramic cone and sealer using matched single cone technique. Restor Dent Endod. 2018; 43:e30. PMID: 30135849.
Article12. Gandolfi MG, Parrilli AP, Fini M, Prati C, Dummer PM. 3D micro-CT analysis of the interface voids associated with Thermafil root fillings used with AH Plus or a flowable MTA sealer. Int Endod J. 2013; 46:253–263. PMID: 23039158.
Article13. Almeida LJ, Penha KJ, Souza AF, Lula EC, Magalhães FC, Lima DM, Firoozmand LM. Is there correlation between polymerization shrinkage, gap formation, and void in bulk fill composites? A μCT study. Braz Oral Res. 2017; 31:e100. PMID: 29267661.14. Križnar I, Zanini F, Fidler A. Presentation of gaps around endodontic access cavity restoration by phase contrast-enhanced micro-CT. Clin Oral Investig. 2019; 23:2371–2381.
Article15. Bouxsein ML, Boyd SK, Christiansen BA, Guldberg RE, Jepsen KJ, Müller R. Guidelines for assessment of bone microstructure in rodents using micro-computed tomography. J Bone Miner Res. 2010; 25:1468–1486. PMID: 20533309.
Article16. Maret D, Peters OA, Galibourg A, Dumoncel J, Esclassan R, Kahn JL, Sixou M, Telmon N. Comparison of the accuracy of 3-dimensional cone-beam computed tomography and micro-computed tomography reconstructions by using different voxel sizes. J Endod. 2014; 40:1321–1326. PMID: 25146011.
Article17. Jiřík M, Bartoš M, Tomášek P, Malečková A, Kural T, Horáková J, Lukáš D, Suchý T, Kochová P, Hubálek Kalbáčová M, Králíčková M, Tonar Z. Generating standardized image data for testing and calibrating quantification of volumes, surfaces, lengths, and object counts in fibrous and porous materials using X-ray microtomography. Microsc Res Tech. 2018; 81:551–568. PMID: 29476582.
Article18. Torres FF, Jacobs R, EzEldeen M, de Faria-Vasconcelos K, Guerreiro-Tanomaru JM, Dos Santos BC, Tanomaru-Filho M. How image-processing parameters can influence the assessment of dental materials using micro-CT. Imaging Sci Dent. 2020; 50:161–168. PMID: 32601591.
Article19. EzEldeen M, Van Gorp G, Van Dessel J, Vandermeulen D, Jacobs R; EzEldeen M. 3-dimensional analysis of regenerative endodontic treatment outcome. J Endod. 2015; 41:317–324. PMID: 25498128.
Article20. Giavarina D. Understanding bland altman analysis. Biochem Med (Zagreb). 2015; 25:141–151. PMID: 26110027.21. De Souza ET, Nunes Tameirão MD, Roter JM, De Assis JT, De Almeida Neves A, De-Deus GA. Tridimensional quantitative porosity characterization of three set calcium silicate-based repair cements for endodontic use. Microsc Res Tech. 2013; 76:1093–1098. PMID: 23913667.
Article22. Cooper D, Turinsky A, Sensen C, Hallgrimsson B. Effect of voxel size on 3D micro-CT analysis of cortical bone porosity. Calcif Tissue Int. 2007; 80:211–219. PMID: 17340226.
Article23. Bosmans B, Famaey N, Verhoelst E, Bosmans J, Vander Sloten J. A validated methodology for patient specific computational modeling of self-expandable transcatheter aortic valve implantation. J Biomech. 2016; 49:2824–2830. PMID: 27395760.
Article24. Kim JE, Yi WJ, Heo MS, Lee SS, Choi SC, Huh KH. Three-dimensional evaluation of human jaw bone microarchitecture: correlation between the microarchitectural parameters of cone beam computed tomography and micro-computer tomography. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015; 120:762–770. PMID: 26548728.
Article25. Choi JC, Choi CA, Yeo IL. Spiral scanning imaging and quantitative calculation of the 3-dimensional screw-shaped bone-implant interface on micro-computed tomography. J Periodontal Implant Sci. 2018; 48:202–212. PMID: 30202604.
Article26. Marinozzi F, Bini F, Marinozzi A, Zuppante F, De Paolis A, Pecci R, Bedini R. Technique for bone volume measurement from human femur head samples by classification of micro-CT image histograms. Ann Ist Super Sanita. 2013; 49:300–305. PMID: 24071611.27. Ferretti A, Bellan E, Gava M, Chondrogiannis S, Massaro A, Nibale O, Rubello D. Phantom study of the impact of reconstruction parameters on the detection of mini- and micro-volume lesions with a low-dose PET/CT acquisition protocol. Eur J Radiol. 2012; 81:3363–3370. PMID: 22613508.
Article28. Küçükkaya Eren S, Aksel H, Askerbeyli Örs S, Serper A, Koçak Y, Ocak M, Çelik HH. Obturation quality of calcium silicate-based cements placed with different techniques in teeth with perforating internal root resorption: a micro-computed tomographic study. Clin Oral Investig. 2019; 23:805–811.29. Ozturk TY, Guneser MB, Taschieri S, Maddalone M, Dincer AN, Venino PM, Del Fabbro M. Do the intracanal medicaments affect the marginal adaptation of calcium silicate-based materials to dentin? J Dent Sci. 2019; 14:157–162. PMID: 31210889.
Article30. Küçükkaya Eren S, Görduysus MO, Şahin C. Sealing ability and adaptation of root-end filling materials in cavities prepared with different techniques. Microsc Res Tech. 2017; 80:756–762. PMID: 28271594.
Article31. Kerckhofs G, Schrooten J, Van Cleynenbreugel T, Lomov SV, Wevers M. Validation of x-ray microfocus computed tomography as an imaging tool for porous structures. Rev Sci Instrum. 2008; 79:013711. PMID: 18248043.
Article32. Ber BS, Hatton JF, Stewart GP. Chemical modification of proroot mta to improve handling characteristics and decrease setting time. J Endod. 2007; 33:1231–1234. PMID: 17889696.
Article33. Camilleri J, Sorrentino F, Damidot D. Investigation of the hydration and bioactivity of radiopacified tricalcium silicate cement, Biodentine and MTA Angelus. Dent Mater. 2013; 29:580–593. PMID: 23537569.
Article34. Isaksson H, Töyräs J, Hakulinen M, Aula AS, Tamminen I, Julkunen P, Kröger H, Jurvelin JS. Structural parameters of normal and osteoporotic human trabecular bone are affected differently by microCT image resolution. Osteoporos Int. 2011; 22:167–177. PMID: 20349043.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Determining the reliability of diagnosis and treatment using artificial intelligence software with panoramic radiographs
- Stress Testing and Imaging Protocols for Myocardial Perfusion Studies
- Biocompatibility of root-end filling materials: recent update
- Contact urticaria to bisphenol-A-Diglycidylether dental resin
- Effect of soft chelating irrigation on the sealing ability of GP/AH Plus root fillings